Practice Essentials
Portal vein thrombosis (PVT) is a pathologic condition characterized by lumen occlusion of the portal vein and its intrahepatic branches, commonly associated with chronic liver disease. PVT is often asymptomatic and is discovered as an incidental finding in the follow-up of chronic hepatopathy. Imaging plays a pivotal role in its detection and characterization. [1] Reduced portal blood flow caused by hepatic parenchymal disease and abdominal sepsis (ie, infectious or ascending thrombophlebitis) are the major causes.
PVT can be classified based on extension (eg, intrahepatic or extrahepatic or both, involving the spleno-mesenteric tract); degree (partial or complete); onset (acute or chronic); and with or without cavernomatous transformation. The most widely used classification is the one developed by Yerdel et al, as follows [2, 3, 4, 5, 6, 7] :
-
Grade I: thrombus at main portal vein affecting less than 50% of the lumen with or without minimal extension into the superior mesenteric vein (SMV).
-
Grade II: thrombus at portal vein affecting more than 50%, including complete thrombosis, with or without minimal extension into the SMV.
-
Grade III: complete PVT plus thrombosis extending into the proximal SMV with patent distal SMV.
-
Grade IV: complete PVT plus complete thrombosis of the SMV.
From a radiologic perspective, PVT can be classified into 4 categories, depending on the involvement of the intrahepatic portal vein, the extrahepatic portal vein, both intrahepatic and extrahepatic portal veins, and SMV and/or splenic vein (SV). [3, 4, 5, 6, 7]
Transient PVT is recognized with increasing frequency, in part because of greatly increased use of ultrasonography in the evaluation of patients with abdominal inflammation such as appendicitis. Hypercoagulable syndromes can lead to portomesenteric and splenic vein thrombosis. Patients with these conditions may present with acute or subacute intestinal angina. In late stages, patients may have variceal bleeding. [8, 9, 10, 11, 12] PVT is a potential complication of inflammatory bowel disease, usually associated with acquired or inherited risk factors for hypercoagulability. [13]
Pylephlebitis, or septic thrombophlebitis of the portal vein, is a rare condition, with an incidence of 0.37 to 2.7 cases per 100,000 person-years.In a study by Fusaro et al, the most frequently isolated bacteria were Escherichia coli (25%), Bacteroides (17%), and Streptococcus (15%). [14, 15]
PVT is a frequent complication of liver cirrhosis, and its prevalence increases with the severity of liver disease: from 1% in patients with compensated cirrhosis to 8-25% in candidates for liver transplantation. Several risk factors have been associated with the occurrence and progression of PVT. Although the negative effect of complete PVT on the surgical outcome of liver transplant recipients is clear, its impact on cirrhosis progression remains uncertain. Treatment options include anticoagulants and interventional thrombolytic therapies, which are chosen almost on a case-by-case basis depending on characteristics of the patient and the thrombus. [16]
Patients with liver cirrhosis and hepatocellular carcinoma (HCC) may have either malignant or benign PVT. Malignant PVT is a frequent complication of HCC, with a reported incidence of 36-44%. Benign PVT also frequently occurs in this population. In malignant PVT, tumor invades a branch of the portal vein. Benign PVT is usually secondary to sluggish flow in patients with cirrhosis and HCC, which leads to the development of thrombosis. [17, 18] Correct diagnosis and characterization of PVT are important for both prognosis and treatment. [19] Portal vein tumor thrombosis (PVTT) is a poor prognostic indicator, which is found at diagnosis in 10-40% of patients with HCC. Survival is approximately 2-4 months. [20]
Portal biliopathy (PB) refers to bile duct irregularity and bile duct strictures, which are not uncommon with portal hypertension and PVT; 5-30% of patients develop symptomatic bile duct obstruction. The pathogenesis is not clear, but bile duct compression by venous collaterals, ischemia, and infection has been implicated. Magnetic resonance cholangiopancreatography (MRCP) is the imaging modality of choice for managing PB. Portosystemic shunts are the treatment of choice for symptomatic PB. Changes in BP resolve after shunt surgery in most patients; however, 15-20% of patients require a subsequent bilioenteric bypass or endoscopic management for BP. Endoscopic therapy is offered to patients with bile duct stones or with cholangitis and to patients for whom portosystemic shunt surgery is not feasible. [21, 22, 23]
(See the images of portal vein thrombosis below.)
 Portal vein thrombosis. Longitudinal oblique sonogram was obtained through the liver in a 36-year-old woman with a known history of Leber optic atrophy (hereditary optic neuroretinopathy) and alcohol abuse who presented with nonspecific complaints of ill health and vague abdominal pain. Image shows ascites and a bright liver (fatty). The portal vein has a linear echogenic structure running the length of the portal vein (solid arrow). A complex cystic mass is present within the liver (open arrow).
Portal vein thrombosis. Longitudinal oblique sonogram was obtained through the liver in a 36-year-old woman with a known history of Leber optic atrophy (hereditary optic neuroretinopathy) and alcohol abuse who presented with nonspecific complaints of ill health and vague abdominal pain. Image shows ascites and a bright liver (fatty). The portal vein has a linear echogenic structure running the length of the portal vein (solid arrow). A complex cystic mass is present within the liver (open arrow).
