Practice Essentials
Ovarian cancer is a silent killer; however, improvements in identification of women at high risk for ovarian cancer, as well as improved imaging techniques, have increased the likelihood of early detection. [1, 2, 3] Primary ovarian, fallopian tube, and peritoneal high-grade serous ovarian cancer (HGSOC high-grade serous ovarian cancer) is the most prevalent and lethal histologic subtype of epithelial ovarian cancer, partly because it is frequently diagnosed at advanced stages. [4]
Pelvic ultrasonography is the examination of choice, followed by magnetic resonance imaging (MRI) and/or computed tomography (CT) scanning. [5, 6, 7] The ovary may be difficult to delineate in some women who are postmenopausal, because of its relatively small size (< 2 × 2 cm), its position deep within the pelvis, and the lack of identifiable contained structures, such as cysts. [8, 9, 10, 11] Relatively simple ultrasound-based rules can be used to diagnose ovarian malignancy, such as the International Ovarian Tumor Analysis (IOTA) rules. [2, 3] The American College of Radiology, U.S. Preventive Services Task Force, American College of Obstetricians and Gynecologists, Society of Gynecologic Oncologists, and National Comprehensive Cancer Network have published guidelines on imaging for ovarian cancer (see Guidelines, below).
(See the images and video below.)
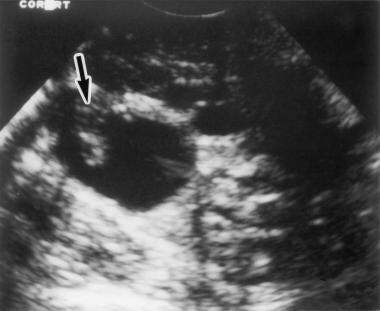 Transvaginal ultrasonogram shows the right ovary, which contains a cystic mass with a papillary excrescence (arrow). This finding is highly indicative of an ovarian neoplasm.
Transvaginal ultrasonogram shows the right ovary, which contains a cystic mass with a papillary excrescence (arrow). This finding is highly indicative of an ovarian neoplasm.
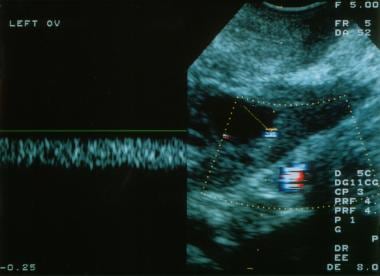
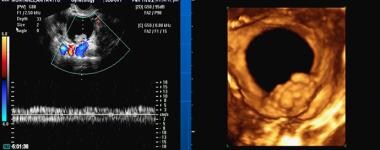
 Transvaginal, color Doppler ultrasonogram shows a solid mass in the left ovary. Low impedance flow is noted within this mass, which is a clear cell carcinoma of the ovary.
Transvaginal, color Doppler ultrasonogram shows a solid mass in the left ovary. Low impedance flow is noted within this mass, which is a clear cell carcinoma of the ovary.
Guidelines
Guidelines on ovarian cancer screening and diagnosis have been published by a number of professional medical organizations. Some are summarized below. [12, 13, 14, 15, 16, 17, 18]
American College of Radiology (ACR)
The ACR appropriateness criteria does not recommend that women at average risk for ovarian cancer receive screening imaging. Women at a high risk of ovarian cancer may benefit from screening. Pre- and postmenopausal women are considered to have a high risk of ovarian cancer if they have a personal or family history of ovarian cancer, have or are suspected to have BRCA1 or BRCA2 genetic mutations, or have an elevated CA-125 level (antigen 125—a protein elevated in cancer tumor cells) as measured by a blood test. The recommended imaging test to screen for ovarian cancer is ultrasound (US) to visualize the ovaries. These tests include transvaginal US (preferred), transabdominal US (in women who are not good candidates for transvaginal US), and US color Doppler (allows for visualization of blood flow). CT and MRI are usually not appropriate for screening women with either average or high risk of ovarian cancer. [12]
ACR appropriateness recommendations for evaluation of adnexal mass include the following [13] :
-
US duplex Doppler pelvis, US pelvis transvaginal, and US pelvis transabdominal are usually appropriate for the initial imaging of both premenopausal and postmenopausal women with a clinically suspected or likely adnexal mass and no acute symptoms. These examinations are complementary and should be performed together.
-
US pelvis transvaginal, US duplex Doppler pelvis, US pelvis transabdominal, and pelvic MRI without and with IV contrast are usually appropriate for the initial follow-up of premenopausal and postmenopausal women with indeterminate adnexal mass and no acute symptoms. These examinations are complementary and should be performed together.
