Practice Essentials
Parotid tumors are the most common of the salivary gland tumors, constituting 80% of all salivary gland tumors. Only about 20% of parotid tumors are malignant. Of the malignant tumors, the most common are mucoepidermoid carcinoma, adenoid cystic carcinoma, and squamous cell carcinoma. A history of prior squamous cell carcinoma, malignant melanoma, or malignant fibrous histiocytoma suggests intraglandular metastasis or metastasis to parotid lymph nodes. Prior parotid tumor most likely indicates a recurrence because of inadequate initial resection. [1, 2, 3, 4, 5, 6]
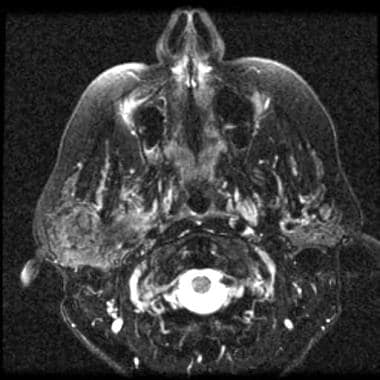
(See the image below.)
 Parotid, malignant tumors. Axial T1-weighted MRI demonstrates a low-signal-intensity mass in the left parotid gland. Pathology indicated mucoepidermoid carcinoma.
Parotid, malignant tumors. Axial T1-weighted MRI demonstrates a low-signal-intensity mass in the left parotid gland. Pathology indicated mucoepidermoid carcinoma.
Preferred examination
The initial imaging approach to tumor of the parotid region is ultrasonography preceded by clinical evaluation. When the diagnosis is in doubt, CT or MRI can help improve evaluation of the parotid gland surrounding tissues. The superficial lobe can be seen with high-frequency ultrasound, and US can help guide fine-needle aspiration, providing a high level of diagnostic accuracy and safety. On US, malignancy is suggested by an irregular shape, spiculated or ill-defined margins, a heterogeneous echotexture, vascularization, and large cervical lymphadenopathy. Ultrasonography has difficulty evaluating the deep lobe of the parotid gland because visibility of the deep lobe is obscured by the ramus of the mandible. For deep lobe examination, MRI is preferred. CT is the next best imaging choice if MRI is not available. [2, 5, 7, 8, 9]
MRI is the preferred imaging modality if a malignancy is suspected and the mass is palpable. Accuracy of MRI can be further increased with contrast enhancement, diffusion-weighted imaging, or apparent diffusion coefficient. However, MRI may not be available and can be expensive. CT is well suited for evaluating recurrent, tender parotid masses that can be inflammatory. The limitation of CT is radiation exposure. Plain radiographs and CT can provide the earliest demonstration of invasion. On CT or MRI, many malignant tumors, such as acinic cell carcinomas or low-grade mucoepidermoid carcinomas, appear indistinguishable from benign tumors, such as pleomorphic adenomas. [2, 4, 5, 10, 11, 12]
For final confirmation, fine-needle aspiration cytology or core-needle biopsy provides the highest accuracy. [2, 3, 4, 5, 13, 14, 15]
Multidisciplinary guidelines from the United Kingdom on the management of salivary gland tumors recommend ultrasonography-guided fine-needle aspiration cytology (FNAC) for diagnosis. According to the guidelines, nonhomogeneous muscle infiltration or suspicious regional lymph node appearance on cross-sectional CT or MRI suggests a malignancy. The main role of cross-secional imaging is to determine size, position, and relationship of tumors to adjacent structures. CT is useful in the case of a proven malignancy to exclude distant metastases. [3]
Radiography
Plain-film evaluation of the parotid gland is of limited clinical value. Radiographs can demonstrate sialolithiasis or involvement of the adjacent mandible. Views used to examine the parotid gland include open-mouth lateral images with an extended chin, posteroanterior images, and bilateral oblique images.
Sialography, or the injection of water-soluble contrast material into the Stensen duct, is used to demonstrate ductal anatomy or sialoliths.
CT is 10 times more sensitive than plain radiography in detecting small calcium deposits.
The sensitivity of sialography in detecting tumor is 85% at best, when performed by an experienced examiner. This rate is low compared with that of CT and MRI. Sialography is contraindicated or not recommended in the workup for a suspected malignant parotid tumor because some researchers believe that the pressure generated by the injection of contrast material can disseminate tumor cells. Sialography should be reserved for the diagnosis of inflammatory conditions.
Computed Tomography
CT findings of diffuse glandular calcifications suggest chronic sialadenitis, whereas calcifications within a mass are commonly seen in a pleomorphic adenoma. A solid mass is more easily differentiated from a cystic mass using CT rather than MRI. Although the facial nerve usually is not visualized on CT, the course of the nerve can be traced from the stylomastoid foramen. In addition, the Stensen duct usually is not seen unless it is dilated.
