Practice Essentials
Complex regional pain syndrome type 1 (CRPS 1), formerly known as reflex sympathetic dystrophy (RSD), is an incompletely understood response of the body to an external stimulus, resulting in pain that is usually nonanatomic and disproportionate to the inciting event or expected healing response.
Current taxonomy categorizes CRPS 1 as occurring in the absence of definable nerve injury. In many cases, CRPS follows a relatively minor trauma, usually a sprain, twist, dislocation, or soft tissue injury. In some cases, no previous injury was recalled. In children, fractures are the precipitating event in about 5-14% of cases and surgical procedures in about 10-15%. Type II, which was previously caused causalgia, occurs in the presence of nerve trauma. CRPS affects daily function, sleep, and activities of daily living and can have a significant effect on mental and psychosocial well-being. [1, 2, 3, 4, 5, 6, 7, 8, 9, 10]
CRPS 1 is diagnosed on the basis of clinical manifestations, and there are limited laboratory tests or image studies to verify the diagnosis. The International Association for the Study of Pain (IASP) has developed criteria (also known as the Budapest criteria) for the clinical diagnosis of complex regional pain syndrome. [9] Several diagnostic procedures, such as bone scintigraphy, plain radiographs, quantitative sensory testing, skin temperature measurements, and fMRI are used to support the diagnosis of CRPS.
Currently, there are no specific pathologic, histologic, or biochemical markers for CRPS 1. [11, 12, 13, 14, 15, 16] However, there is evidence to show that inflammatory processes and immune reactions are involved in the pathophysiology of CRPS. [17] In a systemic review and meta-analysis, Parkitny et al concluded that CRPS is associated with proinflammatory states in blood, blister fluids, and cerebrospinal fluid. The CRPS-related inflammation may change the sympathetic tone of blood vessels and thereby affect blood supply and tissue oxygenation. The acute and chronic phases of CRPS demonstrate different inflammatory features in both clinical manifestations and inflammatory profiles. [18]
(The radionuclide bone scans below depict patients with CRPS 1.)
 Reflex sympathetic dystrophy of the hand. Delayed image palmar view reveals increased tracer diffusely involving the entire right wrist, metacarpals, and phalanges, with juxta-articular accentuation. Relatively less increased uptake is observed distally, but all areas are involved. The dot of increased activity distal to the third ray is a hot marker indicating the right side.
Reflex sympathetic dystrophy of the hand. Delayed image palmar view reveals increased tracer diffusely involving the entire right wrist, metacarpals, and phalanges, with juxta-articular accentuation. Relatively less increased uptake is observed distally, but all areas are involved. The dot of increased activity distal to the third ray is a hot marker indicating the right side.
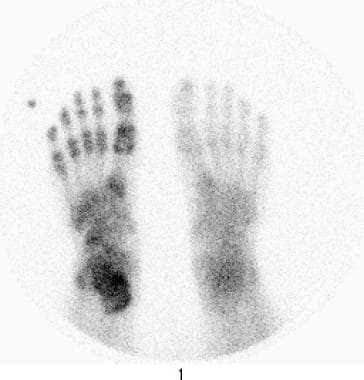 Reflex sympathetic dystrophy of the foot. Delayed image plantar view reveals increased tracer uptake diffusely involving the lowermost right leg, ankle, tarsals, metatarsals, and phalanges. Uptake is less distally than proximally, but all areas are involved. The dot of increased activity distal to fifth toe is a hot marker indicating the right side.
Reflex sympathetic dystrophy of the foot. Delayed image plantar view reveals increased tracer uptake diffusely involving the lowermost right leg, ankle, tarsals, metatarsals, and phalanges. Uptake is less distally than proximally, but all areas are involved. The dot of increased activity distal to fifth toe is a hot marker indicating the right side.
Radiologic examination
Radionuclide bone imaging (RNBI) is the only generally accepted imaging technique to provide objective and relatively specific evidence of CRPS 1 in the upper and lower extremities, predominantly the hands and feet. [19, 20, 21, 22, 23] Delayed bone imaging has been reported to be up to 100% sensitive for the variant of sympathetically maintained pain termed RSD by hand and foot surgeons. [24, 25]
Plain radiography is only 60% sensitive and is not specific; when radiographs are positive, they often show only osteoporosis, occasionally in combination with soft-tissue swelling or diffuse soft-tissue atrophy. Plain radiographs of the affected limb can rule out any localized pathology to the bones, joints, and surrounding tissue. [8]
Although osteoporosis is found in as many as 60% of patients with upper extremity reflex sympathetic dystrophy (RSD), it is not specific, often representing changes of disuse secondary to the pain associated with CRPS 1. Occasionally, soft-tissue swelling or diffuse soft-tissue atrophy may be seen; these are nonspecific findings. No consistent findings have been found in the occasional study done with other imaging modalities, and none are suggested for diagnosis.
