Practice Essentials
Pigmented villonodular synovitis (PVNS), also known as diffuse tenosynovial giant cell tumor, is a benign proliferative disorder of uncertain etiology that affects synovial lined joints, bursae, and tendon sheaths (see the images below). The disorder results in various degrees of villous and/or nodular changes in the affected structures. PVNS lesions are monoarticular or solitary. Polyarticular disease is uncommon but more likely in children. [1, 2, 3, 4, 5, 6]
PVNS is an uncommon disease. [7] Prevalence is approximately 9.2 cases of extra-articular and 1.8 cases of intra-articular disease per 1 million population. [1, 2] Localized lesions are more common than diffuse involvement, comprising 77% of total lesions in one review, with a 3.3:1 localized-to-diffuse predominance ratio. Diffuse PVNS affects predominantly large joints, with the knee being the most common (66-80%). [8, 9, 10] The hip, ankle, shoulder, and elbow follow in descending frequency. [11, 12, 13] The localized intra-articular form of PVNS occurs almost exclusively within the knee. Tendon sheaths of the hand and wrist are affected more frequently, with the volar aspect of the index and long fingers being the most common sites of disease. Diffuse PVNS has nearly equal incidence in male and female patients, while the localized form demonstrates a female-to-male predominance ratio of 1.5-2:1. Diagnosis is more common between ages 20 and 50 years, with a median age of 30 years.
PVNS lesions on histology demonstrate synovial cell proliferation, xanthomatous cell accumulation, hemosiderin deposition, and the presence of multinucleated giant cells. Numerous pathophysiologic mechanisms, including inflammation (multinucleated giant cells), response to antecedent trauma, repeated hemorrhage into the joint (hemosiderin), and disorders of lipid metabolism (xanthoma cells), have been proposed. [14]
PVNS is overwhelmingly benign, with only a few cases of malignant transformation reported, but it may result in significant morbidity if left untreated. Pain, loss of function, and eventual joint destruction may result. The primary treatment options include surgical resection via synovectomy or radiation therapy. [15] Recurrence is reduced with complete resection, and it is achieved more often with localized disease. Radiation therapy may be used as the primary treatment method or in concert with surgical excision.
Preferred examination
Clinical information and plain radiographs are not always sufficient to establish a correct diagnosis. MRI findings are characteristic, but not pathognomonic, for this disorder. Rarely, biopsy is required to establish preoperative tissue diagnosis. Plain radiographs demonstrate signs similar to joint effusion or soft-tissue swelling. Calcifications are not a usual feature of PVNS. Rarely, foci of dystrophic calcification may be seen in an area of PVNS. (See the images below.) [16, 17]
Computed tomography (CT) scans demonstrate a hyperdense soft-tissue mass in the joint or tendon sheath. The hyperdensity of the mass is a reflection of repeated hemorrhage and of blood degradation products within the joint. [16, 18, 19]
MR images demonstrate various appearances ranging from low signal through isointense to hyperintense signals on spin-echo images, reflecting the presence of blood and its degradation products. Hemosiderin appears as low signal on T1- and T2-weighted images. Differentiating calcifications from hemosiderin-laden foci in the setting of PVNS may be difficult, and plain films should be used in this setting to confirm or deny the presence of calcifications. [16, 17]
A combination of plain films and MRI should be used in preoperative evaluation of a patient with PVNS. This combination yields an accurate diagnosis and maps out the extent of disease for the surgeon prior to treatment.
 Pigmented villonodular synovitis of the knee. Plain radiographic findings of the knee apparently are normal except for the curvilinear calcification seen peripherally to the medial femoral condyle.
Pigmented villonodular synovitis of the knee. Plain radiographic findings of the knee apparently are normal except for the curvilinear calcification seen peripherally to the medial femoral condyle.
Two primary forms of PVNS are described: a diffuse form that affects the entire synovial lining of a joint, bursa, or tendon sheath, and a rare focal, or localized, form. The diffuse form typically involves the large joints (see the first 2 images below), while the localized form typically occurs around the small joints of the hands and feet (see the last 2 images below).