-
The panel did not agree on recommending pelvic CT without and with IV contrast in postmenopausal patients with indeterminate adnexal mass and no acute symptoms. There is insufficient medical literature to conclude whether or not these patients would benefit from this procedure but it may be appropriate.
-
CT of the abdomen and pelvis with IV contrast and pelvic MRI without and with IV contrast are usually appropriate for the initial follow-up of patients with an adnexal mass, highly suspicious for malignancy, and no acute symptoms. These examinations are complementary and should be performed together.
-
The panel did not agree on recommending pelvic CT with IV contrast, pelvic CT without and with IV contrast, and US duplex Doppler of the pelvis in patients with an adnexal mass that is highly suspicious for malignancy and no acute symptoms. There is insufficient medical literature to conclude whether or not these patients would benefit from these procedures but they may be appropriate.
-
US duplex Doppler pelvis, US pelvis transabdominal, and US pelvis transvaginal are usually appropriate in the initial imaging and follow-up of pregnant patients with a clinically suspected adnexal mass and no acute symptoms. These examinations are complementary and should be performed together.
ACR appropriateness criteria for the initial staging of ovarian cancer recommends contrast-enhanced CT (with oral contrast) of the abdomen and pelvis as the imaging modality of choice, with inclusion of the chest where indicated. These examinations are complementary and should be performed together. Contrast-enhanced CT of the abdomen and pelvis (with oral contrast) or CT of the chest, abdomen, and pelvis are the modalities of choice for the extent of disease in suspected recurrence, and FDG-PET/CT is also usually appropriate, as it can provide management-changing information about unresectable sites of tumor or small lymph nodes. CT and FDG-PET/CT are considered equivalent alternatives. [14]
U.S. Preventive Services Task Force (USPSTF)
The U.S. Preventive Services Task Force (USPSTF) has concluded that annual screening of asymptomatic women with transvaginal ultrasonography and testing for a serum tumor marker, cancer antigen (CA)–125, does not reduce ovarian cancer deaths, but can lead to major surgical interventions in women who do not have cancer. With the harms of screening outweighing the benefits, USPSTF recommends against routine screening. [15]
The consensus among major medical organizations is in agreement with the USPSTF that screening for ovarian cancer in the general population is not recommended. However, the American College of Obstetricians and Gynecologists (ACOG) and the Society of Gynecologic Oncologists (SGO) recommend that women at high risk be offered an evaluation includes transvaginal ultrasonography, CA-125 testing, and a thorough pelvic examination. [19]
Society of Gynecologic Oncology and the American Society of Clinical Oncology
Guidelines from the Society of Gynecologic Oncology and the American Society of Clinical Oncology recommend that the primary clinical evaluation for ovarian cancer include a computed tomography (CT) scan of the abdomen and pelvis with oral and intravenous contrast, and chest imaging (CT preferred) to evaluate the extent of disease and the feasibility of surgical resection. [19]
National Comprehensive Cancer Network
National Comprehensive Cancer Network guidelines recommend chest x-ray or CT, as clinically indicated, and ultrasound and/or abdominal/pelvic CT or magnetic resonance imaging (MRI), as clinically indicated. Positron emission tomography (PET)/CT scan or MRI may be indicated for indeterminate lesions, if the results will alter management. [16]
MRI can increase the specificity of imaging evaluation in cases where the ultrasound appearance of the lesion is indeterminate. [ 8 ] MRI is not definitive, however. On MRI, endometriotic cysts with enhanced mural nodules are a hallmark of ovarian cancer, but they may also be a feature of benign neoplasms and even inflammatory diseases. Large contrast-enhanced nodules on large endometriotic cysts in an elderly patient are more likely to indicate malignancy. [17]
For patient education information, see the Cancer and Tumors Center, as well as Ovarian Cancer.
Computed Tomography
The primary use of CT scanning is in the evaluation of metastatic disease rather than of the ovarian mass; for the evaluation of the ovarian mass, ultrasonography and MRI are more valuable. [1] CT scanning is helpful in diagnosing cystic teratomas, 93% of which contain fat and 56% of which are calcified. If a large (>10 cm) soft-tissue mass is present, malignant transformation should be suspected. [20]
CT scanning also can aid in the evaluation of cystadenomas. A serous cystadenoma has an attenuation similar to that of water, whereas a mucinous cystadenoma has an attenuation closer to that of soft tissue.
The presence of wall and septal thickness and irregularity, as well as the existence of enhancing nodules, suggests malignancy. Although CT scan findings can suggest malignancy, they are not definitive for diagnosis unless metastases are present.