(See the images below.)
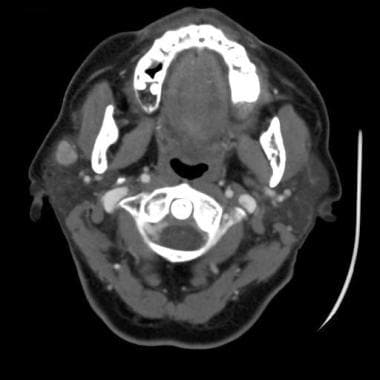 Parotid, malignant tumors. Contrast-enhanced neck CT scan demonstrates a well-circumscribed, enhancing mass in the superficial right parotid gland. Pathology indicated a low-grade adenocarcinoma.
Parotid, malignant tumors. Contrast-enhanced neck CT scan demonstrates a well-circumscribed, enhancing mass in the superficial right parotid gland. Pathology indicated a low-grade adenocarcinoma.
 Parotid, malignant tumors. Image shows a well-circumscribed mass in left parotid gland, which was proven to be a pleomorphic adenoma.
Parotid, malignant tumors. Image shows a well-circumscribed mass in left parotid gland, which was proven to be a pleomorphic adenoma.
 Parotid, malignant tumors. CT scan shows a carcinoma ex pleomorphic adenoma that developed after resection of the tumor (same patient as in the previous image).
Parotid, malignant tumors. CT scan shows a carcinoma ex pleomorphic adenoma that developed after resection of the tumor (same patient as in the previous image).
 Parotid, malignant tumors. Contrast-enhanced CT image of neck demonstrates a well-circumscribed, heterogeneously enhancing mass in the left parotid gland; this is a benign pleomorphic adenoma.
Parotid, malignant tumors. Contrast-enhanced CT image of neck demonstrates a well-circumscribed, heterogeneously enhancing mass in the left parotid gland; this is a benign pleomorphic adenoma.
 Parotid, malignant tumors. Axial contrast-enhanced CT scan shows an infiltrative mass involving the left parotid gland. Pathology indicated a parotid carcinoma.
Parotid, malignant tumors. Axial contrast-enhanced CT scan shows an infiltrative mass involving the left parotid gland. Pathology indicated a parotid carcinoma.
Degree of confidence
CT has advantages and limitations in imaging the parotid gland. Direct axial and coronal images can be obtained quickly in most patients; usually, only axial images are obtained. CT is superior in detecting heterotopic calcification or invasion of the mandible or skull base.
Dental-amalgam streak artifact can seriously degrade image quality; however, changing the gantry angle can reduce this degradation. In some patients with a dense parotid gland, a small tumor or diffuse cell infiltration cannot be detected. Furthermore, direct coronal images cannot be obtained in some patients who cannot extend their necks.
The CT appearance of benign and malignant tumors can overlap. A low-grade mucoepidermoid carcinoma can be cystic and contain calcifications, much like a pleomorphic adenoma. Higher-grade tumors tend to be more attenuating and more homogeneous.
Magnetic Resonance Imaging
Certain MRI characteristics can help differentiate benign parotid masses from malignant masses. A benign lesion usually is marginated smoothly, with a distinct border or capsule; however, many low-grade malignancies have a pseudocapsule and a benign radiographic appearance. High-grade malignancies have ill-defined infiltrating margins. [16, 17]
(See the images below.)
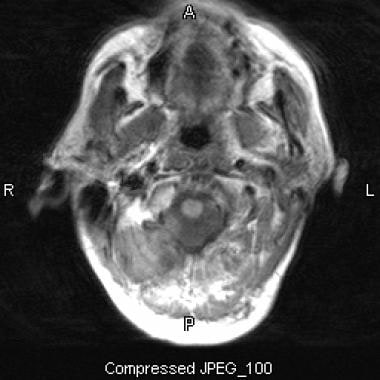
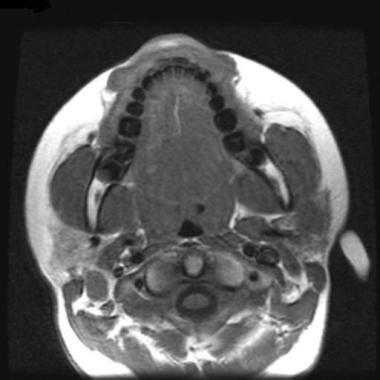 Parotid, malignant tumors. Axial T1-weighted MRI demonstrates a low-signal-intensity mass in the left parotid gland. Pathology indicated mucoepidermoid carcinoma.
Parotid, malignant tumors. Axial T1-weighted MRI demonstrates a low-signal-intensity mass in the left parotid gland. Pathology indicated mucoepidermoid carcinoma.
