Practice Essentials
Osteomyelitis is an infection of bone and bone marrow. It may be subdivided into acute, subacute, and chronic stages. Chronic osteomyelitis may appear as such at the initial presentation; not all patients show progression through the 3 phases. Rarely, a sclerotic nonpurulent form of osteomyelitis occurs; this is termed Garrès sclerosing osteomyelitis. Other related disorders are chronic recurrent multifocal osteomyelitis (CRMO), [1] tuberculous osteomyelitis, synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome. [2, 3, 4, 5, 6]
Osteomyelitis originates primarily from ulcer formation and soft tissue infection. The infection invades bone through the damaged skin or the broken bone cortex. Osteomyelitis can most often affect the forefoot and heel because they are the primary weight-bearing areas of the foot. Chronic osteomyelitis needs to be treated quickly and thoroughly; if not, the wound can persist, resulting in dysfunction, disability, or even amputation. [7, 8]
(See the images of osteomyelitis below.)
 Osteomyelitis, chronic. Sclerosing osteomyelitis of the lower tibia. Note the bone expansion and marked sclerosis.
Osteomyelitis, chronic. Sclerosing osteomyelitis of the lower tibia. Note the bone expansion and marked sclerosis.
 Osteomyelitis, chronic. Short-tau inversion recovery (STIR) MRIs show bone marrow edema of the clavicle and periclavicular fluid (pus).
Osteomyelitis, chronic. Short-tau inversion recovery (STIR) MRIs show bone marrow edema of the clavicle and periclavicular fluid (pus).
Chronic osteomyelitis is a severe, persistent, and sometimes incapacitating infection of bone and bone marrow. [9] It is often a recurring condition because it is difficult to treat definitively. This disease may result from the following:
-
Inadequate treatment of acute osteomyelitis
-
A hematogenous type of osteomyelitis
-
Trauma
-
Iatrogenic causes such as joint replacements and the internal fixation of fractures
-
Compound fractures
-
Infection with organisms, such as Mycobacterium tuberculosis and Treponema species ( syphilis)
-
Contiguous spread from soft tissues, as may occur with diabetic ulcers or ulcers associated with peripheral vascular disease
Cierny and Mader proposed an anatomic classification of chronic osteomyelitis [10] :
-
Type 1 — Endosteal or medullary lesion
-
Type 2 — Superficial osteomyelitis limited to the surface
-
Type 3 — Localized, well-marked legion with sequestration and cavity formation
-
Type 4 — Diffuse osteomyelitis lesions
According to the American College of Radiology (ACR), yhe initial study for suspected osteomyelitis should be a radiograph. If osteomyelitis is suspected but initial radiographs are normal or have findings suggestive of osteomyelitis, MRI is usually appropriate as the next imaging study. [11]
The Society of Skeletal Radiology (SSR) Practice Guidelines and Technical Standards Committee has recommended the term chronic osteomyelitis be used "if the marrow cavity demonstrates patchy areas of active disease and fibrosis, especially when coupled with features such as cortical remodeling, Brodie’s abscess, sequestrum, or sinus tract." [12]
Imaging modalities
Radiologic assessment of chronic osteomyelitis is performed for the following reasons: (1) to evaluate bone involvement (eg, the extent of active intramedullary infection or abscess superimposed on areas of necrosis, sequestrum and fibrosis) and (2) to identify soft tissue involvement (areas of cellulitis, abscess, and sinus tracts).
Plain radiographs are usually obtained initially. Ultrasonography may readily depict soft tissue involvement, but it provides only limited information about bone changes. [13, 14, 15, 16]
Because of its high sensitivity in the detection of bone marrow changes, MRI may provide detailed information regarding the extent and activity of the process by allowing the detection of the intramedullary site of infection and its complications. MRI may also be used to distinguish soft tissue involvement, allowing differential diagnosis. [17] With scintigraphy, other conditions not involving bone marrow, such as cellulitis and myositis, may cause errors; scintigraphy may be indicated for the assessment of local disturbances in vascular perfusion that are common in cases of chronic osteomyelitis. [18, 19, 20, 21, 22, 23]
Limitations of techniques
Although plain radiographs may provide important clues for diagnosis (eg, demonstration of bone remodeling, sclerosis, and thickening), the radiographic impression is often equivocal and relies heavily on clinical findings.
CT may depict intramedullary and soft tissue gas, sequestra, sinus tracts, and foreign bodies. However, CT scanning is insufficient for the assessment of the activity of the process.
MRI has limited availability, it is relatively expensive, and it is contraindicated in patients with certain implant devices and metallic clips. In addition, MRI is not tolerated by all patients with claustrophobia or morbid obesity, and young children may require sedation. Good MRIs require patient cooperation because patient motion degrades the images.