 Pigmented villonodular synovitis of the knee. Coronal T2-weighted magnetic resonance imaging (MRI) scan shows low signal mass above the medial femoral condyle, posteriorly.
Pigmented villonodular synovitis of the knee. Coronal T2-weighted magnetic resonance imaging (MRI) scan shows low signal mass above the medial femoral condyle, posteriorly.
 Pigmented villonodular synovitis of the knee. Sagittal T1-weighted magnetic resonance imaging scan (MRI) of the knee shows inhomogeneous foci of low signal in the suprapatellar pouch and, posteriorly, just above the femoral condyle.
Pigmented villonodular synovitis of the knee. Sagittal T1-weighted magnetic resonance imaging scan (MRI) of the knee shows inhomogeneous foci of low signal in the suprapatellar pouch and, posteriorly, just above the femoral condyle.
 Giant cell tumor of tendon sheath. Anteroposterior plain film of the foot shows a circumferential mass, which is more apparent on the medial aspect of the proximal phalanx of the great toe. Note the degenerative cystic changes at the interphalangeal joint of the great toe. Mild saucerization or pressure erosion of the medial cortex of the proximal phalanx is seen.
Giant cell tumor of tendon sheath. Anteroposterior plain film of the foot shows a circumferential mass, which is more apparent on the medial aspect of the proximal phalanx of the great toe. Note the degenerative cystic changes at the interphalangeal joint of the great toe. Mild saucerization or pressure erosion of the medial cortex of the proximal phalanx is seen.
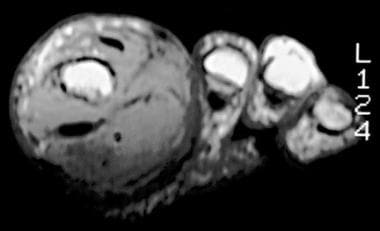 Giant cell tumor of tendon sheath. Axial T1-weighted magnetic resonance imaging (MRI) scan of the foot shows intermediate signal mass surrounding the proximal phalanx of the great toe and displacing the tendons away from the bone, especially in the plantar aspect of the foot.
Giant cell tumor of tendon sheath. Axial T1-weighted magnetic resonance imaging (MRI) scan of the foot shows intermediate signal mass surrounding the proximal phalanx of the great toe and displacing the tendons away from the bone, especially in the plantar aspect of the foot.
Neoplasia is the currently accepted underlying etiology, with empirical and genetic evidence supporting this theory. PVNS has demonstrated the capability of autonomous growth and rare malignant transformation. Several genetic studies have demonstrated associated cytogenetic aberrations, including rearrangement involving the CSF-1 and COL6a3 genes, as well as association with trisomy 5 and trisomy 7. [1, 20, 21] Not all cases are associated with such genetic anomalies, suggesting a multifactorial etiology for the disease.
The localized form often appears around tendon sheaths, in which case it is termed giant cell tumor of the tendon sheath. It primarily affects the knee (66-80% of cases) but also affects the hips, ankle, shoulder, and elbow. [2] Rarely, the localized form may develop around large joints. The term PVNS generally is used when the condition, in either diffuse or localized form, affects a joint. Imaging plays an important role in the diagnosis, treatment, and follow-up monitoring of the disorder.
Limitations of techniques
Plain radiographs cannot confidently exclude effusion as a cause of symptoms, nor can they help determine the extent of disease.
CT scan findings invariably are diagnostic; however, CT scanning is hobbled by its inability to completely show the extent of disease and other pathology around or within the joint.
MRI findings are diagnostic in more than 95% of patients. Rarely, synovial osteochondromatosis (SOC) may demonstrate a similar appearance, and plain radiographs may be necessary to exclude SOC in the appropriate setting.
