Practice Essentials
Pneumoconiosis is a lung disease that is caused by the inhalation and deposition of mineral dust, with asbestosis being a form of pneumoconiosis that is specifically caused by inhalation of asbestos fibers. Asbestos is the generic term used for the group of fibrous mineral silicates of magnesium and iron whose chemical and physical properties make it ideal for a variety of commercial and industrial uses. Asbestos is derived from the Greek word meaning inextinguishable. Its natural resistance to heat and fire, as well as its tensile strength, flexibility, and insulating properties, has led to its use in more than 3000 applications, including floor tiles, boiler and pipe insulation, roofing, and brake lining. [1, 2, 3]
Asbestos is classified into 2 groups, based on its physical properties: the serpentines, which tend to be wavy and long, and the amphiboles, which are straight and rodlike. The most important member of the serpentines is chrysotile, which makes up more than 90% of the asbestos used in the United States. The amphibole group includes crocidolite, amosite, and tremolite, which is often found as a contaminant of chrysotile ore.
Three major diseases are associated with asbestos exposure: asbestosis, lung cancer, and mesothelioma. Pleural plaques are the most common manifestation of exposure. This article focuses on asbestosis, which specifically refers to the bilateral, diffuse, interstitial fibrosis of the lungs caused by the inhalation of asbestos fibers. Imaging features of asbestosis are seen below.
Preferred examination
Chest radiography is the traditional modality used for the initial diagnostic evaluation of asbestosis. [4] "B" readings (standardized forms from the International Labour Organization, filled out by certified "B" readers to assess lung parenchymal and pleural abnormalities related to pneumoconiosis [5] ) often are performed on chest radiographs. These readings have little or no clinical utility. Conventional radiographs are relatively insensitive in the detection of early asbestosis and tend to underestimate the severity of disease. The chest radiograph is normal in 10-20% of patients with histologic evidence of asbestosis. The classic radiographic appearance of asbestosis is nonspecific, but the presence of ancillary findings, such as pleural plaques or diffuse pleural thickening, strongly suggests asbestos exposure as the cause.
High-resolution computed tomography (HRCT) scanning is more sensitive than conventional radiography in the detection of early or mild fibrosis, particularly in the subpleural zones. HRCT and standard resolution CT (SRCT) scanning are indicated in patients suspected of having asbestosis. HRCT scanning can define and detect alveolitis and fibrosis earlier than SRCT scanning can. SRCT scanning is essential for detecting lung cancer earlier than chest radiography can. HRCT scanning is excellent in defining lung parenchymal detail, whereas SRCT scanning images the entire lung and is therefore more likely to detect a malignancy. Individual HRCT scan findings are nonspecific, but the likelihood that the fibrosis is the result of asbestos exposure increases with the number of characteristic abnormalities observed and the presence of asbestos-related abnormalities, such as pleural disease. [6, 7, 8, 1, 9, 10, 11, 12, 13]
 Asbestosis. Posteroanterior chest radiograph reveals a few reticulonodular opacities at the lung bases consistent with mild asbestosis.
Asbestosis. Posteroanterior chest radiograph reveals a few reticulonodular opacities at the lung bases consistent with mild asbestosis.
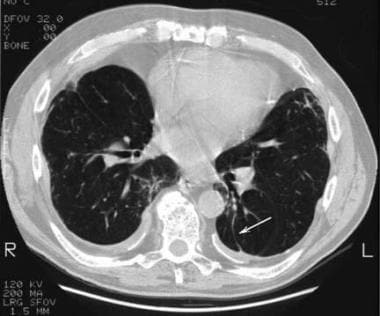
 Asbestosis. High-resolution CT scan through the lower lung zone nicely demonstrates thickened septal lines (white arrows) and small, rounded, subpleural, intralobular opacities (black arrow). Also note the calcified diaphragmatic pleural plaque on the left.
Asbestosis. High-resolution CT scan through the lower lung zone nicely demonstrates thickened septal lines (white arrows) and small, rounded, subpleural, intralobular opacities (black arrow). Also note the calcified diaphragmatic pleural plaque on the left.