Magnetic resonance imaging (MRI) changes in established CRPS 1 have rarely been evaluated, and as with studies using other modalities, the definition of CRPS has varied considerably. In one study by Schweitzer et al involving the lower extremity (N = 35), soft-tissue thickening with and without contrast enhancement (n = 31) was demonstrated without any marrow changes. [26] In another study of the upper extremity (N = 17), by Koch et al, [27] no marrow changes and only inconsistent soft-tissue or muscle signal changes were seen.
Radiography
Below is an imaging example of advanced stage III chronic phase of the disease.
 A 55-year-old female with a chronic history of left foot pain for more than two years and a clinical diagnosis of chronic regional pain syndrome. Radiographic examination of the left foot reveals severe osteopenia, particularly pronounced along the periarticular region (black arrows), while maintaining the integrity of the joint space. Subsequent T1-weighted (B) and STIR (C) MRI images of the same patient exhibit intrinsic plantar muscle atrophy within the foot (white arrow), along with mild edema visible on the STIR images (red arrow). These imaging findings are consistent with the advanced stage III chronic phase of the disease. (Images courtesy of Dr. Muhammad Umer Nasir, MSK Radiology, Queen’s University)
A 55-year-old female with a chronic history of left foot pain for more than two years and a clinical diagnosis of chronic regional pain syndrome. Radiographic examination of the left foot reveals severe osteopenia, particularly pronounced along the periarticular region (black arrows), while maintaining the integrity of the joint space. Subsequent T1-weighted (B) and STIR (C) MRI images of the same patient exhibit intrinsic plantar muscle atrophy within the foot (white arrow), along with mild edema visible on the STIR images (red arrow). These imaging findings are consistent with the advanced stage III chronic phase of the disease. (Images courtesy of Dr. Muhammad Umer Nasir, MSK Radiology, Queen’s University)
Positron Emission Tomography (PET)
Although positron emission tomography (PET) is not typically used to diagnose CRPS, some evidence suggests that this technology could be used as a noninvasive means by which to improve the understanding of the disease’s pathophysiology. Sigma-1 receptor (σ1R), a distinct intracellular protein, is linked to several pathologic conditions afflicting the central nervous system (CNS). This includes CRPS. A study conducted in mice demonstrated that two radioligands, especially [11C]HCC0929, possessed ideal imaging properties and might be valuable tools for noninvasive quantification of σ1R in the brain. [40]
Magnetic Resonance Imaging
MRI cannot exclusively be used to diagnose patients with CRPS. Its role in individuals with suspected CRPS is to rule out the possibility of other diagnoses that could explain the patients’ symptoms.
A retrospective health-record search was conducted for patients with suspected CRPS (foot). [41] Fifty patients with initially suspected CRPS were included: 37 female (age, 51 ± 13 y) and 13 male (age, 44 ± 15 y). All patients underwent MRI. Two radiologists assessed skin, bone, and soft-tissue parameters on MRI. The final diagnosis was CRPS (gold standard: Budapest criteria) or non-CRPS. MRI parameters were compared between CRPS patients and non-CRPS patients. No significant differences between the imaging findings in the two groups were demonstrated.
Ultrasonography
Although ultrasonography (US) is not an established technique in the imaging evaluation of CRPS 1, musculoskeletal US can identify myofascial structural lesions and may help distinguish CRPS from neuropathic pain.
In a retrospective observational study, musculoskeletal US results of patients with neuropathic pain (n = 7) were compared to those of patients with CRPS 1 (n = 7). [28] Muscles in patients with CRPS 1 were characterized by a variable and/or global intramuscular structural disruption with loss of muscle bulk. Adjacent muscles coalesced with one another to present a uniform hyperechogenic mass of tissue. Muscle edema was present in some patients. In comparison, muscles affected by neuropathic pain were structurally normal but also showed considerable reduction in bulk.