Radiography
For the detection of acute osteomyelitis, the sensitivity of plain radiography is less than 5% at presentation and about 33% at 1 week; however, the sensitivity is 90% 3-4 weeks after presentation. Stress fractures, osteoid osteomas, and other causes of periosteitis may mimic acute or chronic osteomyelitis.
Plain radiographic findings in acute or subacute osteomyelitis are deep soft tissue swelling, a periosteal reaction, cortical irregularity, and demineralization. The chronic phase of the disease is characterized by thick, irregular, sclerotic bone interspersed with radiolucencies, an elevated periosteum, and chronic draining sinuses. [24]
(See the radiographic images of chronic osteomyelitis below.)
 Osteomyelitis, chronic. Sclerosing osteomyelitis of the lower tibia. Note the bone expansion and marked sclerosis.
Osteomyelitis, chronic. Sclerosing osteomyelitis of the lower tibia. Note the bone expansion and marked sclerosis.
 Osteomyelitis, chronic. Image in a 56-year-old man with diabetes shows chronic osteomyelitis of the calcaneum. Note air in the soft tissues.
Osteomyelitis, chronic. Image in a 56-year-old man with diabetes shows chronic osteomyelitis of the calcaneum. Note air in the soft tissues.
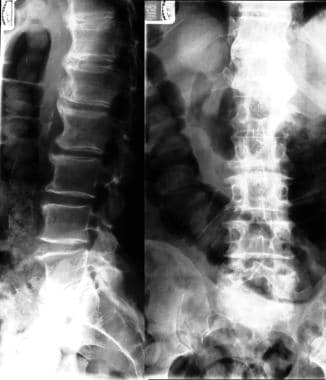
 Osteomyelitis, chronic. Radiograph (left) and isotopic bone scans (right) show sclerosing osteomyelitis of the tibia.
Osteomyelitis, chronic. Radiograph (left) and isotopic bone scans (right) show sclerosing osteomyelitis of the tibia.
 Osteomyelitis, chronic. Plain radiographs show Garrès sclerosing osteomyelitis. (See also the next image.)
Osteomyelitis, chronic. Plain radiographs show Garrès sclerosing osteomyelitis. (See also the next image.)
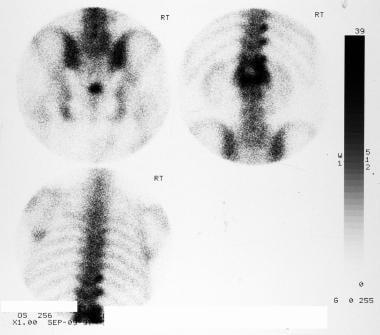
 Osteomyelitis, chronic. Technetium-99m diphosphonate bone scans show increased activity in the region with Garrès sclerosing osteomyelitis.
Osteomyelitis, chronic. Technetium-99m diphosphonate bone scans show increased activity in the region with Garrès sclerosing osteomyelitis.
Sclerosing osteomyelitis of Garré most commonly affects the mandible [25] and appears with a focal sclerosing periosteal reaction on radiologic studies.
Chronic recurrent osteomyelitis is a benign, self-limiting condition that primarily affects long bones in children and adolescents. [26] The metaphysis of long bones are usually affected; changes may be symmetrical. The appearances are those of confluent areas of bone lysis.
A Brodie abscess is a subacute osteomyelitis with a predilection for the ends of long bones and the carpus and tarsus. Plain radiographic findings include the following:
-
A central area of radiolucency with a surrounding thick rim of reactive bone sclerosis, which may persist for months
-
Pathognomonic tortuous parallel lucent channels extending toward the growth plate
-
A variable degree of periosteal new-bone formation
-
Associated soft tissue swelling
Computed Tomography
CT is of definite value for studying the entire articular surface of bone and periarticular soft tissues; for delineating the extent of medullary and soft tissue involvement; and for demonstrating cavities, serpiginous tracts, sequestra, or cloacae in osteomyelitis. [27, 28, 29]
CT may depict intramedullary and soft tissue gas, sequestra, sinus tracts, and foreign bodies. CT shows more sequestra than does the conventional method of investigation. An important advantage of CT is its ability to demonstrate lesions in the medulla and infections in the soft tissues. CT is the standard modality when looking for a sequestrum.
In the United Kingdom, CT is reserved for cases in which fistulae are present and when conventional methods with tomography leave problems unsolved. In the United States, conventional tomography is being used less often; it is being replaced by CT. However, CT is insufficient for assessing the activity of the disease process in chronic osteomyelitis.
One advantage of CT is that, for patients with acute osteomyelitis, it depicts changes earlier in the disease process than does plain imaging. CT is especially good for imaging the spine, the pelvis, and the sternum.
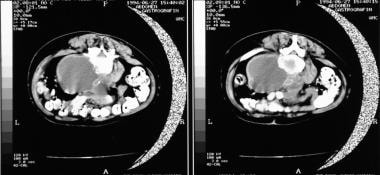
(See the CT scans of osteomyelitis below.)