 Portal vein thrombosis. Portal venous–phase enhanced axial CT scan, obtained in the same patient as in the previous image, shows a low-attenuating mass in the termination of the splenic vein (arrow). Note the multiple low-attenuating masses at the periphery of the right lobe of the liver.
Portal vein thrombosis. Portal venous–phase enhanced axial CT scan, obtained in the same patient as in the previous image, shows a low-attenuating mass in the termination of the splenic vein (arrow). Note the multiple low-attenuating masses at the periphery of the right lobe of the liver.
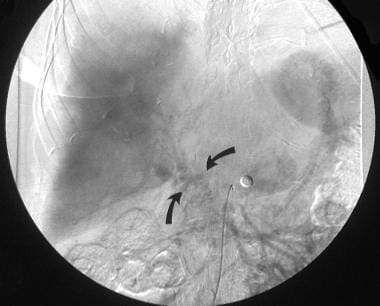 Portal vein thrombosis. Digital subtraction portal venous–phase superior mesenteric angiogram, obtained in the same patient as in the previous image, shows collateral vessels at the porta hepatis but no patent portal vein. Note that the liver is displaced away from the thoracic cage as a result of ascites. This patient had severe hepatic failure and died within 72 hours after the imaging examination. Postmortem examination showed early cirrhosis, fulminant pyogenic cholangitis, multiple liver abscesses, and portal vein and splenic and left gastric vein thrombosis.
Portal vein thrombosis. Digital subtraction portal venous–phase superior mesenteric angiogram, obtained in the same patient as in the previous image, shows collateral vessels at the porta hepatis but no patent portal vein. Note that the liver is displaced away from the thoracic cage as a result of ascites. This patient had severe hepatic failure and died within 72 hours after the imaging examination. Postmortem examination showed early cirrhosis, fulminant pyogenic cholangitis, multiple liver abscesses, and portal vein and splenic and left gastric vein thrombosis.
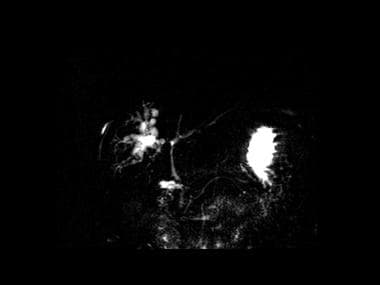 MRCP showing intrahepatic dilatation of the right lobe bile ducts and a long stricture of the common bile duct.
MRCP showing intrahepatic dilatation of the right lobe bile ducts and a long stricture of the common bile duct.
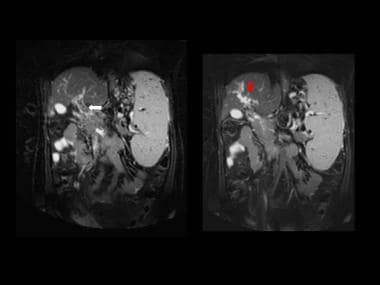 T1-contrast-enhanced coronal MR images showing thrombus within the main portal vein and a cavernous transformation of portal vein at the porta hepatis (same patient as in the previous image).
T1-contrast-enhanced coronal MR images showing thrombus within the main portal vein and a cavernous transformation of portal vein at the porta hepatis (same patient as in the previous image).
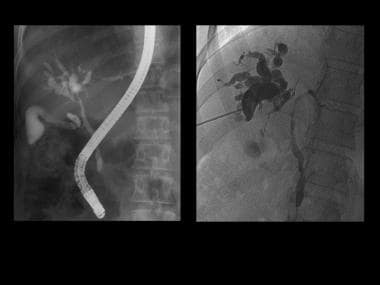 ERCP and PTC confirming the biliary abnormalities. The appearances are those of portal biliopathy (same patient as in the previous image).
ERCP and PTC confirming the biliary abnormalities. The appearances are those of portal biliopathy (same patient as in the previous image).
Generally, the portal vein enters the porta hepatis and divides into the right and left main branches. The right main branch divides into anterior and posterior branches that supply the anterior and posterior segments of the right lobe. The left main branch courses horizontally to the left before turning vertically to form the medial and lateral segmental branches. Several variations in portal venous anatomy have been described when ultrasonography, CT, and cadaveric dissection are performed.
