Practice Essentials
Pleomorphic adenoma (see the images below), also called benign mixed tumor, is by far the most common benign salivary gland tumor, accounting for as many as 80% of all such tumors. Although pleomorphic adenomas most commonly occur in the parotid gland (about 85%), this tumor may be encountered in the submandibular, lingual, and minor salivary glands as well. Although almost one half of tumors found in the minor salivary glands are malignant, the pleomorphic adenoma is still the most common tumor in these glands. [1, 2, 3, 4]
Approximately 6% of pleomorphic adenomas transform into carcinoma ex pleomorphic adenoma, which is defined as a carcinoma originating from a primary (de novo) or recurrent benign pleomorphic adenoma. [5]
Computed tomography (CT) scanning or magnetic resonance imaging (MRI) depicts the mass, and the findings may be essentially diagnostic in routine cases with typical features. MRI has the advantages of multiplanar imaging, and MRI results may suggest the tissue type on the basis of signal intensity characteristics. CT is often the first study ordered in patients with neck masses, and scans can show the mass and the retromandibular vein. Newer multisection CT scanners offer multiplanar capabilities rivaling that of MRI. [2, 6, 7, 8, 9, 10, 11, 12]
Disadvantages of CT include radiation exposure, the use of iodinated contrast material, and tissue distinction poorer than that of other studies. CT may also be problematic in cases of benign pleomorphic adenomas when the outer margin of the tumor appears indistinct and suggests malignant invasion of the surrounding tissue. MRIs show the well-defined outer borders in these instances. In many cases, however, CT may be the only study needed to guide the surgeon.
Some authors have reported excellent sensitivity with ultrasonography, although ultrasound typically does not help the surgeon understand the 3-dimensional (3D) relationship of the tumor to the parotid gland and the facial nerve. [13, 6, 14, 7, 15, 8, 16] On sonograms, pleomorphic adenomas typically appear as smooth, round, hypoechoic masses with distal acoustic enhancement. [9, 17] Lobulations are commonly visualized. Large tumors appear more heterogeneous than small ones and are better imaged with CT or MRI than with sonography. [18, 15] Even in patients in whom the diagnosis is made by means of sonography and biopsy, CT or MRI is needed for preoperative planning.
Evidence suggests that dual-isotope imaging with technetium-99m and thallium-201 single-photon emission CT (SPECT) is accurate in distinguishing various tumors of the salivary glands, including pleomorphic adenomas.
(See the images below.)
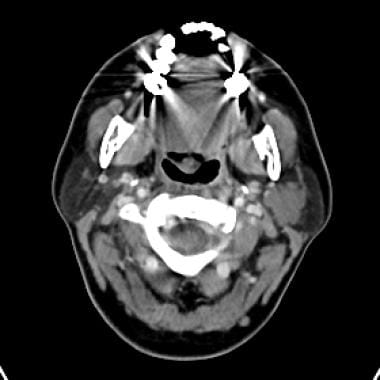 Enhanced CT image shows a lobular mass in the left parotid gland. The circumscribed borders and location are highly suggestive of pleomorphic adenoma, which was confirmed with fine-needle aspiration.
Enhanced CT image shows a lobular mass in the left parotid gland. The circumscribed borders and location are highly suggestive of pleomorphic adenoma, which was confirmed with fine-needle aspiration.
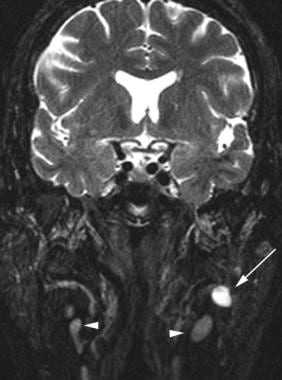 Coronal fat-saturated T2-weighted MRI demonstrates a hyperintense mass (pleomorphic adenoma) involving the deep lobe of the left parotid gland (arrow). The tumor has higher signal intensity than that of the visualized lymph nodes (arrowheads). This finding can help in distinguishing pleomorphic adenomas from intraparotid lymph nodes.
Coronal fat-saturated T2-weighted MRI demonstrates a hyperintense mass (pleomorphic adenoma) involving the deep lobe of the left parotid gland (arrow). The tumor has higher signal intensity than that of the visualized lymph nodes (arrowheads). This finding can help in distinguishing pleomorphic adenomas from intraparotid lymph nodes.