Infrared Thermography
According to a case report published by Tucker-Bartley et al, infrared thermography may be a valuable diagnostic and management imaging tool for CRPS. [42] The patient in this report, who developed CRPS, catalogued his symptoms by using a digital and infrared thermal imaging diary. Researchers noted that these images were critical in establishing the initial diagnosis of CRPS, monitoring the progression of the disease, and assessing the patient’s response to treatment.
Nuclear Imaging
Three-phase RNBI is performed primarily because the differential diagnosis often includes infection or other lesions for which information about the perfusion to the extremity (phase I) or the relative vascularity of the extremity (phase II) is helpful. [29, 30, 31, 32]
For CRPS 1 of the hand or foot, the hallmark on the radionuclide angiogram (RNA; phase I) is diffuse increased perfusion to the entire extremity, including the distal forearm or leg and, occasionally, reaching the shoulder or hip, even when the inciting lesion is distal.
Similar diffuse increased vascularity, manifested by diffuse increased tracer accumulation on blood pool or tissue-phase images (phase II) is seen. On these images, juxta-articular accentuation may be apparent. RNA findings are abnormal in approximately 40% of patients and blood pool findings in approximately 50%, most often in clinical stage I or II of the disease.
Delayed images demonstrate diffuse increased tracer throughout the hand or foot, including the wrist or ankle, with juxta-articular accentuation and, often, proximal uptake involving the forearm or leg and, occasionally, the shoulder and arm or hip and femur. Activity in the hands or feet usually is more prominent proximally than distally, but the amount of abnormal tracer uptake has not been correlated with clinical severity. Quantification occasionally has been helpful but is not used routinely.
Furthermore, three-phase bone scintigraphy (TBPS) can be useful in diagnosing chronic posttraumatic CRPS. A study that aimed to evaluate the diagnostic performance of TPBS and digital infrared thermography imaging (DITI) in chronic posttraumatic CRPS found that uptake pattern and uptake ratio in blood pool phase on the TPBS were significantly different between CRPS and non-CRPS groups. [43]
(See the images below.)
 Reflex sympathetic dystrophy of the hand. Delayed image palmar view reveals increased tracer diffusely involving the entire right wrist, metacarpals, and phalanges, with juxta-articular accentuation. Relatively less increased uptake is observed distally, but all areas are involved. The dot of increased activity distal to the third ray is a hot marker indicating the right side.
Reflex sympathetic dystrophy of the hand. Delayed image palmar view reveals increased tracer diffusely involving the entire right wrist, metacarpals, and phalanges, with juxta-articular accentuation. Relatively less increased uptake is observed distally, but all areas are involved. The dot of increased activity distal to the third ray is a hot marker indicating the right side.
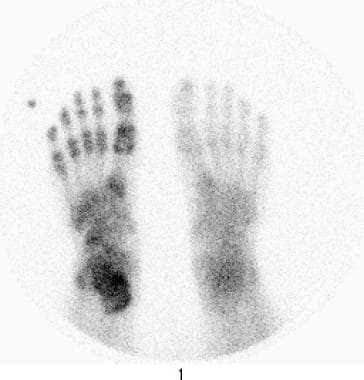 Reflex sympathetic dystrophy of the foot. Delayed image plantar view reveals increased tracer uptake diffusely involving the lowermost right leg, ankle, tarsals, metatarsals, and phalanges. Uptake is less distally than proximally, but all areas are involved. The dot of increased activity distal to fifth toe is a hot marker indicating the right side.
Reflex sympathetic dystrophy of the foot. Delayed image plantar view reveals increased tracer uptake diffusely involving the lowermost right leg, ankle, tarsals, metatarsals, and phalanges. Uptake is less distally than proximally, but all areas are involved. The dot of increased activity distal to fifth toe is a hot marker indicating the right side.
