Practice Essentials
Pulmonary hypertension, defined as a mean pulmonary arterial pressure (mPAP) of 25 mm Hg or greater at rest measured during right heart catheterization; however, the upper limit of a normal mPAP is considered to be 20 mm Hg. It is often characterized by a progressive and sustained increase in pulmonary vascular resistance that eventually may lead to right ventricular failure and can be a life-threatening condition if left untreated. [1, 2, 3, 4, 5]
Normal pulmonary circulation is a high-flow, low-resistance circuit capable of accommodating the entire right ventricular output at one fifth the pressure of the systemic circulation level. The thin-walled right ventricle functions primarily as a flow-generator pump and is particularly sensitive to increases in its afterload. Increased pulmonary artery pressure and pulmonary vascular resistance characterize pulmonary hypertension.
Pulmonary hypertension is classified into 5 groups by the World Health Organization on the basis of pathophysiology, clinical presentation, and therapeutic options, as follows [6, 1, 2] :
-
Group 1 - Pulmonary arterial hypertension (PAH); mainly related to progressive RV dysfunction as a consequence of progressive pulmonary vasculopathy.
-
Group 2 - Pulmonary hypertension due to left-sided heart disease.
-
Group 3 - Pulmonary hypertension due to lung disease and/or hypoxia.
-
Group 4 - Pulmonary hypertension associated with chronic pulmonary artery obstruction; all patients whose symptoms can be attributed to post-thrombo-embolic fibrotic obstructions within the PA are considered to have chronic thromboembolic pulmonary disease (CTEPD).
-
Group 5 - Pulmonary hypertension with unclear or multifactorial etiologies, including hematologic disorders, systemic disorders, metabolic disorders, chronic renal failure, and other conditions (eg, chronic renal failure, pulmonary tumor thrombotic microangiopathy, fibrosing mediastinitis).
Pulmonary hypertension may be divided into primary and secondary forms. Primary pulmonary hypertension (PPH) is a disease of unknown etiology, whereas secondary pulmonary arterial hypertension (SPAH) is due to either intrinsic parenchymal disease of the lung or disease extrinsic to the lung. [7, 8]
In an individual with suspected pulmonary hypertension, PPH is the diagnosis of exclusion. Hence, a designated algorithm should be used to exclude secondary causes of pulmonary hypertension. The following are proposed investigations [9] :
- Autoantibody tests, HIV test, liver function tests
- Electrocardiography
- Chest radiography
- Pulmonary function tests
- Echocardiography
- Ventilation-perfusion (V/Q) scanning
- Computed tomographic pulmonary angiography (CTPA)
- Pulmonary angiography
- Cardiac catheterization
- Magnetic resonance imaging (MRI)
As a baseline, the first 5 tests are reasonable for substantiating the presence of increased pressures on the right side of the pulmonary vascular system. On the basis of the results, a more focused approach to establish the etiology of the pulmonary hypertension may then involve tests 6-10. Most patients with secondary pulmonary hypertension do not require right heart catheterization before beginning a trial with vasodilators. However, select patients, such as those with collagen vascular disease, should undergo invasive investigations. [8, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21]
The purposes of imaging studies in individuals with pulmonary hypertension are as follows:
-
Detecting pulmonary hypertension (echocardiography, cardiac catheterization)
-
Differentiating the cause (echocardiography, V/Q scanning, CTPA, cardiac catheterization, pulmonary angiography, MRI)
-
Determining the severity (echocardiography, cardiac catheterization)
-
Evaluating the status of the right ventricle (echocardiography, cardiac catheterization, MRI)
Various imaging modalities, including chest radiography, CT, MRI, pulmonary function tests, echocardiography, and angiography, have variable success in detecting the presence and severity of pulmonary hypertension.
Transthoracic echocardiography (TTE) has been the primary method of noninvasive hemodynamic screening and assessment of symptomatic patients, with transesophageal echocardiography (TEE) sometimes required to further evaluate findings from TTE or other imaging modalities. [22]
High resolution computed tomography (HRCT) is the primary imaging modality for assessment of lung parenchyma, and CT pulmonary angiography (CTPA) provides assessment of pulmonary arteries. [22, 3, 23]
MRI is the reference standard for cardiac imaging following medical treatment of PAH and CTEPH. Neither scintigraphy nor CT is is routinely used for follow-up assessment. [24]
Electrocardiograms are useful for demonstrating signs of right ventricular hypertrophy and strain. These signs include the following:
-
Right-axis deviation
-
R/S ratio greater than 1 in lead V1
-
Right atrial enlargement as indicated by an increased P-wave amplitude in lead II
-
Right bundle branch block
PPH is diagnosed if no underlying etiology is found.