CT scan findings of complex functional cysts, benign ovarian tumors, and inflammatory and/or infectious masses, such as tubo-ovarian abscesses, can mimic ovarian malignancies.
Patients with a new diagnosis of epithelial ovarian cancer are routinely imaged with CT as a part of the initial work-up [4] , and CT is part of the standard of care in patients with high-grade serous ovarian cancer (HGSOC high-grade serous ovarian cancer), where it typically serves as a guide to surgical debulking and to assess response to chemotherapy. Because of frequent diagnosis of HGSOC high-grade serous ovarian cancer at the advanced stage, CT images typically display transcoelomic spread, usually over serosal and peritoneal surfaces. [21]
Magnetic Resonance Imaging
The primary advantage of using MRI in the evaluation of ovarian masses is the ability to employ this modality in the characterization of tissue. The presence of fat, hemorrhage, mucin, fluid, and solid tissue within an ovarian mass can be determined with the aid of MRI. The ability to characterize tissue in this way is most useful in determining whether a mass is definitely benign. [1, 9]
To determine the potential of malignancy for epithelial tumors, assessing the internal architecture is useful. In this situation, for example, gadolinium enhancement can be employed in the differentiation of solid papillary tissue (which can enhance) from clot or debris (which does not). Gadolinium enhancement is useful in the evaluation of the internal architecture of predominantly cystic lesions. In addition, if the mass is malignant, gadolinium enhancement may aid in the depiction of peritoneal implants.
Obtain images in at least 2 planes with T1- and T2-weighted sequences. [1]
For masses with high signal intensity on T1-weighted images, the addition of fat-saturated, T1-weighted images is useful in differentiating fat from hemorrhage. [1] If the signal intensity of a lesion is high on the T1-weighted image, the lesion can contain fat, hemorrhage, or mucin. If the lesion loses signal intensity after fat saturation, it contains fat; most likely, it is a cystic teratoma. If it does not lose signal, the lesion most likely contains hemorrhage, and it may represent an endometrioma or hemorrhagic cyst. Endometriomas are often dark on T2-weighted images. [22] In addition, high-viscosity mucin can be bright on T1-weighted images. Low-viscosity mucin is dark on T1-weighted images. [23]
If a lesion is dark on T1- and T2-weighted images, it may contain fibrotic tissue and be a fibroma. Consider a fibrothecoma or Brenner tumor.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or magnetic resonance angiography (MRA) scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
In a multivariate analysis, the accuracy of gadolinium-enhanced MRI in the diagnosis of ovarian malignancy was 93%. [24] The findings most predictive of malignancy were necrosis in a solid lesion (odds ratio, 107) and vegetations in a cystic lesion (odds ratio, 40). In addition, ancillary findings, such as ascites, peritoneal metastases, and hemorrhage, on MRI scans had a high predictive value for malignancy. The use of gadolinium-based contrast agents improves tissue characterization and increases the degree of confidence for MRI findings.
As with CT scans, MRI scans may depict numerous benign processes, such as complex functional cysts, tubo-ovarian abscesses, and benign tumors, that can mimic an ovarian malignancy.
Ultrasonography
Malignant ovarian tumors tend to have papillary excrescences, irregular walls, and/or thick septations. [5, 1, 25, 26, 27] The tumor can contain echogenic material arising from mucin or protein debris. The more solid the areas are, the greater the likelihood that a tumor is present. Typically, intraperitoneal fluid is present; this is a sign of peritoneal spread.
On color Doppler ultrasonograms, tumors tend to have vessels with low impedance because of the lack of muscular media in the vessel wall and arteriovenous shunts. The vessels tend to be clustered.
(See the images and video below.)
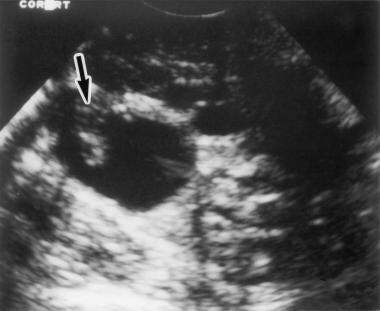 Transvaginal ultrasonogram shows the right ovary, which contains a cystic mass with a papillary excrescence (arrow). This finding is highly indicative of an ovarian neoplasm.
Transvaginal ultrasonogram shows the right ovary, which contains a cystic mass with a papillary excrescence (arrow). This finding is highly indicative of an ovarian neoplasm.
 Transvaginal and color Doppler ultrasonograms of stage I ovarian cancer. Top: Note the marked thickening and irregularity in the wall of this left adnexal cyst. Bottom: Color Doppler ultrasonogram shows very low impedance flow within the wall, which indicates an ovarian tumor.