Imaging modalities
Imaging has replaced open laparotomy or percutaneous biopsy for characterizing PVTT. Contrast-enhanced ultrasonography (CEUS), contrast-enhanced computed tomography (CT), and contrast-enhanced magnetic resonance imaging (MRI) have proved to be suitable modalities for differentiating benign from malignant PVT. [24, 17, 18]
CEUS allows detailed visualization of the hepatic microvasculature system (similar to CT or MRI), of focal liver lesions, and of PVT. Blunt thrombi are avascular and will not enhance during CEUS examination. Malignant thrombi have the same enhancement pattern as the tumor from which they originated, including rapid arterial phase hyperenhancement and slow or weak portal venous washout. [19] Imaging characteristics of malignant PVT on CT and MRI include intrathrombus neovascularity, venous expansion, and direct invasion of the vein. [24]
Preferred examinations include duplex Doppler ultrasonography and/or color Doppler ultrasonography, CT, magnetic resonance angiography (MRA) (see the image below), and arterial portography or splenoportography. [22, 25, 26, 27, 28]
 Portal vein thrombosis. Digital subtraction portal venous–phase superior mesenteric angiogram, obtained in the same patient as in the previous image, shows collateral vessels at the porta hepatis but no patent portal vein. Note that the liver is displaced away from the thoracic cage as a result of ascites. This patient had severe hepatic failure and died within 72 hours after the imaging examination. Postmortem examination showed early cirrhosis, fulminant pyogenic cholangitis, multiple liver abscesses, and portal vein and splenic and left gastric vein thrombosis.
Portal vein thrombosis. Digital subtraction portal venous–phase superior mesenteric angiogram, obtained in the same patient as in the previous image, shows collateral vessels at the porta hepatis but no patent portal vein. Note that the liver is displaced away from the thoracic cage as a result of ascites. This patient had severe hepatic failure and died within 72 hours after the imaging examination. Postmortem examination showed early cirrhosis, fulminant pyogenic cholangitis, multiple liver abscesses, and portal vein and splenic and left gastric vein thrombosis.
Tumors in the portal vein may have an appearance identical to that of thrombosis, but this appearance is far less common than others. Tumor in the portal vein is most frequently related to hepatocellular carcinoma. The thrombus may be partial or complete. It may be mixed with bland thrombus as well.
Adults who have acute PVT secondary to abdominal sepsis may completely recover, and the vessel may recanalize with successful treatment of the underlying sepsis. [29] In children, the portal vein may recanalize with the development of multiple, small, collateral channels. These channels are seen as a partially echogenic band of small vessels extending to the porta hepatis (cavernous transformation). These vessels have reduced flow velocity of 2-7 cm/s. Nonvisualization of the portal vein is strongly suggestive of occlusion. The portal vein may be seen as a band of high-level echoes at the porta hepatis. [30]
For patients who have contraindications to IV contrast, PVT can be detected on unenhanced MRI using T2, T1, and diffusion-weighted imaging. These sequences may also help differentiate between bland PVT, portal pyemia, and tumor thrombus. [31]
COVID-19 patients have been found to have increased thrombotic risk. Despite receiving prophylactic anticoagulation, many develop serious arterial and venous thromboembolic events. Clinicians should consider abdominal imaging in patients presenting with abdominal pain due to Clostridium difficile infection in the setting of COVID-19 to rule out complications such as PVT. [32]
Intervention
Development of PVT can precipitate the need for emergency endoscopy for sclerotherapy of varices, transjugular intrahepatic portosystemic shunt (TIPS) creation, surgical portocaval shunt creation, transjugular or transhepatic portomesenteric thrombolysis and thrombectomy, or even resection of ischemic bowel or liver transplantation. [33] However, PVT may complicate sclerotherapy. Fine-needle aspiration biopsy of PVT can be performed with color Doppler sonographic guidance to assess therapeutic effectiveness.
Early complications of TIPS creation that are detectable with ultrasonography include the following: intraperitoneal hemorrhage, shunt thrombosis, neck hematoma, compromise of hepatic blood supply, PVT, hepatic artery occlusion, hepatic infarction, failed stent deployment, inadequate stent expansion, stent retraction, stent fracture, and biliary obstruction. [34, 35, 36]
Delayed complications of TIPS creation that are detectable with ultrasonography include shunt stenosis caused by pseudointimal hyperplasia and hepatic vein stenosis. [37, 38]
Researchers considering the outcomes of patients with cirrhosis undergoing TIPS have noted that although an increase in portal vein flow velocity and a reduction in portal hypertension are achieved, the hypercoagulable state persists and may cause extension of residual PVT or rethrombosis, This has the potential to offset the increased portal velocity, leading to increased rates of shunt dysfunction and portal hypertension–related bleeding, ascites, or hepatic encephalopathy. PVT may also interrupt hepatic perfusion, causing hepatocyte ischemia and hormonal deprivation, which could result in hepatocyte death, parenchymal extinction, and ultimately deterioration of liver fibrosis and liver function, leading to increased mortality. [39]
Radiography
Portal vein thrombosis may be a complication of liver cirrhosis and may occur as a primary vascular disorder without liver disease. PVT can result in portal hypertension and may present with variceal bleeding or hypersplenism. Radiologists should be familiar with the imaging of PVT in patients of various ages and in different clinical scenarios. PVT can influence hepatic perfusion, the shape of the bile ducts, and liver architecture. Bland PVT and tumor-related PVT have major implications for hepatic transplant. [40]
Plain radiographs may reveal hepatosplenomegaly, an enlarged azygos vein, and paraspinal varices. Esophageal varices that consist of dilated submucosal veins in the lower esophagus occur chiefly as a consequence of portal hypertension, most often in cirrhosis. The varices appear as beaded or serpiginous translucent filling defects. Large esophageal varices are obvious and appear as nodular or vermiform, changeable filling defects within the esophagus. Smaller varices appear as scalloped esophageal folds, which are better seen on recumbent radiographs because they tend to disappear on upright images.