Pleomorphic adenomas have a female predominance (2:1) and typically affect patients between 30 and 60 years of age. [13] Pleomorphic adenomas are associated with a 2-25% risk of malignant transformation over time, and recurrence rates have been shown to be higher in patients who undergo enucleation. [19]
Complete excision of pleomorphic parotid adenomas are difficult because of critical anatomic issues, such as the presence of the facial nerve. Pleomorphic adenoma can metastasize, especially when the excision is incomplete. The 3 most common sites for metastasizing pleomorphic adenoma are bone (36.6%), lung (33.8%), and cervical lymph nodes (20.1%). [20]
Computed Tomography
Pleomorphic adenomas (see the images below) are typically smooth, well-marginated tumors, although nodularity along the outer surface is sometimes present. The attenuation values of the mass are usually homogeneous and higher than that of the surrounding gland, although lower attenuation masses that resemble cysts are occasionally seen. [21, 21, 22, 10, 11, 23]
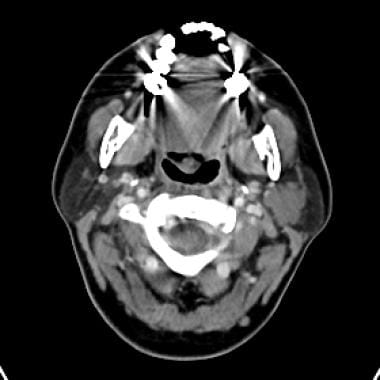 Enhanced CT image shows a lobular mass in the left parotid gland. The circumscribed borders and location are highly suggestive of pleomorphic adenoma, which was confirmed with fine-needle aspiration.
Enhanced CT image shows a lobular mass in the left parotid gland. The circumscribed borders and location are highly suggestive of pleomorphic adenoma, which was confirmed with fine-needle aspiration.
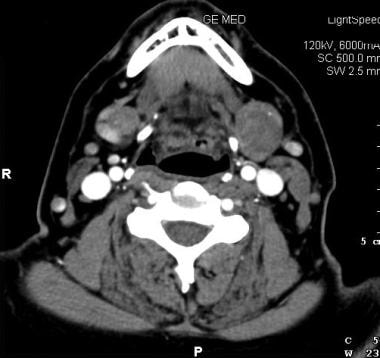 Axial contrast-enhanced CT scan demonstrates a poorly enhancing mass (pleomorphic adenoma) involving the left submandibular gland. The mass is smoothly marginated and causes the gland to expand. Image courtesy of Dr Doug Phillips, Director of Neuroradiology, University of Virginia.
Axial contrast-enhanced CT scan demonstrates a poorly enhancing mass (pleomorphic adenoma) involving the left submandibular gland. The mass is smoothly marginated and causes the gland to expand. Image courtesy of Dr Doug Phillips, Director of Neuroradiology, University of Virginia.
Tumor enhancement is variable and can result in a missed diagnosis if delayed images are not acquired. Pleomorphic adenomas are poorly enhancing in the early phase of contrast enhancement, although the amount of enhancement increases over time. Delayed images obtained at 5-10 minutes are often useful.
Lev et al described increased degree and homogeneity of tumor enhancement over time. Although the average delay was 24 minutes, in practice, a 5- to 10-minute delay is almost as effective. [22]
When pleomorphic adenomas become large, they may develop a heterogeneous appearance with areas of necrosis, hemorrhage, cysts, and calcification. Large tumors commonly have a lobulated contour, which strongly suggests the diagnosis.
Although certain CT features (eg, lobulation, homogeneity, delayed contrast enhancement) can suggest the diagnosis of pleomorphic adenoma, these findings are not specific to the tumor. [24] In addition, CT results may falsely suggest invasion of the surrounding tissue; in these cases, MRI should be performed to ensure that a diagnosis of malignancy is not incorrectly made. MRIs can demonstrate a well-defined capsule, even when the border appears irregular on CT scans.
Kim and Lee reported that enhanced, multidetector CT scanning with a 50-second delay between contrast injection and scanning can be used to differentiate Warthin tumors from pleomorphic adenomas and malignant tumors. [10]
Magnetic Resonance Imaging
Pleomorphic adenomas, as shown in the images below, are usually well-circumscribed, homogeneous masses with low intensity on T1-weighted images and high intensity on T2-weighted images. They commonly have a rim of decreased signal intensity on T2-weighted images; this rim also appears hypointense on fat-suppressed T1-weighted images. This finding represents the surrounding fibrous capsule. [24, 25, 8, 16, 26]
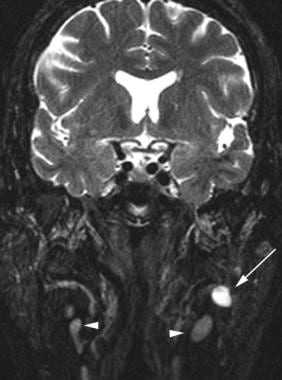 Coronal fat-saturated T2-weighted MRI demonstrates a hyperintense mass (pleomorphic adenoma) involving the deep lobe of the left parotid gland (arrow). The tumor has higher signal intensity than that of the visualized lymph nodes (arrowheads). This finding can help in distinguishing pleomorphic adenomas from intraparotid lymph nodes.
Coronal fat-saturated T2-weighted MRI demonstrates a hyperintense mass (pleomorphic adenoma) involving the deep lobe of the left parotid gland (arrow). The tumor has higher signal intensity than that of the visualized lymph nodes (arrowheads). This finding can help in distinguishing pleomorphic adenomas from intraparotid lymph nodes.