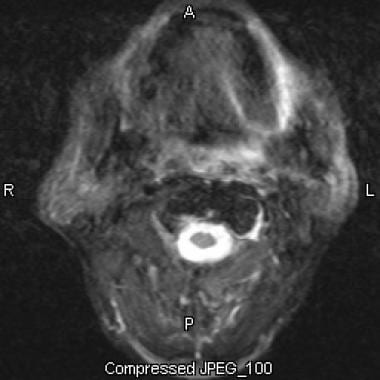
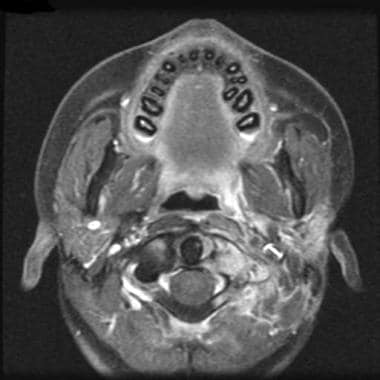 Parotid, malignant tumors. Axial T1-weighted MRI with fat saturation and contrast enhancement shows an infiltrative, enhancing mass involving the superficial and deep lobes of the left parotid gland. Pathology indicated a mucoepidermoid carcinoma.
Parotid, malignant tumors. Axial T1-weighted MRI with fat saturation and contrast enhancement shows an infiltrative, enhancing mass involving the superficial and deep lobes of the left parotid gland. Pathology indicated a mucoepidermoid carcinoma.
 Parotid, malignant tumors. Axial T1-weighted MRI with fat saturation and contrast enhancement shows an enhancing mass extending into the superficial and deep lobes of the right parotid gland. Pathology indicated a squamous cell carcinoma.
Parotid, malignant tumors. Axial T1-weighted MRI with fat saturation and contrast enhancement shows an enhancing mass extending into the superficial and deep lobes of the right parotid gland. Pathology indicated a squamous cell carcinoma.
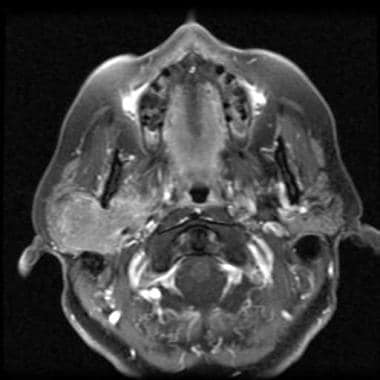
 Parotid, malignant tumors. Axial T2-weighted MRI shows relatively hypointense mass in the right parotid glands; this finding suggests malignancy. Pathology indicated a squamous cell carcinoma.
Parotid, malignant tumors. Axial T2-weighted MRI shows relatively hypointense mass in the right parotid glands; this finding suggests malignancy. Pathology indicated a squamous cell carcinoma.
In cases of a pleomorphic adenoma, T1-weighted images typically demonstrate intermediate signal intensity, with isointense-to-hyperintense signal on T2-weighted images. Contrast enhancement can be homogeneous or heterogeneous.
A Warthin tumor has homogeneous intermediate-to-hyperintense signal on T1-weighted images and intermediate signal intensity with focal hyperintense areas on T2-weighted images. Typically, these tumors are not contrast enhancing.
As a result of increased cellularity and decreased mucous production, high-grade malignancies tend to have low signal intensity with both T1- and T2-weighted sequences, whereas benign and low-grade malignancies are bright on T2-weighted images.
Common benign pleomorphic adenoma can evolve into malignant carcinoma ex pleomorphic adenoma or malignant mixed tumor. MRI can demonstrate the change from high T2 signal intensity with benign tumors to low-to-intermediate T2 signal with malignant tumors.
Degree of confidence
MRI is superior to CT in demonstrating tumor margins, and MRI is the procedure of choice for evaluating a nontender palpable parotid mass. Occasionally, the facial nerve or Stensen duct can be visualized. Common sequences are T1-weighted, T2-weighted, and inversion recovery fast spin-echo sequences.
MRI contrast agents are controversial and usually reserved for use when a palpable mass is not seen on a nonenhanced study. The use of contrast agents is indicated in evaluating the postoperative gland.
Low-grade mucoepidermoid carcinomas can appear identical to pleomorphic adenomas.