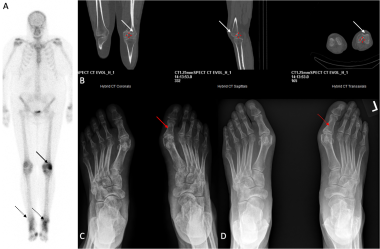 A three-phase bone scan of the lower extremities (A) reveals notable asymmetry and a relative increase in radiotracer uptake in the left lower extremity, particularly prominent within the lateral femoral condyle (black arrow) and the tarsal bones. This increased uptake in tarsal bones is more pronounced on the left side compared to the right (dotted black arrow). Notably, the low-dose SPECT-CT imaging (B) does not show any morphological abnormalities that could account for the elevated uptake in the lateral femoral condyle (white arrow). An anteroposterior (AP) foot radiograph (C) taken prior to the bone scan in 2021 exhibits widespread osteopenia, with a more pronounced distribution around the joints (red arrow). Clinical feature and constellation of the bone scan and radiographic features are consistent with complex regional pain syndrome, stage II dystrophic. Subsequent follow-up AP radiograph in 2023 (post-treatment) displays a resolution of osteopenia (dotted red arrow), coinciding with the alleviation of clinical symptoms. (Images courtesy of Dr. Muhammad Umer Nasir, MSK Radiology, Queen’s University)
A three-phase bone scan of the lower extremities (A) reveals notable asymmetry and a relative increase in radiotracer uptake in the left lower extremity, particularly prominent within the lateral femoral condyle (black arrow) and the tarsal bones. This increased uptake in tarsal bones is more pronounced on the left side compared to the right (dotted black arrow). Notably, the low-dose SPECT-CT imaging (B) does not show any morphological abnormalities that could account for the elevated uptake in the lateral femoral condyle (white arrow). An anteroposterior (AP) foot radiograph (C) taken prior to the bone scan in 2021 exhibits widespread osteopenia, with a more pronounced distribution around the joints (red arrow). Clinical feature and constellation of the bone scan and radiographic features are consistent with complex regional pain syndrome, stage II dystrophic. Subsequent follow-up AP radiograph in 2023 (post-treatment) displays a resolution of osteopenia (dotted red arrow), coinciding with the alleviation of clinical symptoms. (Images courtesy of Dr. Muhammad Umer Nasir, MSK Radiology, Queen’s University)
 A three-phase bone scan of the feet and bone imaging up to the proximal tibias reveal diffuse asymmetrical increased uptake in the affected limb on all three phases, with the left side showing more pronounced uptake (black arrow) than the right. Considering the clinical history, absence of trauma history, and the observed imaging features, the findings are indicative of Complex Regional Pain Syndrome (Stage I, acute) affecting both feet. (Image courtesy of Dr. Muhammad Umer Nasir, MSK Radiology, Queen’s University).
A three-phase bone scan of the feet and bone imaging up to the proximal tibias reveal diffuse asymmetrical increased uptake in the affected limb on all three phases, with the left side showing more pronounced uptake (black arrow) than the right. Considering the clinical history, absence of trauma history, and the observed imaging features, the findings are indicative of Complex Regional Pain Syndrome (Stage I, acute) affecting both feet. (Image courtesy of Dr. Muhammad Umer Nasir, MSK Radiology, Queen’s University).
Pediatricians have reported a moderate frequency of lower-extremity neurovascular or neuroregulatory disease in children that has been termed reflex sympathetic dystrophy (RSD). In these children, a bone scan pattern often reveals marked decreased tracer uptake on delayed images as compared with increased uptake in adults; therefore, this may represent a different condition, such as pseudodystrophy.
When RNBI, especially in the upper extremity, demonstrates classic diffuse findings, RSD is certain. When RNBI does not demonstrate that pattern, the most common variant of sympathetically maintained pain syndrome (SMPS) or CRPS 1 is excluded.
In the lower extremity, patients with severe infection, especially if underlying diabetes mellitus is present, may demonstrate diffuse increased delayed image tracer uptake on RNBI performed to diagnose osteomyelitis. This is not usually a diagnostic issue clinically.
Intervention
CT-assisted temporary thoracic sympathetic nerve blockade
Andresen et al found outpatient computed tomography (CT)-assisted temporary thoracic sympathetic nerve blockade to be an effective adjunct therapy for CRPS, with a low complication rate. [33] In their study, in addition to physiotherapy and pharmacotherapy with analgesics and calcitonin, sympathetic nerve blockade was performed three times, at 2-day intervals. The CT-assisted puncture was performed in the prone position at the level of the T2-T3 intervertebral space. All patients reported immediate pain relief. Color-coded duplex US of the arteries of the affected limb performed before and after the puncture showed increased peripheral blood flow.