(See the images below.)
 Pulmonary hypertension. Chest radiograph in a patient with secondary pulmonary hypertension reveals enlarged pulmonary arteries. This patient was found to have an atrial septal defect.
Pulmonary hypertension. Chest radiograph in a patient with secondary pulmonary hypertension reveals enlarged pulmonary arteries. This patient was found to have an atrial septal defect.
 Pulmonary hypertension. Selective left pulmonary arteriogram reveals large central pulmonary arteries and attenuation of the peripheral vessels, without thrombi.
Pulmonary hypertension. Selective left pulmonary arteriogram reveals large central pulmonary arteries and attenuation of the peripheral vessels, without thrombi.
Radiography
Chest radiographs reveal a number of findings in pulmonary hypertension and may assist in the differential diagnosis of PH by showing signs suggesting lung disease or pulmonary venous congestion due to left heart disease. However, PH cannot be excluded based on a normal radiograph. [6]
Chest radiography may help in distinguishing between arterial and venous PH by respectively demonstrating increased and decreased artery-to-vein ratios. [9]
(See the image below.)
 Pulmonary hypertension. Chest radiograph in a patient with secondary pulmonary hypertension reveals enlarged pulmonary arteries. This patient was found to have an atrial septal defect.
Pulmonary hypertension. Chest radiograph in a patient with secondary pulmonary hypertension reveals enlarged pulmonary arteries. This patient was found to have an atrial septal defect.
Findings in patients with pulmonary artery hypertension (PAH) include central pulmonary arterial dilatation, which contrasts with ‘pruning’ (loss) of the peripheral blood vessels. [9]
A dilated right heart due to right ventricular enlargement is seen as a decrease in the retrosternal space on the lateral image. Right atrial enlargement may be present if significant tricuspid regurgitation is present. This finding may be recognized by the widened right heart border in the frontal projection and enlargement of the right atrial appendage in the lateral projection, which is seen as increased retrosternal opacity above the expected location of the right ventricle.
Peripheral vessel opacity-oligemic lung fields may be observed. This oligemia may be asymmetric. This is also a useful finding suggestive of chronic pulmonary embolism (PE).
An increase in the transverse diameter of the right interlobar artery is indicative of pulmonary hypertension. The upper limit of the transverse diameter of the right interlobar artery from its lateral aspect to the intermediate bronchus is 15 mm in women and 16 mm in men.
The transverse diameter of the left interlobar artery is difficult to appreciate on the posteroanterior (PA) view. Using a lateral view, one can measure from the circular lucency of the left upper lobe bronchus to the posterior margin of the vessel; the upper limit is 18 mm.
Evidence of right atrial dilatation and right ventricular dilatation may be noted.
Kerley B lines may be present. These indicate the presence of pulmonary venous hypertension.
Atrial septal defect is characterized by cardiomegaly, enlargement of the right atrium and ventricle, and enlargement of the central pulmonary arteries. Also present is rapid tapering, with increased vascularity in the periphery of the lung.
Eisenmenger syndrome is characterized by peripheral oligemia, indicating the reversal of a left-to-right shunt due to increased vascular resistance. The peripheral vasculature is diminished, and the cardiac morphology is consistent with cor pulmonale.
Computed Tomography
CT scanning is a useful, noninvasive procedure for confirming the presence of pulmonary hypertension. CT pulmonary angiography (CTPA) is useful in delineating the anatomic detail of the pulmonary vasculature (see the image below). CTPA is the best method for demonstrating emboli. Contrast-enhanced images may show intraluminal abnormalities in the arteries and veins, which are useful for confirming etiologies such as thromboembolic disease. [10, 11, 12, 13, 25, 19, 20, 21, 26, 27]
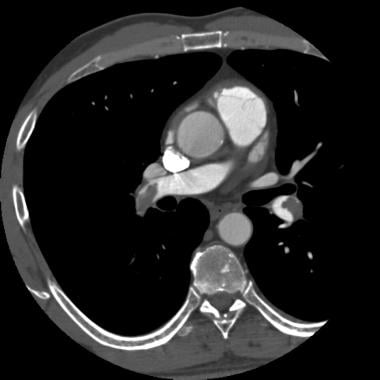 Pulmonary hypertension. CT pulmonary angiogram in a 42-year-old man who experienced severe chest pain after a long flight. Image demonstrates clots in both the right and left main pulmonary arteries.
Pulmonary hypertension. CT pulmonary angiogram in a 42-year-old man who experienced severe chest pain after a long flight. Image demonstrates clots in both the right and left main pulmonary arteries.