Computed Tomography
The portal vein supplies 75% of blood flow to the liver. Therefore, peak liver contrast enhancement occurs during the portal venous phase, about 60 seconds after the start of a bolus injection of contrast material. [41] With helical CT, a liver examination requires about 20 seconds to complete; images can usually be acquired in one breath hold. [42]
This technique can be extended to acquire a dual-phase contrast-enhanced CT scan in which the liver is imaged twice with a single contrast agent bolus—first during the arterial phase, and then through the portal venous phase. Dual-phase CT is indicated in some cases involving benign or malignant lesions in which vascular characteristics suggest the correct diagnosis (see the images below).
 Portal vein thrombosis. Portal venous–phase enhanced axial CT scan shows no flow in the portal vein. Note the multiple low-attenuating masses at the periphery of the right lobe of the liver.
Portal vein thrombosis. Portal venous–phase enhanced axial CT scan shows no flow in the portal vein. Note the multiple low-attenuating masses at the periphery of the right lobe of the liver.
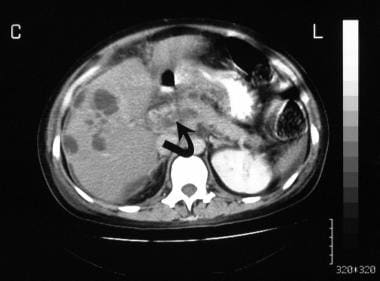
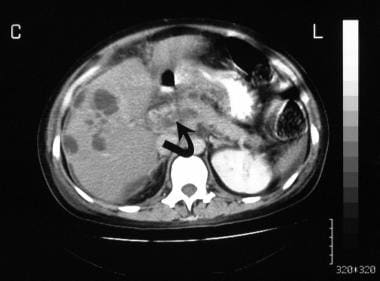 Portal vein thrombosis. Portal venous–phase enhanced axial CT scan, obtained in the same patient as in the previous image, shows a low-attenuating mass in the termination of the splenic vein (arrow). Note the multiple low-attenuating masses at the periphery of the right lobe of the liver.
Portal vein thrombosis. Portal venous–phase enhanced axial CT scan, obtained in the same patient as in the previous image, shows a low-attenuating mass in the termination of the splenic vein (arrow). Note the multiple low-attenuating masses at the periphery of the right lobe of the liver.
 Portal vein thrombosis. Portal venous–phase enhanced axial CT scan, obtained in the same patient as in the previous 2 images, shows an enlarged left gastric vein associated with a low-attenuating mass in the vein. No contrast enhancement is seen in the vein; this finding is suggestive of thrombosis (arrow).
Portal vein thrombosis. Portal venous–phase enhanced axial CT scan, obtained in the same patient as in the previous 2 images, shows an enlarged left gastric vein associated with a low-attenuating mass in the vein. No contrast enhancement is seen in the vein; this finding is suggestive of thrombosis (arrow).
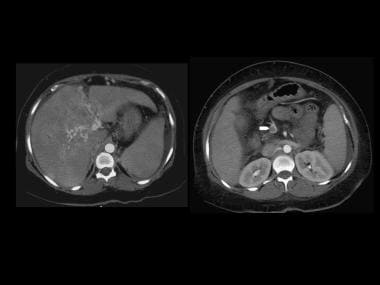 Contrast-enhanced axial CT depicts cavernous transformation following portal venous thrombosis. The portal venous thrombus is extending from the superior mesenteric vein (right image-arrow). Note the small ascites.
Contrast-enhanced axial CT depicts cavernous transformation following portal venous thrombosis. The portal venous thrombus is extending from the superior mesenteric vein (right image-arrow). Note the small ascites.
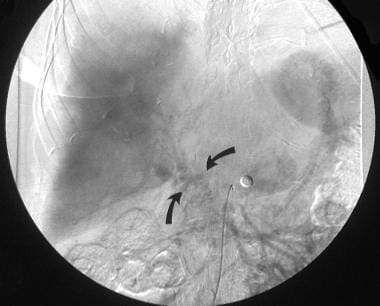
 Coronal reconstruction of contrast-enhanced CT depicts cavernous transformation following portal venous thrombosis. Note the gallbladder varices (red arrow) and a dilated bile duct (white arrow). The appearances suggest portal biliopathy.
Coronal reconstruction of contrast-enhanced CT depicts cavernous transformation following portal venous thrombosis. Note the gallbladder varices (red arrow) and a dilated bile duct (white arrow). The appearances suggest portal biliopathy.
