Practice Essentials
Pulmonary interstitial emphysema (PIE) is primarily an iatrogenic pulmonary condition of the premature infant with immature lungs. PIE occurs almost exclusively in association with respiratory distress syndrome and mechanical ventilation. [1] Independent risk factors for mechanical ventilation–caused pulmonary interstitial emphysema are higher oxygen during resuscitation and a higher need for surfactant and ventilatory pressures before diagnosis. Although PIE occurs more commonly in neonates, it can also occur in adults. Increased air pressure in the alveoli and the alveolar airspaces can disrupt adjacent lung interstitial tissue and damage lung structure, resulting in linear and cystic spaces that can be complicated with air leaks.The leaked air then collects outside normal air passages and inside the interstitium or bronchovascular complexes. When PIE occurs within 48 hours after birth in a premature infant, it is usually associated with a grave prognosis. [2, 3, 4, 5]
The ventilatory pressure that is used to keep the alveolar ducts open may cause the alveolar duct to rupture (usually at the junction of the bronchiole and alveolar duct); this in turn leads to the escape of air into the pulmonary interstitium, lymphatics, and venous circulation. [6, 7, 8] Differential diagnosis includes cystic adenomatoid malformation, lobar emphysema, diaphragmatic hernia, and bronchogenic cyst. [4]
PIE may be identified with a frontal chest radiograph. Disease progression is assessed with sequential studies. [3, 4, 9] In an ill infant, it may be difficult to differentiate PIE from lucent overdistention of the bronchioles, although overdistended distal airways tend to be round and of uniform diameter, whereas PIE tends to be ovoid in the direction of the bronchovascular bundles. In addition, the lesions of PIE tend to be of different sizes. It is also difficult to differentiate PIE from early bronchopulmonary dysplasia (BPD) with uneven patterns of aeration. Computed tomography (CT) scanning of the chest can be a helpful diagnostic tool if doubt about the diagnosis remains. [3] The presence of subpleural PIE, in which there is an interstitial air collection in the subpleural region of the lungs excluding the bronchovascular bundle, on CT scan suggests single or multiple alveolar rupture(s) as an origin of pneumomediastinal air. [9] A study by Donnelly et al found that 82% of patients with persistent pulmonary interstitial emphysema (14 of 17 patients) had characteristic CT findings (central lines and dots surrounded by radiolucency). [10]
(The development of PIE is shown in the images below.)
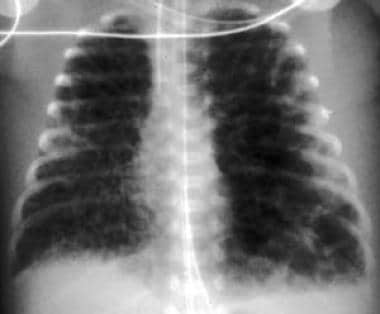
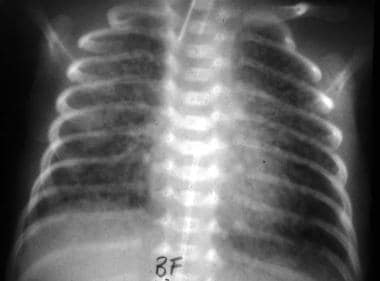
 Anteroposterior examination of the chest at age 1 hour in this 27-week premature infant shows severe diffuse respiratory distress syndrome.
Anteroposterior examination of the chest at age 1 hour in this 27-week premature infant shows severe diffuse respiratory distress syndrome.
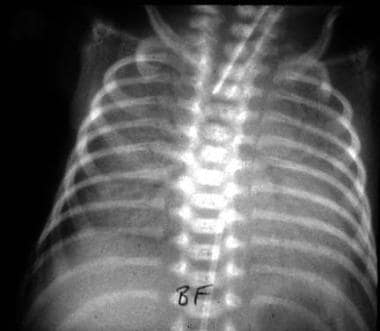
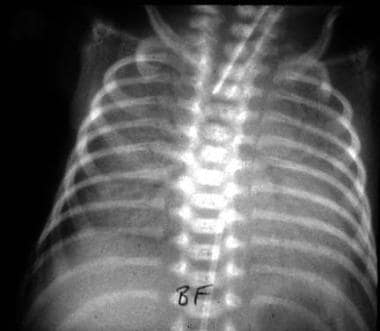
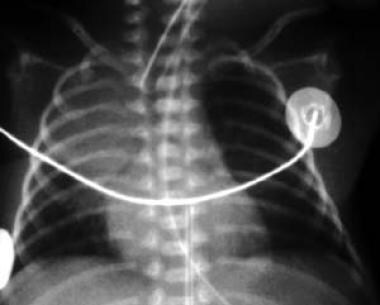
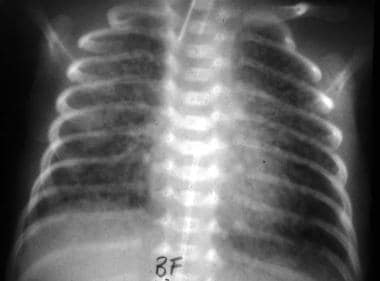 At 7 hours, the lungs are overexpanded with multiple linear areas of lucency, indicating pulmonary interstitial emphysema.