Ultrasonography
In the parotid gland, US is used to differentiate solid from cystic lesions. Parotid US uses a linear, high-frequency transducer (of 7-10 MHz) that provides high-resolution images. However, imaging depth is compromised. The deep lobe of the gland usually is not seen well. US often can be used to determine whether a lesion is intraglandular. The real-time capability of US makes it useful for guiding needle biopsy. [18, 19] It is frequently used for diagnostics of parotid tumors in countries where US is performed by the head and neck surgeons and can be combined with the clinical examination. [2]
On US, malignancy is suggested by an irregular shape, spiculated or ill-defined margins, a heterogeneous echotexture, vascularization, and large cervical lymphadenopathy. Ultrasonography has difficulty evaluating the deep lobe of the parotid gland because visibility of the deep lobe is obscured by the ramus of the mandible. For deep lobe examination, MRI is preferred. CT is the next best imaging choice if MRI is not available. [2, 5, 7, 8, 9]
Nuclear Imaging
The parotid and other salivary glands concentrate technetium-99m pertechnetate; however, nuclear medicine studies are not the preferred imaging modality for evaluating a parotid mass. Gallium-67 citrate, technetium-99m (99mTc) pertechnetate, and thallium-201 chloride have been used to evaluate parotid tumors.
Degree of confidence
Nuclear medicine studies lack the resolution to show bony invasion. Most malignant tumors are cold on scintigraphy.
In detecting malignant parotid tumors, gallium-67 citrate scanning has shown a sensitivity of 85% and a specificity of 38%. The low specificity is secondary to uptake by a pleomorphic adenoma.
Scanning with 99mTc pertechnetate has shown a 75% sensitivity and an 88% specificity for evaluating oncocytoma or Warthin tumor.
As a single test, cross-sectional imaging such as CT or MRI provides more information than scintigraphy.
With technetium, most tumors are relatively photopenic compared with the remainder of the gland and easily missed. Decreased activity in the gland is nonspecific and can represent benign or malignant neoplasm, metastasis, abscess, focal atrophy, or the changes of Sjogren syndrome. Two neoplasms—Warthin tumor and oncocytoma —concentrate pertechnetate and are seen easily.
-
Parotid, malignant tumors. Axial T1-weighted MRI demonstrates a low-signal-intensity mass in the left parotid gland. Pathology indicated mucoepidermoid carcinoma.
-
Parotid, malignant tumors. Axial T1-weighted MRI with fat saturation and contrast enhancement shows an infiltrative, enhancing mass involving the superficial and deep lobes of the left parotid gland. Pathology indicated a mucoepidermoid carcinoma.
-
Parotid, malignant tumors. Contrast-enhanced neck CT scan demonstrates a well-circumscribed, enhancing mass in the superficial right parotid gland. Pathology indicated a low-grade adenocarcinoma.
-
Parotid, malignant tumors. Axial T1-weighted MRI with fat saturation and contrast enhancement shows an enhancing mass extending into the superficial and deep lobes of the right parotid gland. Pathology indicated a squamous cell carcinoma.
-
Parotid, malignant tumors. Axial T2-weighted MRI shows relatively hypointense mass in the right parotid glands; this finding suggests malignancy. Pathology indicated a squamous cell carcinoma.
-
Parotid, malignant tumors. Image shows a well-circumscribed mass in left parotid gland, which was proven to be a pleomorphic adenoma.
-
Parotid, malignant tumors. CT scan shows a carcinoma ex pleomorphic adenoma that developed after resection of the tumor (same patient as in the previous image).
-
Parotid, malignant tumors. Contrast-enhanced CT image of neck demonstrates a well-circumscribed, heterogeneously enhancing mass in the left parotid gland; this is a benign pleomorphic adenoma.
-
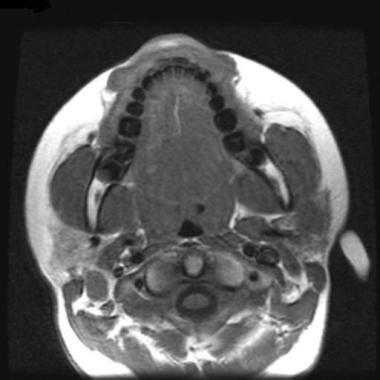
Parotid, malignant tumors. Axial T1-weighted MRI shows a left parotid carcinoma.
-
Parotid, malignant tumors. Axial T2-weighted MRI shows a left parotid carcinoma.
-
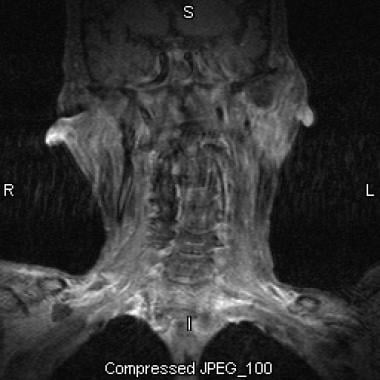
Parotid, malignant tumors. Coronal T2-weighted MRI shows a left parotid carcinoma.
-
Parotid, malignant tumors. Axial contrast-enhanced CT scan shows an infiltrative mass involving the left parotid gland. Pathology indicated a parotid carcinoma.