Transvaginal and color Doppler ultrasonograms of stage I ovarian cancer. Top: Note the marked thickening and irregularity in the wall of this left adnexal cyst. Bottom: Color Doppler ultrasonogram shows very low impedance flow within the wall, which indicates an ovarian tumor.
 Transvaginal, color Doppler ultrasonogram shows a solid mass in the left ovary. Low impedance flow is noted within this mass, which is a clear cell carcinoma of the ovary.
Transvaginal, color Doppler ultrasonogram shows a solid mass in the left ovary. Low impedance flow is noted within this mass, which is a clear cell carcinoma of the ovary.
 Color Doppler ultrasonogram shows low impedance flow within the wall, which indicates an ovarian tumor.
Color Doppler ultrasonogram shows low impedance flow within the wall, which indicates an ovarian tumor.
The ultrasonographic finding that is most indicative of ovarian cancer is papillary excrescence, which is present in more than 50% of ovarian malignancies. Low impedance and clustered vessels have a 70-80% diagnostic accuracy. [7]
(See the images below.)
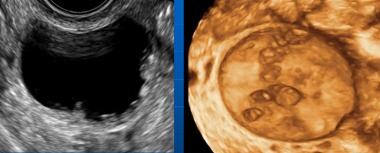 3D transvaginal sonography of ovarian cancer. Multiple papillary excrescences arising from the wall of a borderline serous cancer.
3D transvaginal sonography of ovarian cancer. Multiple papillary excrescences arising from the wall of a borderline serous cancer.
 3D transvaginal sonography of ovarian cancer. Multiple papillary excrescences with feeding vessels in a serous cystadencarcinoma.
3D transvaginal sonography of ovarian cancer. Multiple papillary excrescences with feeding vessels in a serous cystadencarcinoma.
 3D transvaginal sonography of ovarian cancer. Single sessile mural excrescence in a serous cystadenocarcinoma.
3D transvaginal sonography of ovarian cancer. Single sessile mural excrescence in a serous cystadenocarcinoma.
Tubo-ovarian abscesses may mimic the ultrasonographic appearance of ovarian cancer, but patients with abscesses typically present with symptoms that are attributable to an inflammatory process.
Studies evaluating contrast-enhanced transvaginal sonography (CE-TVS) have showed increased intensity at peak enhancement and longer transit time, reflecting the vascular network seen in malignant lesions. One meta-analysis that included over 8,000 women showed that CE-TVS had the highest sensitivity and specificity for detection of ovarian malignancy when compared to TVS and color Doppler ultrasonography. Labeled microbubbles have shown promise in distinguishing benign from malignant masses. [28, 29]
Questions & Answers
Overview
What are ovarian malignancies?
What are the NCCN guidelines on imaging for malignant ovarian tumors?
What is the role of imaging in the diagnosis of malignant ovarian tumors?
What are the USPSTF guidelines for ovarian cancer screening?
What are the SGO/ASCO guidelines on the primary evaluation for ovarian cancer?
What is the role of CT scanning in malignant ovarian tumor imaging?
What is the role of MRI in the diagnosis of malignant ovarian tumors?
Which ultrasound findings are characteristic of malignant ovarian tumors?
-
Transvaginal ultrasonogram shows the right ovary, which contains a cystic mass with a papillary excrescence (arrow). This finding is highly indicative of an ovarian neoplasm.
-
Transvaginal and color Doppler ultrasonograms of stage I ovarian cancer. Top: Note the marked thickening and irregularity in the wall of this left adnexal cyst. Bottom: Color Doppler ultrasonogram shows very low impedance flow within the wall, which indicates an ovarian tumor.
-
Transvaginal, color Doppler ultrasonogram shows a solid mass in the left ovary. Low impedance flow is noted within this mass, which is a clear cell carcinoma of the ovary.
-
Note the marked thickening and irregularity of the wall of this left adnexal cyst.
-
Color Doppler ultrasonogram shows low impedance flow within the wall, which indicates an ovarian tumor.
-
Three-dimensional, color Doppler ultrasonogram shows a cystic mass containing a vascular papillary excrescence; this is indicative of ovarian cancer.
-
3D transvaginal sonography of ovarian cancer. Multiple papillary excrescences arising from the wall of a borderline serous cancer.
-
3D transvaginal sonography of ovarian cancer. Multiple papillary excrescences with feeding vessels in a serous cystadencarcinoma.
-
3D transvaginal sonography of ovarian cancer. Single sessile mural excrescence in a serous cystadenocarcinoma.