Radiography
Findings on plain radiographs are not specific. (See the image below.) In the diffuse form, pigmented villonodular synovitis (PVNS) presents as painless, monoarticular joint swelling. Findings of mineralization of the bones around the lesion are normal until late in the disease, with preservation of the cartilage space and no calcifications.
Well-corticated pressure erosions (saucerization) and cysts may occur on either side or both sides of the joint. Secondary degenerative changes may occur in the affected joint in long-standing disease, with concentric cartilage space narrowing, subchondral cyst, and osteophyte formation.
The diffuse form presents with joint effusion/soft-tissue swelling. Occasionally, the effusion is dense because of the presence of hemosiderin. The nodular form most commonly results in localized swelling of the palmar aspect of a finger.
 Pigmented villonodular synovitis of the knee. Plain radiographic findings of the knee apparently are normal except for the curvilinear calcification seen peripherally to the medial femoral condyle.
Pigmented villonodular synovitis of the knee. Plain radiographic findings of the knee apparently are normal except for the curvilinear calcification seen peripherally to the medial femoral condyle.
Computed Tomography
CT scan findings are as follows:
-
Secondary to the presence of intracellular and extracellular hemosiderin, lesions have high attenuation and appear hyperdense on CT scans.
-
Because of improved tissue contrast, CT scanning is valuable in delineating bone cysts and erosions.
-
Affected synovium is hypervascular and generally enhances following administration of radiographic contrast.
CT scanning is useful for needle biopsy guidance when a histologic diagnosis is required and is especially useful for preoperative planning.
Radiographic contrast may be injected into the joint following joint aspiration. With contrast filling of the joint, findings demonstrate multiple, irregular, nodular filling defects of variable sizes. These produce the typical cobblestone appearance of the synovium seen on arthrography. [16, 18, 19]
Magnetic Resonance Imaging
MRI has become the imaging modality of choice in the evaluation of synovial and soft-tissue lesions. Pigmented villonodular synovitis (PVNS) demonstrates variable appearance on MRI, depending on the composition of the lesion and its relative proportions of hemosiderin, lipid, fibrous tissue, cyst formation, and cellular elements and on the imaging parameters. [3, 13, 16, 17, 22, 23, 24, 25, 26]
Characteristic findings include nodular intra-articular masses that demonstrate low signal intensity on T1-, T2-, and proton density–weighted sequences (as in the images below). Low signal intensity is due to hemosiderin deposits within the affected tissue and is accentuated on T2-weighted sequences, most notably on gradient-recalled echo sequences. [1, 2]
Hemophilic arthropathy, synovial hemangioma, synovial chondromatosis, gout, and amyloid arthropathy may all present similarly on MRI.
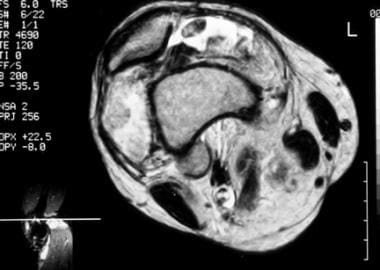
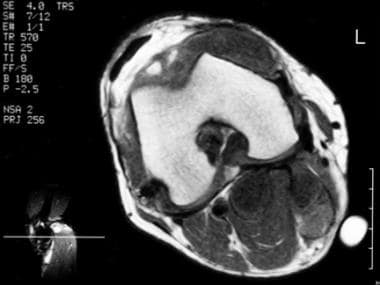 Pigmented villonodular synovitis of the knee. Axial T1- and T2-weighted magnetic resonance imaging (MRI) scans show tissue areas with abnormally low and high signals anteriorly in the suprapatellar pouch and, posteriorly, deep and superficial to the medial head of the gastrocnemius (Baker and popliteal bursae).
Pigmented villonodular synovitis of the knee. Axial T1- and T2-weighted magnetic resonance imaging (MRI) scans show tissue areas with abnormally low and high signals anteriorly in the suprapatellar pouch and, posteriorly, deep and superficial to the medial head of the gastrocnemius (Baker and popliteal bursae).