Kastler reported using CT-guided radiofrequency neurolysis for treating patients with refractory type I CRPS of the upper limb. [34] Inclusion criteria were clinically based, consisting of the International Association for the Study of Pain (IASP) criteria plus a positive stellate ganglion block. [35]
Ultrasound-guided pulsed radiofrequency
A patient who developed CRPS following injury to the saphenous nerve achieved sustained pain relief after the administration of US-guided pulsed radiofrequency for the management of intractable pain of the lower limb. [36]
Fluoroscopy-guided lumbar sympathetic blocks
In a study by Bovaira et al (N = 27), a series of three fluoroscopy-guided lumbar sympathetic blocks with local anesthetic and corticoids, with infrared thermography used as an intraprocedural support tool, were performed on subjects with lower-extremity CRPS accompanied by severe pain and persistent functional impairment. [44] A responder rate of 37% was noted. Improvements in most of the clinical variables recorded (eg, tingling, edema, perception of thermal asymmetry, difference in coloring, and sweating) were observed. Neuropathic pain was significantly decreased, and functional impairment was reduced.
Photoacoustic Microscopy
It has been suggested that measurement of microcirculatory parameters, such as blood flow rate, blood volume, and oxygen saturation (SO2), with photoacoustic microscopy (PAM) might be useful for diagnosing the presence of CRPS, indicating the activity of the disease, and monitoring the effectiveness of therapeutic intervention.
In a prospective observational study (N = 8) of adult patients with CRPS 1 and pain in one upper extremity who were undergoing stellate ganglion block (SGB), peripheral blood vessels in two sites in patients’ hands were imaged by PAM systems. [37] From pre-SGB to post-SGB, PAM signal intensity increased by 50%, and SO2 increased by 4%, which agreed with the increased temperature and decreased pain level. The results showed that blood perfusion increased after SBG, a finding is consistent with prior reports.
-
Reflex sympathetic dystrophy of the hand. Delayed image palmar view reveals increased tracer diffusely involving the entire right wrist, metacarpals, and phalanges, with juxta-articular accentuation. Relatively less increased uptake is observed distally, but all areas are involved. The dot of increased activity distal to the third ray is a hot marker indicating the right side.
-
Reflex sympathetic dystrophy of the foot. Delayed image plantar view reveals increased tracer uptake diffusely involving the lowermost right leg, ankle, tarsals, metatarsals, and phalanges. Uptake is less distally than proximally, but all areas are involved. The dot of increased activity distal to fifth toe is a hot marker indicating the right side.
-
A 55-year-old female with a chronic history of left foot pain for more than two years and a clinical diagnosis of chronic regional pain syndrome. Radiographic examination of the left foot reveals severe osteopenia, particularly pronounced along the periarticular region (black arrows), while maintaining the integrity of the joint space. Subsequent T1-weighted (B) and STIR (C) MRI images of the same patient exhibit intrinsic plantar muscle atrophy within the foot (white arrow), along with mild edema visible on the STIR images (red arrow). These imaging findings are consistent with the advanced stage III chronic phase of the disease. (Images courtesy of Dr. Muhammad Umer Nasir, MSK Radiology, Queen’s University)
-
A three-phase bone scan of the lower extremities (A) reveals notable asymmetry and a relative increase in radiotracer uptake in the left lower extremity, particularly prominent within the lateral femoral condyle (black arrow) and the tarsal bones. This increased uptake in tarsal bones is more pronounced on the left side compared to the right (dotted black arrow). Notably, the low-dose SPECT-CT imaging (B) does not show any morphological abnormalities that could account for the elevated uptake in the lateral femoral condyle (white arrow). An anteroposterior (AP) foot radiograph (C) taken prior to the bone scan in 2021 exhibits widespread osteopenia, with a more pronounced distribution around the joints (red arrow). Clinical feature and constellation of the bone scan and radiographic features are consistent with complex regional pain syndrome, stage II dystrophic. Subsequent follow-up AP radiograph in 2023 (post-treatment) displays a resolution of osteopenia (dotted red arrow), coinciding with the alleviation of clinical symptoms. (Images courtesy of Dr. Muhammad Umer Nasir, MSK Radiology, Queen’s University)
-
A three-phase bone scan of the feet and bone imaging up to the proximal tibias reveal diffuse asymmetrical increased uptake in the affected limb on all three phases, with the left side showing more pronounced uptake (black arrow) than the right. Considering the clinical history, absence of trauma history, and the observed imaging features, the findings are indicative of Complex Regional Pain Syndrome (Stage I, acute) affecting both feet. (Image courtesy of Dr. Muhammad Umer Nasir, MSK Radiology, Queen’s University).