The role of MRI in the diagnosis of asbestosis is limited. One study showed MRI to be more sensitive than chest radiography in the detection of subclinical asbestosis, [14] and another study found hat MRI compared favorably to CT scanning in the detection of asbestos-related pleural disease. [15]
Before HRCT gained popularity, gallium-67 scans were often helpful in diagnosing asbestosis in patients with appropriate clinical presentations but normal or equivocal chest radiographs. [7] Gallium-67 scans are usually positive in patients with asbestosis and may even provide a measure of inflammatory activity, because gallium-67 is believed to be engulfed by alveolar macrophages.
Radiography
The characteristic finding in asbestosis is the presence of small, irregular opacities, usually in the midlung and lower lung zones (see the images below). [16] According to the International Labour Organization classification, [17] "small irregular opacities" describe irregular, linear shadows that develop in the lung parenchyma and obscure normal bronchovascular markings. Asbestosis-related opacities are seen in the radiographs below. [1]
 Asbestosis. Posteroanterior chest radiograph reveals a few reticulonodular opacities at the lung bases consistent with mild asbestosis.
Asbestosis. Posteroanterior chest radiograph reveals a few reticulonodular opacities at the lung bases consistent with mild asbestosis.
 Asbestosis. Asbestosis and asbestos-related pleural disease in a 70-year-old man. Posteroanterior chest radiograph reveals prominent linear opacities at both bases, with obscuring of the cardiac borders and diaphragm. The thick, linear band at the right lateral base likely represents the subpleural, curvilinear opacities observed on high-resolution CT scans.
Asbestosis. Asbestosis and asbestos-related pleural disease in a 70-year-old man. Posteroanterior chest radiograph reveals prominent linear opacities at both bases, with obscuring of the cardiac borders and diaphragm. The thick, linear band at the right lateral base likely represents the subpleural, curvilinear opacities observed on high-resolution CT scans.
Stages of asbestosis progression
The progression of asbestosis is divided into 3 stages. In the first stage, a fine, reticular pattern may be seen, usually at the lung bases, in association with a ground-glass appearance, which may represent a combination of alveolitis and interstitial fibrosis.
The second stage is characterized by progression of the small, irregular opacities into a prominent interstitial pattern. During this stage, a combination of parenchymal and pleural abnormalities may partially obscure the heart border (shaggy heart sign; see the image below) and diaphragm.
 Asbestosis. Posteroanterior chest radiograph in a 54-year-old man with asbestosis demonstrates coarse, linear opacities at the bases more prominent on the left, obscuring the cardiac borders and diaphragm (shaggy heart border sign).
Asbestosis. Posteroanterior chest radiograph in a 54-year-old man with asbestosis demonstrates coarse, linear opacities at the bases more prominent on the left, obscuring the cardiac borders and diaphragm (shaggy heart border sign).
In the last stage, progression of the coarse interstitial pattern and honeycombing to the upper lung zones occurs; in addition, the heart and diaphragm are further obscured.
The radiographic findings described above are rather nonspecific, which may lead to a high false-positive rate. However, the presence of pleural abnormalities and of a compatible clinical history increases specificity in the diagnosis of asbestosis.
Estimates of the sensitivity of chest radiography in the detection of asbestos-related interstitial fibrosis vary widely, from 40-90%.
As previously mentioned, conventional radiographs are relatively insensitive in the detection of early asbestosis and tend to underestimate the severity of disease.
Computed Tomography
With its ability to show lung abnormalities not appreciated on conventional radiographs, CT scanning is considerably more sensitive than conventional radiography in the detection of asbestosis, especially in early or mild disease. As with radiography, CT scan findings in asbestosis are nonspecific, and the identification of a single abnormality is not diagnostic. [12, 13]
The advent of HRCT scanning has further improved the sensitivity of this modality. Common HRCT scan findings in early asbestosis are intralobular, small, rounded or branching opacities; thickened interlobular septa; subpleural curvilinear lines; and parenchymal bands. [18, 19] The interlobular septal lines typically represent fibrosis. With progression of disease, honeycombing is seen. [9, 10, 11]
Similar to the radiographic appearance, the findings on HRCT predominantly involve the subpleural regions of the lower lung zones. As most of the abnormalities seen in mild asbestosis may be confined to the posterior basal lung zones, the CT scan study should include images with the patient in the prone position to differentiate normal dependent parenchymal opacity from mild subpleural fibrosis. [8]
(CT scans of patients with asbestosis appear below.)
 Asbestosis. High-resolution CT scan through the midlung zone demonstrates a parenchymal band on the left (arrow).