 Pigmented villonodular synovitis of the knee. Axial T1- and T2-weighted magnetic resonance imaging (MRI) scans show tissue areas with abnormal low and high signals anteriorly in the suprapatellar pouch (same patient as in the previous image) and, posteriorly, deep and superficial to the medial head of the gastrocnemius (Baker and popliteal bursae).
Pigmented villonodular synovitis of the knee. Axial T1- and T2-weighted magnetic resonance imaging (MRI) scans show tissue areas with abnormal low and high signals anteriorly in the suprapatellar pouch (same patient as in the previous image) and, posteriorly, deep and superficial to the medial head of the gastrocnemius (Baker and popliteal bursae).
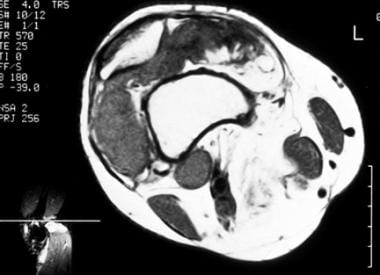 Pigmented villonodular synovitis of the knee. Axial T1- and T2-weighted magnetic resonance imaging (MRI) scans performed at a higher level above the knee joint show mixed signal pattern in the suprapatellar pouch. Nodular, low-signal foci are interspersed within inhomogeneous low- and high-signal areas. The foci correspond to areas of hemosiderin-laden hyperplastic synovium of pigmented villonodular synovitis.
Pigmented villonodular synovitis of the knee. Axial T1- and T2-weighted magnetic resonance imaging (MRI) scans performed at a higher level above the knee joint show mixed signal pattern in the suprapatellar pouch. Nodular, low-signal foci are interspersed within inhomogeneous low- and high-signal areas. The foci correspond to areas of hemosiderin-laden hyperplastic synovium of pigmented villonodular synovitis.
 Pigmented villonodular synovitis of the knee. Axial T1- and T2-weighted magnetic resonance imaging (MRI) scans performed at a higher level above the knee joint show mixed signal pattern in the suprapatellar pouch. Nodular, low-signal foci are interspersed within inhomogeneous low- and high-signal areas. The foci correspond to areas of hemosiderin-laden hyperplastic synovium of pigmented villonodular synovitis.
Pigmented villonodular synovitis of the knee. Axial T1- and T2-weighted magnetic resonance imaging (MRI) scans performed at a higher level above the knee joint show mixed signal pattern in the suprapatellar pouch. Nodular, low-signal foci are interspersed within inhomogeneous low- and high-signal areas. The foci correspond to areas of hemosiderin-laden hyperplastic synovium of pigmented villonodular synovitis.
The presence of fat signal also is apparent secondary to the presence of lipid-laden macrophages, resulting in focal regions of high signal intensity on T1-weighted images and intermediate signal on T2-weighted images.
Hyperplastic and hypervascular synovium enhances following intravascular administration of gadolinium chelates.
Bony erosions (when present) and extra-articular extension of the lesion are well demonstrated on MRI. MRI findings are not pathognomonic for PVNS, and similar findings may be seen in rheumatoid arthritis, hemophilic arthropathy, amyloid arthropathy, synovial osteochondromatosis, gout, and degenerative joint disease.
Nuclear Imaging
Bone scans do not play a significant or routine role in the diagnosis of pigmented villonodular synovitis (PVNS). On bone scan, the hypervascularity and areas of erosion may result in increased radionuclide uptake. Soft-tissue masses often demonstrate increased uptake on blood-pool images.
Positron emission tomography (PET) imaging is of similarly little utility in establishing the diagnosis or extent of involvement of PVNS. The lesions are generally hypermetabolic. Unsuspected lesions may be found during surveillance for neoplasia on PET scans.