Sometimes, if the emboli are large, they may be seen in the pulmonary arteries on routine contrast-enhanced CT scans.
CTPA and, often, conventional pulmonary arteriography are necessary for an adequate evaluation of chronic PE. The technique of CTPA includes a rapid infusion at 3-4 mL/sec for a total of 80-120 mL. Careful review of the images on a workstation is the optimal method of detecting subtle emboli. Evaluation of the lung windows to detect abnormalities of perfusion (mosaic perfusion) is necessary, as occlusions of major pulmonary arterial branches may not be present in a subset of patients with chronic pulmonary thromboembolism.
High-resolution CT (HRCT) scanning of the chest has a role in the evaluation of pulmonary hypertension in patients with suspected diffuse lung disease (eg, in patients with collagen vascular disease).
The upper limit of normal for the diameter of the pulmonary artery is 28.6 mm. A value greater than 28.6 mm suggests increased pressures in the pulmonary system.
(See the image below.)
 Pulmonary hypertension. Spiral CT scan in a patient with pulmonary hypertension reveals enlarged pulmonary arteries and an absence of thrombosis.
Pulmonary hypertension. Spiral CT scan in a patient with pulmonary hypertension reveals enlarged pulmonary arteries and an absence of thrombosis.
Dual-energy computed tomography (DECT) of the chest provides a combined morphologic and functional analysis of the lung, usually obtained in a single acquisition without extra radiation or injection of extra intravenous iodine contrast. DECT enables the ability to quantitatively characterize the material properties of soft tissues, including the distal pulmonary vasculature. [14] Perfusion measured with DECT has an excellent correlation with the perfusion measured with pulmonary scintigraphy. [15]
Magnetic Resonance Imaging
MRI with contrast enhancement allows one to distinguish between the pulmonary vasculature and mediastinal adenopathy. [11, 13, 16, 17, 28]
MRI has capabilities similar to those of echocardiography in the diagnosis and treatment of patients with pulmonary hypertension. MRI is useful for measuring the mass, volume, and overall function of the right ventricle. [14] MRI is also useful for detecting shunt lesions contributing to pulmonary hypertension. Acute and chronic pulmonary thromboembolic disease can be confirmed by using this imaging modality. [29]
The disadvantages with MRI include limitations in individuals with cardiac pacemakers and defibrillators, limited availability, high cost, and difficulty in assessing estimate PA pressures.
Echocardiology
Two-dimensional (2D) Doppler echocardiography remains the most commonly used imaging modality for cardiac and hemodynamic evaluation in PH. However, while echocardiography can assist in determining whether left heart disease or congenital heart disease is the cause of PH, several other causes of PH (eg, lung disease, chronic thromboembolic disease) require additional imaging modalities. [14, 30]
In evaluating pulmonary hypertension, echocardiography can be used to identify secondary causes, such as congenital, valvular, and myocardial disease. In addition, one may estimate pulmonary artery systolic pressure with this method. [31]
The following findings for pulmonary hypertension are confirmed on echocardiography: (1) right atrial and ventricular enlargement and (2) paradoxical movement of the interventricular septum and tricuspid regurgitation. (If right ventricular end-diastolic pressures are greater than 20 mm Hg, the risk of sudden death is relatively high.)
Doppler echocardiography is the most reliable noninvasive method for estimating pulmonary artery pressure. Tricuspid regurgitation is often present in pulmonary hypertension. It is detected in more than 90% of patients with severe pulmonary hypertension, with a correlation of more than 95% when the pressure is measured by means of catheterization. [18, 32]
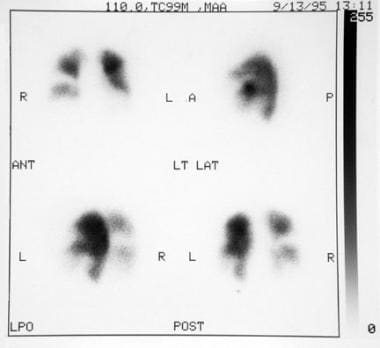
Nuclear Imaging
Radioisotope perfusion lung scanning is performed with intravenous injection of particles of albumin labeled with technetium-99m. As these particles perfuse the lung, the lungs are imaged by using a gamma camera to obtain anterior, posterior, lateral, and oblique views. One would expect a normal distribution of these particles, which produce 2 blackened lung-shaped shadows.
In primary pulmonary hypertension (PPH), the V/Q scan is usually normal.