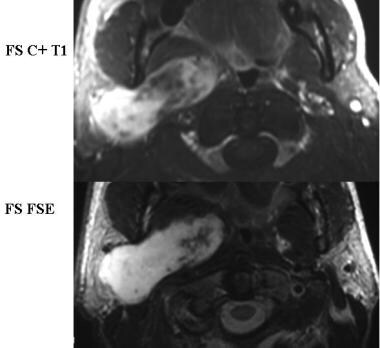 Contrast-enhanced T1- and T2-weighted MRIs in a patient with carcinoma ex pleomorphic adenoma. A large mass with a heterogeneous medial portion involves primarily the deep lobe of the parotid gland. The ill-defined anteromedial border, heterogeneous signal intensity, and enhancement, as well as the size of the tumor, all suggest the possibility of carcinomatous transformation. Image courtesy of Dr Linda Gray, Professor of Neuroradiology, Duke University.
Contrast-enhanced T1- and T2-weighted MRIs in a patient with carcinoma ex pleomorphic adenoma. A large mass with a heterogeneous medial portion involves primarily the deep lobe of the parotid gland. The ill-defined anteromedial border, heterogeneous signal intensity, and enhancement, as well as the size of the tumor, all suggest the possibility of carcinomatous transformation. Image courtesy of Dr Linda Gray, Professor of Neuroradiology, Duke University.
A well-defined parotid mass with increased signal intensity on proton density- and T2-weighted images is highly suggestive of the diagnosis. In fact, the increased signal intensity on T2-weighted images is so prevalent that any parotid mass with this finding should be viewed with suspicion, as this often indicates a carcinoma ex pleomorphic adenoma. [5]
When it becomes large, the tumor may lose its homogeneous appearance on MRI, as with CT. It may have areas of fibrosis, necrosis, and hemorrhage. Inhomogeneous signal intensity should be apparent in these cases. Lobulation is commonly visualized and is, in itself, also suggestive of the diagnosis.
After gadolinium enhancement, the tumors are homogeneously enhancing unless they are large. Unlike CT, MRI has no role in delayed imaging.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Degree of confidence
The diagnosis of pleomorphic adenoma can be at least strongly suggested in most cases. Special attention should be paid to the signal intensity of the tumor and to any possible invasion into adjacent soft tissues.
Kakimoto et al investigated the CT scanning and MRI features of 50 pleomorphic adenomas of the head and neck in 50 patients and found that tumor detectabilities were 77% on axial plain CT images, 90% on axial CE CT images, 86% on axial T1-weighted MRI, 88% on axial T2-weighted MRI, and 85% on axial CE T1-weighted MR images. The capsule could be hardly detected on CT images but could be detected in many cases on MR images. The authors therefore concluded that pleomorphic adenomas of the head and neck should be evaluated with MRI over CT. [11]
Ultrasonography
Some authors have reported excellent sensitivity with ultrasonography, although ultrasound typically does not help the surgeon understand the 3-dimensional (3D) relationship of the tumor to the parotid gland and the facial nerve. [6, 14, 7, 15, 8, 16] Ultrasonography is heavily operator dependent, provides limited visualization of the deep lobe of the parotid gland, and often has difficulty distinguishing benign from malignant neoplasms. [13] On sonograms, pleomorphic adenomas typically appear as smooth, round, hypoechoic masses with distal acoustic enhancement. [9, 17] Lobulations are commonly visualized. Large tumors appear more heterogeneous than small ones and are better imaged with CT or MRI than with sonography. [18, 15]
Rong et al identified different ultrasound characteristics of Warthin tumors and pleomorphic adenomas. Grade 2 or 3 vascularity was identified in the majority of Warthin tumors (73.1%), whereas grade 0 or 1 vascularity was present in most of the pleomorphic adenomas (77.9%). In addition, cystic areas were identified in 45.2% of Warthin tumors but only 20.8% of pleomorphic adenomas. [27]
Although sonographic findings can suggest the diagnosis of pleomorphic adenoma in many small tumors, CT or MRI is needed to fully evaluate large tumors. Even in patients in whom the diagnosis is made by means of sonography and biopsy, CT or MRI is needed for preoperative planning.
-
Enhanced CT image shows a lobular mass in the left parotid gland. The circumscribed borders and location are highly suggestive of pleomorphic adenoma, which was confirmed with fine-needle aspiration.
-
Axial contrast-enhanced CT scan demonstrates a poorly enhancing mass (pleomorphic adenoma) involving the left submandibular gland. The mass is smoothly marginated and causes the gland to expand. Image courtesy of Dr Doug Phillips, Director of Neuroradiology, University of Virginia.
-
Coronal fat-saturated T2-weighted MRI demonstrates a hyperintense mass (pleomorphic adenoma) involving the deep lobe of the left parotid gland (arrow). The tumor has higher signal intensity than that of the visualized lymph nodes (arrowheads). This finding can help in distinguishing pleomorphic adenomas from intraparotid lymph nodes.
-
Contrast-enhanced T1- and T2-weighted MRIs in a patient with carcinoma ex pleomorphic adenoma. A large mass with a heterogeneous medial portion involves primarily the deep lobe of the parotid gland. The ill-defined anteromedial border, heterogeneous signal intensity, and enhancement, as well as the size of the tumor, all suggest the possibility of carcinomatous transformation. Image courtesy of Dr Linda Gray, Professor of Neuroradiology, Duke University.