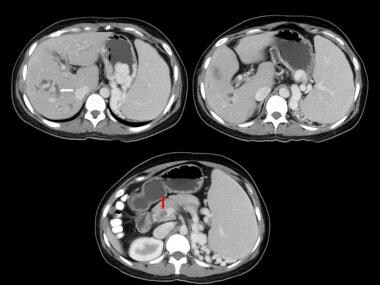 Axial contrast-enhanced CT images of the liver depicting dilated ducts (white arrow) and portal vein thrombus (red arrow) Note the varices around the spleen (same patient as in the previous image).
Axial contrast-enhanced CT images of the liver depicting dilated ducts (white arrow) and portal vein thrombus (red arrow) Note the varices around the spleen (same patient as in the previous image).
Angiographically assisted CT, or CT arterial portography, can provide better delineation of the portal venous system and portal venous enhancement of the liver. An angiographic catheter is placed in the common celiac axis, hepatic artery, or superior mesenteric artery via a modified Seldinger technique through the femoral artery. Image acquisition begins 3-5 seconds after injection of contrast agent is initiated. The examination should be completed as soon as possible, before the contrast material recirculates. To prevent significant artifacts related to the density of the contrast material, 70 mL of dilute (1-30%) iodinated contrast agent is used at an infusion rate of 2 mL/s. Although angiographically assisted CT can produce elegant images, it is invasive and expensive and is not widely accepted.
On contrast-enhanced CT scans, PVT may be depicted as a low-attenuating center in the portal vein surrounded by peripheral enhancement. Portal vein attenuation is 20-30 HU less than that in the aorta.
CT angiography (CTA) is an application of helical CT. The rapidity of helical CT allows the maintenance of a higher concentration of intravenous contrast medium, particularly through the arterial enhancement phase and offers the capability of 3-dimensional (3D) reconstruction. Both peripheral intravenous injections of contrast agent and CT arterial portography have been used as with CTA. CTA has shown great promise in the evaluation of hepatic vessels before liver resection. It provides preoperative surgical information about the segmental location of liver tumors, the segmental venous anatomy, and the presence of significant arterial anomalies. The value of CTA in the evaluation of portal hypertension is unclear, but CTA is likely to be useful because it may delineate collateral vessels, varices, and other findings in patients with portal hypertension.
Magnetic Resonance Imaging
The vascular anatomy of the liver may be outlined by using spin-echo and gradient-recalled-echo (GRE) techniques, but these techniques cannot demonstrate the direction of portal flow. Time-of-flight magnetic resonance imaging (MRI) with bolus tracking has been successful in the assessment of portal hypertension and its sequelae. Phase-contrast sequences can also be used to evaluate the portal vein, and phase-contrast cine magnetic resonance angiography (MRA) can show the direction of portal venous flow and the presence of portal vein thrombus. Magnetic resonance evaluation of the portal venous system accurately demonstrates thrombosis and the collateral circulation. Gadolinium enhancement is useful in this application (see the images below). [25, 43, 44]
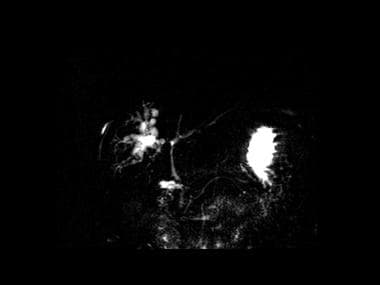 MRCP showing intrahepatic dilatation of the right lobe bile ducts and a long stricture of the common bile duct.
MRCP showing intrahepatic dilatation of the right lobe bile ducts and a long stricture of the common bile duct.
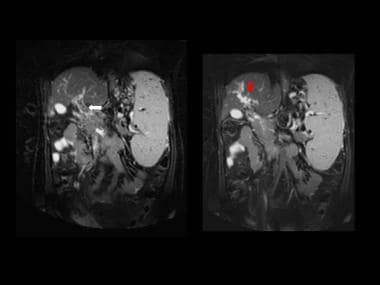 T1-contrast-enhanced coronal MR images showing thrombus within the main portal vein and a cavernous transformation of portal vein at the porta hepatis (same patient as in the previous image).
T1-contrast-enhanced coronal MR images showing thrombus within the main portal vein and a cavernous transformation of portal vein at the porta hepatis (same patient as in the previous image).
Magnetic resonance cholangiopancreatography (MRCP) coupled with dynamic 3D gradient-echo imaging not only can detect portal vein occlusion, cavernous transformation, and gallbladder varices but also can depict bile duct abnormalities associated with portal biliopathy. [45, 46, 47]
Lin and associates compared surgery and x-ray portography with 3D contrast-enhanced (CE) MRA in patients with portal vein involvement from HCC. [48] Overall sensitivity with 3D CE-MRA was 99%; specificity was 96%; the positive predictive value was 91%, and the negative predictive value was 99%. Accuracy in diagnosis of the main portal vein was 100%. Three-dimensional CE-MRA resulted in 7 false-positive interpretations involving 6 left portal veins and 1 right portal vein. One false-negative diagnosis with right portal vein involvement was made.