At 7 hours, the lungs are overexpanded with multiple linear areas of lucency, indicating pulmonary interstitial emphysema.
Radiography
On radiography, PIE appears as linear, oval, and occasional spherical cystic air-containing spaces throughout the lung parenchyma. The interstitial changes are initially linear but may become more cystic as the air in the interstitium congregates locally. Subpleural cysts also develop and may rupture, producing a pneumothorax. The heart tends to get smaller as intrathoracic pressure increases; this results in diminished venous return into the chest. Overall lung volume is increased; however, the lungs are less compliant because they are splinted at a large volume by the air within the interstitium. Gas exchange is reduced by the increase in distance between the pulmonary vascular bed and the airspaces.
Linear gas collections in the periphery of the lung, in association with an increased demand for respiratory support, are diagnostic of PIE. Increasing lung volumes also strongly support a diagnosis of PIE. Early bronchopulmonary dysplasia (BPD) may present as focal areas of hyperaeration secondary to partial bronchial obstruction. The pattern closely resembles PIE, although the lucency is less linear in BPD. At histopathology, many lungs of infants with BPD demonstrate PIE that was not seen radiographically.
(The images below show the radiographic characteristics of PIE.)
 Anteroposterior examination of the chest at age 1 hour in this 27-week premature infant shows severe diffuse respiratory distress syndrome.
Anteroposterior examination of the chest at age 1 hour in this 27-week premature infant shows severe diffuse respiratory distress syndrome.
 At 7 hours, the lungs are overexpanded with multiple linear areas of lucency, indicating pulmonary interstitial emphysema.
At 7 hours, the lungs are overexpanded with multiple linear areas of lucency, indicating pulmonary interstitial emphysema.
 Pulmonary interstitial emphysema developing in an infant with respiratory distress syndrome at age 1 day.
Pulmonary interstitial emphysema developing in an infant with respiratory distress syndrome at age 1 day.
 Shortly before death, despite efforts to decrease ventilatory pressures, the lungs remain hyper-aerated with diffuse pulmonary interstitial emphysema.
Shortly before death, despite efforts to decrease ventilatory pressures, the lungs remain hyper-aerated with diffuse pulmonary interstitial emphysema.
 Air in the lymphatics may rupture, causing pneumothorax, and can dissect into the peritoneum through potential openings in the diaphragm. This infant has pulmonary interstitial emphysema, pneumothoraces, and pneumoperitoneum.
Air in the lymphatics may rupture, causing pneumothorax, and can dissect into the peritoneum through potential openings in the diaphragm. This infant has pulmonary interstitial emphysema, pneumothoraces, and pneumoperitoneum.
-
Anteroposterior examination of the chest at age 1 hour in this 27-week premature infant shows severe diffuse respiratory distress syndrome.
-
At 7 hours, the lungs are overexpanded with multiple linear areas of lucency, indicating pulmonary interstitial emphysema.
-
Pulmonary interstitial emphysema developing in an infant with respiratory distress syndrome at age 1 day.
-
By age 2 days, the infant has not improved, and pulmonary interstitial emphysema is more extensive.
-
Close-up examination shows the typical linear pattern of pulmonary interstitial emphysema.
-
Shortly before death, despite efforts to decrease ventilatory pressures, the lungs remain hyper-aerated with diffuse pulmonary interstitial emphysema.
-
The cut section of the lung shows gas dissecting through the interstitium.
-
Histologic section showing gas within the interstitium, mainly in lymphatic vessels. The pulmonary tissue is atelectatic.
-
The surface of the lung in pulmonary interstitial emphysema shows subpleural lymphatics distended with air.
-
Air in the lymphatics may rupture, causing pneumothorax, and can dissect into the peritoneum through potential openings in the diaphragm. This infant has pulmonary interstitial emphysema, pneumothoraces, and pneumoperitoneum.
-
Gas dissects into the interstitium from ruptured airspaces and is rapidly taken up by lymphatics in the interstitium.