PVNS and giant cell tumor of the tendon sheath (GCTTS), according to a study by Broski et al, can be intensely hypermetabolic, mimicking musculoskeletal metastases on 18F-FDG PET/CT. [18] PVNS displays as a focal FDG-avid lesion, which can masquerade as a metastatic lesion, on PET/CT. [2]
-
Pigmented villonodular synovitis of the knee. Plain radiographic findings of the knee apparently are normal except for the curvilinear calcification seen peripherally to the medial femoral condyle.
-
Pigmented villonodular synovitis of the knee. Coronal T2-weighted magnetic resonance imaging (MRI) scan shows low signal mass above the medial femoral condyle, posteriorly.
-
Pigmented villonodular synovitis of the knee. Sagittal T1-weighted magnetic resonance imaging scan (MRI) of the knee shows inhomogeneous foci of low signal in the suprapatellar pouch and, posteriorly, just above the femoral condyle.
-
Pigmented villonodular synovitis of the knee. Axial T1- and T2-weighted magnetic resonance imaging (MRI) scans show tissue areas with abnormally low and high signals anteriorly in the suprapatellar pouch and, posteriorly, deep and superficial to the medial head of the gastrocnemius (Baker and popliteal bursae).
-
Pigmented villonodular synovitis of the knee. Axial T1- and T2-weighted magnetic resonance imaging (MRI) scans show tissue areas with abnormal low and high signals anteriorly in the suprapatellar pouch (same patient as in the previous image) and, posteriorly, deep and superficial to the medial head of the gastrocnemius (Baker and popliteal bursae).
-
Pigmented villonodular synovitis of the knee. Axial T1- and T2-weighted magnetic resonance imaging (MRI) scans performed at a higher level above the knee joint show mixed signal pattern in the suprapatellar pouch. Nodular, low-signal foci are interspersed within inhomogeneous low- and high-signal areas. The foci correspond to areas of hemosiderin-laden hyperplastic synovium of pigmented villonodular synovitis.
-
Pigmented villonodular synovitis of the knee. Axial T1- and T2-weighted magnetic resonance imaging (MRI) scans performed at a higher level above the knee joint show mixed signal pattern in the suprapatellar pouch. Nodular, low-signal foci are interspersed within inhomogeneous low- and high-signal areas. The foci correspond to areas of hemosiderin-laden hyperplastic synovium of pigmented villonodular synovitis.
-
Giant cell tumor of tendon sheath. Anteroposterior plain film of the foot shows a circumferential mass, which is more apparent on the medial aspect of the proximal phalanx of the great toe. Note the degenerative cystic changes at the interphalangeal joint of the great toe. Mild saucerization or pressure erosion of the medial cortex of the proximal phalanx is seen.
-
Giant cell tumor of tendon sheath. Axial T1-weighted magnetic resonance imaging (MRI) scan of the foot shows intermediate signal mass surrounding the proximal phalanx of the great toe and displacing the tendons away from the bone, especially in the plantar aspect of the foot.
-
Giant cell tumor of tendon sheath. Coronal T1-weighted, fat-saturated, contrast-enhanced MRIs showing a well-defined enhancing mass along the medial aspect of the thumb, without appreciable effect on the underlying bone.
-
Localized intra-articular pigmented villonodular synovitis (PVNS). Lateral radiograph of the knee in a patient with localized intra-articular PVNS showing a moderate-sized effusion in the suprapatella pouch and soft-tissue fullness in the Hoffa fat pad.
-
Diffuse-type pigmented villonodular synovitis (PVNS) in the ankle. Lateral radiograph demonstrates a prominent soft-tissue mass seen both in the anterior and posterior aspects of the joint.
-
Diffuse-type pigmented villonodular synovitis (PVNS) of the ankle. Sagittal intermediate-density MRI of the ankle showing a soft-tissue mass along the anterior tibiotalar joint, with smaller soft-tissue masses posteriorly, which proved contiguous throughout the ankle.
-
Giant cell tumor of tendon sheath. Axial T1-weighted image of the ankle demonstrates a low-signal lesion anterior to the tibiotalar joint, which proved intimately related to the tibialis anterior tendon.