Shah and associates compared MRI with intraoperative findings in the diagnosis of PVT in transplantation candidates. In this study, the sensitivity and specificity of MRI for detecting main PVT were 100% and 98%, respectively. The cause of discordance between findings on MRI and at transplantation in 2 cases was a diminutive caliber of the main portal vein that was interpreted as recanalized chronic thrombosis on MRI. The major reason for a false-positive MRI is a diminutive but patent portal vein. [25]
An extremely slow portal venous flow is considered to be the cause of false-positive findings with unenhanced MRI and sonography. [49]
Timely diagnosis and treatment of PVT are crucial to prevent morbidity and mortality. However, current imaging tests cannot always accurately differentiate acute from chronic (nonocclusive) PVT. Magnetic resonance noncontrast thrombus imaging (MR-NCTI) has been shown to accurately differentiate acute from chronic venous thrombosis at other locations and may also prove valuable in the diagnostic management of PVT. Using 3-dimensional T1 fast field echo (3D T1 FFE) and 3D T1 Dixon FFE sequences, van Dam et al were able to distinguish between acute and chronic PVT. [50]
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). This disease has occurred in patients with moderate to end-stage renal disease after they were given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Ultrasonography
Portal vein thrombosis is recognized with increasing frequency on ultrasonography. Abdominal sepsis and reduced portal blood flow resulting from hepatic parenchymal disease are the major causes. Transient PVT is also recognized with increasing frequency, in part because of the great increase in the use of ultrasonography in the evaluation of patients with abdominal inflammation such as appendicitis. Tumor in the portal vein may have an appearance identical to that of thrombosis, [51, 52] but this appearance is far less common than others (see the images below).
 Portal vein thrombosis. Longitudinal oblique sonogram was obtained through the liver in a 36-year-old woman with a known history of Leber optic atrophy (hereditary optic neuroretinopathy) and alcohol abuse who presented with nonspecific complaints of ill health and vague abdominal pain. Image shows ascites and a bright liver (fatty). The portal vein has a linear echogenic structure running the length of the portal vein (solid arrow). A complex cystic mass is present within the liver (open arrow).
Portal vein thrombosis. Longitudinal oblique sonogram was obtained through the liver in a 36-year-old woman with a known history of Leber optic atrophy (hereditary optic neuroretinopathy) and alcohol abuse who presented with nonspecific complaints of ill health and vague abdominal pain. Image shows ascites and a bright liver (fatty). The portal vein has a linear echogenic structure running the length of the portal vein (solid arrow). A complex cystic mass is present within the liver (open arrow).
 Portal vein thrombosis. Power Doppler sonogram of the liver shows blood flow around an intraluminal filling defect in the portal vein (P).
Portal vein thrombosis. Power Doppler sonogram of the liver shows blood flow around an intraluminal filling defect in the portal vein (P).
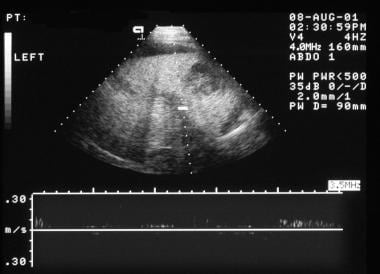 Portal vein thrombosis. Spectral Doppler sonogram of the liver, obtained in the same patient as in the previous image, shows the portal vein (cursor), which demonstrates no blood flow.
Portal vein thrombosis. Spectral Doppler sonogram of the liver, obtained in the same patient as in the previous image, shows the portal vein (cursor), which demonstrates no blood flow.
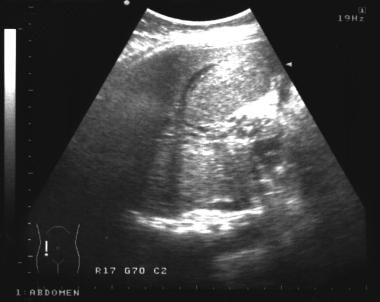 Portal vein thrombosis. Longitudinal oblique sonogram was obtained in a 28-year-old woman who was referred for gallbladder ultrasonography. On questioning, she gave a history of an episode of severe pyrexial illness and dehydration during childhood. The image shows several vascular tubular structures at the porta hepatis, which are suggestive of a cavernous transformation.
Portal vein thrombosis. Longitudinal oblique sonogram was obtained in a 28-year-old woman who was referred for gallbladder ultrasonography. On questioning, she gave a history of an episode of severe pyrexial illness and dehydration during childhood. The image shows several vascular tubular structures at the porta hepatis, which are suggestive of a cavernous transformation.