Asbestosis. High-resolution CT scan through the midlung zone demonstrates a parenchymal band on the left (arrow).
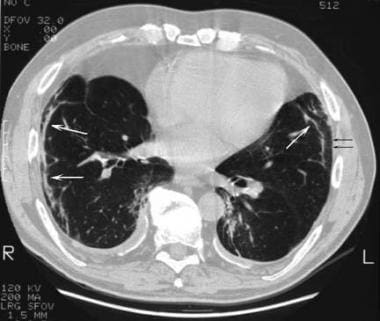 Asbestosis. High-resolution CT scan more inferiorly reveals subpleural, curvilinear opacities bilaterally (white arrows) and thickened interstitial lines (black arrows).
Asbestosis. High-resolution CT scan more inferiorly reveals subpleural, curvilinear opacities bilaterally (white arrows) and thickened interstitial lines (black arrows).
 Asbestosis. High-resolution CT scan through the lower lung zone nicely demonstrates thickened septal lines (white arrows) and small, rounded, subpleural, intralobular opacities (black arrow). Also note the calcified diaphragmatic pleural plaque on the left.
Asbestosis. High-resolution CT scan through the lower lung zone nicely demonstrates thickened septal lines (white arrows) and small, rounded, subpleural, intralobular opacities (black arrow). Also note the calcified diaphragmatic pleural plaque on the left.
On HRCT scans, the earliest lesions observed that indicate fibrosis are believed to be subpleural, intralobular, rounded or branching opacities that correspond to peribronchiolar fibrosis, the earliest microscopic finding. Theoretically, prior to fibrosis, a ground-glass appearance involving the air spaces may indicate alveolitis. Subpleural lines, which also are present early on, are curvilinear opacities observed parallel to and within 1 cm of the pleura. They are usually 5-10 cm long and likely represent a combination of peribronchiolar fibrosis and atelectasis.
Parenchymal bands are thick, linear opacities that are 2-5 cm long; they course through the lung and contact the pleural surface. These correspond to fibrosis along a bronchovascular sheath or interlobular septa with architectural distortion. Honeycombing is characterized by thick-walled, multiple, cystic spaces smaller than 1 cm in diameter.
One study assessing the accuracy of HRCT in asbestos-exposed individuals demonstrated 100% specificity when at least 3 of the abnormalities described above were present on the scans. [20] However, the exceptionally high specificity came at the expense of a decreased sensitivity (56% when 3 findings were present). The converse holds true as well: diagnosis based on 1 or 2 abnormalities increased sensitivity but decreased specificity.
Questions & Answers
Overview
What are the preferred modalities for asbestosis imaging?
What are the limitations chest radiography in asbestosis imaging?
What are the limitations HRCT scans in asbestosis imaging?
Which radiography findings are characteristic of asbestosis?
What are the radiographic stages of asbestosis progression?
Which HRCT scan findings are characteristic of asbestosis?
What is the degree of confidence in HRCT scanning for asbestosis?
What is the role of MRI in asbestosis imaging?
What is the role of gallium-67 scans in asbestosis imaging?
-
Asbestosis. Posteroanterior chest radiograph reveals a few reticulonodular opacities at the lung bases consistent with mild asbestosis.
-
Asbestosis. Posteroanterior chest radiograph in a 54-year-old man with asbestosis demonstrates coarse, linear opacities at the bases more prominent on the left, obscuring the cardiac borders and diaphragm (shaggy heart border sign).
-
Asbestosis. Asbestosis and asbestos-related pleural disease in a 70-year-old man. Posteroanterior chest radiograph reveals prominent linear opacities at both bases, with obscuring of the cardiac borders and diaphragm. The thick, linear band at the right lateral base likely represents the subpleural, curvilinear opacities observed on high-resolution CT scans.
-
Asbestosis. High-resolution CT scan through the midlung zone demonstrates a parenchymal band on the left (arrow).
-
Asbestosis. High-resolution CT scan more inferiorly reveals subpleural, curvilinear opacities bilaterally (white arrows) and thickened interstitial lines (black arrows).
-
Asbestosis. High-resolution CT scan through the lower lung zone nicely demonstrates thickened septal lines (white arrows) and small, rounded, subpleural, intralobular opacities (black arrow). Also note the calcified diaphragmatic pleural plaque on the left.