In secondary pulmonary hypertension due to chronic thromboembolic disease, emboli are responsible for blocking the branches of the pulmonary artery. The lung tissue peripheral to the block is not perfused; this block results in a defect on the scan. When findings in the perfusion scan are abnormal, a ventilation scan is obtained next by using inhalational radioactive xenon-133. A number of lung diseases, including pneumonia and COPD, can cause alterations in the ventilation component, whereas uncomplicated PE does not. Thus, a patient with a high likelihood of PE has an abnormal perfusion scan with a normal ventilation component. (See the image below.)
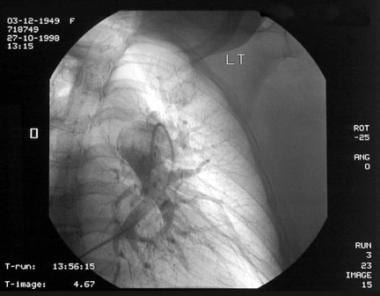
Angiography
Right heart catheterization may be required. Pulmonary angiography is the most accurate modality for evaluating the anatomy and pathophysiology of pulmonary hypertension. This examination is the criterion standard for the diagnosis of pulmonary hypertension. (See the images below.)
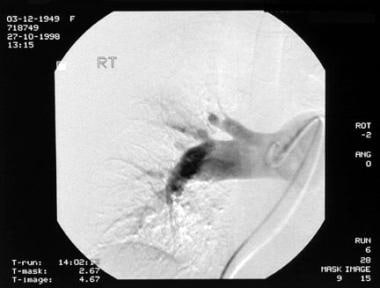 Pulmonary hypertension. Selective right pulmonary arteriogram demonstrates large central pulmonary arteries and attenuation of the peripheral vessels, without any definite demonstrable thrombi.
Pulmonary hypertension. Selective right pulmonary arteriogram demonstrates large central pulmonary arteries and attenuation of the peripheral vessels, without any definite demonstrable thrombi.
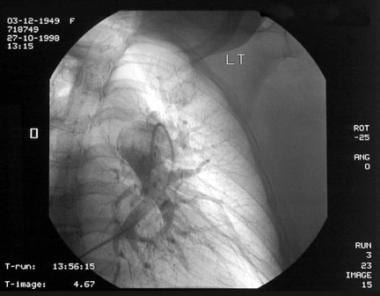 Pulmonary hypertension. Selective left pulmonary arteriogram reveals large central pulmonary arteries and attenuation of the peripheral vessels, without thrombi.
Pulmonary hypertension. Selective left pulmonary arteriogram reveals large central pulmonary arteries and attenuation of the peripheral vessels, without thrombi.
Pulmonary angiography should be performed when the results of V/Q scanning cannot exclude chronic thromboembolic disease as an etiology for the elevated pulmonary pressures. The angiogram reveals large central pulmonary arteries with marked peripheral tapering.
The disadvantage of pulmonary angiography is that it is an invasive procedure, as one cannulates the right side of the heart and the pulmonary artery. Complications include (1) transient rhythm disturbances that respond to the removal of the catheter, (2) cardiac perforation leading to pericardial tamponade, and (3) nephrotoxicity. In patients with an elevated creatinine level (1.5 times normal), the use of high-osmolar contrast material poses a risk of nephrotoxicity. This problem is less commonly seen with the selective use of small amounts of low-osmolar nonionic contrast material. The frequency of complications with pulmonary angiography is limited to less than 5% of cases examined.
-
Pulmonary hypertension. Chest radiograph in a patient with secondary pulmonary hypertension reveals enlarged pulmonary arteries. This patient was found to have an atrial septal defect.
-
Pulmonary hypertension. Spiral CT scan in a patient with pulmonary hypertension reveals enlarged pulmonary arteries and an absence of thrombosis.
-
Pulmonary hypertension. CT pulmonary angiogram in a 42-year-old man who experienced severe chest pain after a long flight. Image demonstrates clots in both the right and left main pulmonary arteries.
-
Pulmonary hypertension. Ventilation-perfusion (V/Q) scans show bilateral mismatched segmental and subsegmental defects due to chronic thromboembolic disease, which has lead to secondary pulmonary arterial hypertension.
-
Pulmonary hypertension. Selective right pulmonary arteriogram demonstrates large central pulmonary arteries and attenuation of the peripheral vessels, without any definite demonstrable thrombi.
-
Pulmonary hypertension. Selective left pulmonary arteriogram reveals large central pulmonary arteries and attenuation of the peripheral vessels, without thrombi.
-
Pulmonary hypertension. Image shows an example of the successful resolution of secondary pulmonary arterial hypertension in a patient who underwent pulmonary arterial thromboendarterectomy with the removal of thrombi.