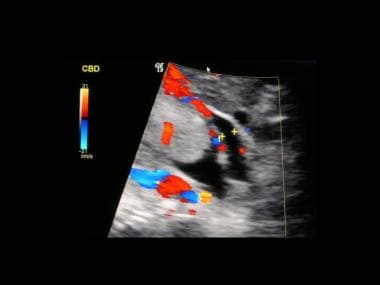
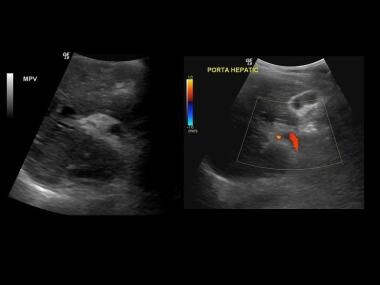
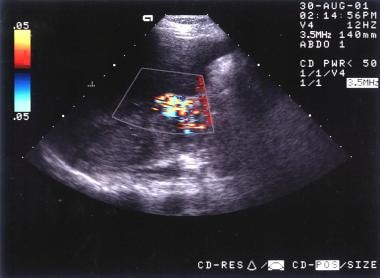 Portal vein thrombosis. Color Doppler sonogram, obtained in the same patient as in the previous image, shows flow in the cavernous transformation.
Portal vein thrombosis. Color Doppler sonogram, obtained in the same patient as in the previous image, shows flow in the cavernous transformation.
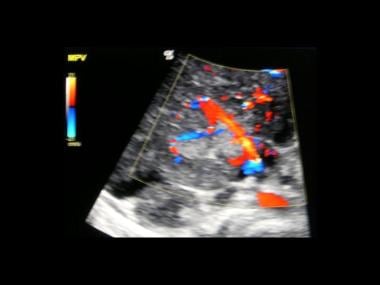
 Portal vein thrombosis. Color Doppler sonogram of the spleen, obtained in the same patient as in the previous 2 images, shows moderate splenomegaly with varices at the splenic hilum. Endoscopic findings confirmed the presence of esophageal varices.
Portal vein thrombosis. Color Doppler sonogram of the spleen, obtained in the same patient as in the previous 2 images, shows moderate splenomegaly with varices at the splenic hilum. Endoscopic findings confirmed the presence of esophageal varices.
 Ultrasound reveals an echogenic partially recanalized portal vein thrombus. The patient was a 36-year-old woman with idiopathic chronic portal vein thrombosis of 2 years' duration. She presented with cholestatic jaundice.
Ultrasound reveals an echogenic partially recanalized portal vein thrombus. The patient was a 36-year-old woman with idiopathic chronic portal vein thrombosis of 2 years' duration. She presented with cholestatic jaundice.
On sonograms, echogenic lesions in the portal vein may be evident. Clot with variable echogenicity may be depicted. The clot usually has moderate echogenicity, but if it is recently formed, it may be hypoechoic. Patent vessels may have increased intraluminal echogenicity because of erythrocyte rouleaux formation, which makes slow-flowing blood slightly echogenic. Increased or decreased echogenicity may be observed in the lumen of the portal vein. In isolation, this finding is not sufficient for diagnosis or exclusion of PVT.
PVT eliminates the usual venous flow signal from the lumen of the portal vein during pulsed or color flow Doppler imaging. Color flow Doppler images can show flow around a thrombus that partially blocks the vein. However, if flow is sluggish, the Doppler signal may not be detected. Color flow may be noted in other small collateral vessels. [53]
Incomplete occlusion may occur. This is common with neoplastic invasion. Alternatively, thrombolytic recanalization may occur. The 2 cannot be differentiated on sonograms. Cavernous malformation, spontaneous shunts, and splenorenal and portosystemic collaterals may be seen. The underlying cause (eg, hepatocellular carcinoma, metastases, cirrhosis, pancreatic neoplasms) may be evident. The incidence of PVT in portal hypertension is reported to be low.
The string sign—that is, thickening of the portal vein with narrowing of its lumen—is assumed to be caused by portal phlebitis. This is considered to be a precursor of PVT in patients with acute pancreatitis. The portal vein thrombus may be calcified. The diameter of the portal vein is larger than 15 mm in 38% of cases of PVT. [54]
Angiography
Among catheter-directed techniques, arterial portography is now the preferred method for evaluating the portal venous system because it is less invasive and has a lower complication rate than other methods (eg, splenoportography). This method involves indirect opacification of the portal venous system with an injection of contrast material into the splenic vein to outline the splenic and portal veins or the superior artery to outline the superior mesenteric and portal veins.
The 3 major indications for arterial portography are the following: (1) to examine patients with portal hypertension and its sequelae, particularly when surgical treatment is planned; (2) to determine the resectability of hepatic and pancreatic tumors when both arterial and venous phase angiographic findings make a significant contribution; and (3) to perform transcatheter embolization in cases of metastases of islet cell tumors or carcinoid metastases, or chemoembolization in cases of HCC. (A widely or partially patent portal vein is a prerequisite for such treatment.) [55]
Patient preparation and contraindications are the same as for conventional angiography. Selective catheters are used to cannulate the appropriate vessel. In a superior mesenteric artery injection, the tip of the catheter is placed to enable opacification of all branches with contrast material. Before delivery of the contrast agent, a vasodilator (tolazoline [Priscoline], papaverine, or prostaglandin E) is administered to improve opacification of the portal vein.
Manual or digital subtraction is necessary. If digital subtraction is used, administration of an anticholinergic drug (eg, glucagon) before imaging reduces bowel motion. Selective injection of the superior mesenteric artery can be used to outline the superior mesenteric and portal veins. For splenic and/or portal vein delineation, splenic artery catheterization is chosen. Injection of the left gastric artery consistently demonstrates esophageal varices.
Another technique for opacifying the portal system is wedged hepatic venous injections of carbon dioxide. [56] The low viscosity of the gas allows it to readily float across the hepatic sinusoids, successfully opacifying the portal vein in most cases.
Diagnostic modalities such as ultrasonography, CT, and MRI have reduced the diagnostic importance of arteriography in the diagnosis of liver tumor. The role of liver angiography seems to be limited to occasional mapping of the vascular anatomy before surgery (now largely performed with magnetic resonance angiography [MRA] or computed tomography angiography [CTA]) and transcatheter treatment of liver tumors. Venous phase imaging in the celiac axis and superior angiography provide sufficient detail to make direct portography unnecessary in most cases.
-
Portal vein thrombosis. Longitudinal oblique sonogram was obtained through the liver in a 36-year-old woman with a known history of Leber optic atrophy (hereditary optic neuroretinopathy) and alcohol abuse who presented with nonspecific complaints of ill health and vague abdominal pain. Image shows ascites and a bright liver (fatty). The portal vein has a linear echogenic structure running the length of the portal vein (solid arrow). A complex cystic mass is present within the liver (open arrow).
-
Portal vein thrombosis. Power Doppler sonogram of the liver shows blood flow around an intraluminal filling defect in the portal vein (P).
-
Portal vein thrombosis. Spectral Doppler sonogram of the liver, obtained in the same patient as in the previous image, shows the portal vein (cursor), which demonstrates no blood flow.
-
Portal vein thrombosis. Portal venous–phase enhanced axial CT scan shows no flow in the portal vein. Note the multiple low-attenuating masses at the periphery of the right lobe of the liver.
-
Portal vein thrombosis. Portal venous–phase enhanced axial CT scan, obtained in the same patient as in the previous image, shows a low-attenuating mass in the termination of the splenic vein (arrow). Note the multiple low-attenuating masses at the periphery of the right lobe of the liver.
-
Portal vein thrombosis. Portal venous–phase enhanced axial CT scan, obtained in the same patient as in the previous 2 images, shows an enlarged left gastric vein associated with a low-attenuating mass in the vein. No contrast enhancement is seen in the vein; this finding is suggestive of thrombosis (arrow).
-
Portal vein thrombosis. Digital subtraction portal venous–phase superior mesenteric angiogram, obtained in the same patient as in the previous image, shows collateral vessels at the porta hepatis but no patent portal vein. Note that the liver is displaced away from the thoracic cage as a result of ascites. This patient had severe hepatic failure and died within 72 hours after the imaging examination. Postmortem examination showed early cirrhosis, fulminant pyogenic cholangitis, multiple liver abscesses, and portal vein and splenic and left gastric vein thrombosis.
-
Portal vein thrombosis. Longitudinal oblique sonogram was obtained in a 28-year-old woman who was referred for gallbladder ultrasonography. On questioning, she gave a history of an episode of severe pyrexial illness and dehydration during childhood. The image shows several vascular tubular structures at the porta hepatis, which are suggestive of a cavernous transformation.
-
Portal vein thrombosis. Color Doppler sonogram, obtained in the same patient as in the previous image, shows flow in the cavernous transformation.
-
Portal vein thrombosis. Color Doppler sonogram of the spleen, obtained in the same patient as in the previous 2 images, shows moderate splenomegaly with varices at the splenic hilum. Endoscopic findings confirmed the presence of esophageal varices.
-
Color Doppler ultrasonography depicts a vascularized HCC portal venous thrombus.
-
Color Doppler ultrasonography depicts a vascularized HCC portal venous thrombus.
-
Contrast-enhanced axial CT depicts cavernous transformation following portal venous thrombosis. The portal venous thrombus is extending from the superior mesenteric vein (right image-arrow). Note the small ascites.
-
Coronal reconstruction of contrast-enhanced CT depicts cavernous transformation following portal venous thrombosis. Note the gallbladder varices (red arrow) and a dilated bile duct (white arrow). The appearances suggest portal biliopathy.
-
Ultrasound reveals an echogenic partially recanalized portal vein thrombus. The patient was a 36-year-old woman with idiopathic chronic portal vein thrombosis of 2 years' duration. She presented with cholestatic jaundice.
-
Axial contrast-enhanced CT images of the liver depicting dilated ducts (white arrow) and portal vein thrombus (red arrow) Note the varices around the spleen (same patient as in the previous image).
-
MRCP showing intrahepatic dilatation of the right lobe bile ducts and a long stricture of the common bile duct.
-
T1-contrast-enhanced coronal MR images showing thrombus within the main portal vein and a cavernous transformation of portal vein at the porta hepatis (same patient as in the previous image).
-
ERCP and PTC confirming the biliary abnormalities. The appearances are those of portal biliopathy (same patient as in the previous image).