CT scans sometimes show soft tissue edema or bone destruction not seen on plain images, particularly in the setting of acute osteomyelitis. Sclerosis, demineralization, and periosteal reactions are usually well depicted in chronic osteomyelitis. CT also helps in evaluating the need for surgery, and it provides vital information about the extent of disease. This information is helpful in planning appropriate surgery. CT is also an important modality in image-guided biopsy.
Stress fractures, osteoid osteomas, and other causes of periosteitis may mimic acute or chronic osteomyelitis.
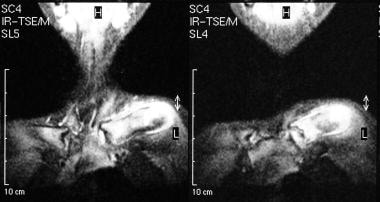
Magnetic Resonance Imaging
The sensitivity and specificity of MRI are higher than those of plain radiography and CT; MRI is particularly good at depicting bone marrow abnormalities. On MRI, marrow signal abnormality is more sensitive than lytic changes on plain images, and findings become positive earlier in the disease process with MRI than with radiography. Intramedullary bone pathology may be directly visualized with MRI; in marrow with osteomyelitis, these findings may precede bone changes.
One advantage of MRI is its multiplanar capability; because of this mutiplanar capability, MRI provides better anatomic detail and better soft tissue contrast. MRI is especially good in assessing vertebral osteomyelitis, which has a characteristic pattern of confluent vertebral body and disk involvement. The presence of titanium devices and other orthopedic devices usually poses no problem apart from causing artifacts.
However, MRI findings of osteomyelitis are nonspecific, and similar changes may occur as a result of tumors, fractures, and a variety of other intramedullary or juxtamedullary processes that may cause bone marrow edema. The sensitivity and specificity have been reported to be 92-100% and 89-100%, respectively. Previous fracture changes associated with surgery or the fracture itself are difficult to differentiate from infection. Fractures, bone bruises, and benign or malignant bone tumors may all mimic osteomyelitis.
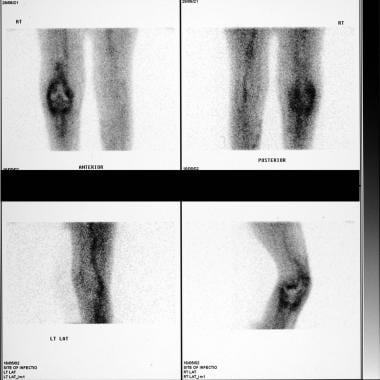
MRI findings in osteomyelitis usually are related to the replacement of marrow fat with water secondary to edema, exudate, hyperemia, and bone ischemia. Findings include the following: decreased signal intensity in the involved bone on T1-weighted images, increased signal intensity in the involved bone on T2-weighted image, and increased signal intensity in the involved bone on short-tau inversion recovery (STIR) images (see the image below). [17, 30, 31, 32, 33, 34, 35]
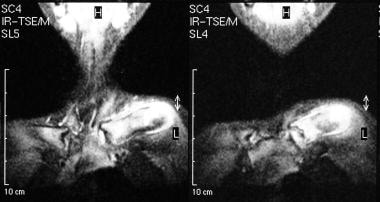 Osteomyelitis, chronic. Short-tau inversion recovery (STIR) MRIs show bone marrow edema of the clavicle and periclavicular fluid (pus).
Osteomyelitis, chronic. Short-tau inversion recovery (STIR) MRIs show bone marrow edema of the clavicle and periclavicular fluid (pus).
Sequestrum of cortical bone appears hypointense on T1-weighted, T2-weighted, and STIR MRIs and shows no gadolinium enhancement. Sequestrum of cancellous bone is hyperintense relative to cortical sequestrum on T1-weighted, T2-weighted, and STIR images and shows no gadolinium enhancement. The involucrum is hypointense on all 3 types of images and shows gadolinium enhancement.
Granulation tissue is hypointense on T1-weighted images and hyperintense on T2-weighted and STIR images. It shows gadolinium enhancement. Similarly, draining sinuses and soft tissue inflammation are hypointense on T1-weighted images and hyperintense on T2-weighted and STIR images; however, it does show gadolinium enhancement.
A Brodie abscess is characterized by a double line at the site of the lesion, caused by the high signal intensity of granulation tissue surrounded by low signal intensity of bone sclerosis on T2-weighted MRIs. The lesion has low to intermediate signal intensity that is outlined by a hypointense rim on T1-weighted MRIs.
Whole-body MRI is often used for diagnosis of chronic recurrent multifocal osteomyelitis (CRMO). [36, 37] CRMO is a polymorphic disorder in which whole-body MRI is beneficial to demonstrate subclinical edema. The mean age at diagnosis is 11 years (range, 3-17 yr). The most common sites are the long bone metaphysis, particularly femoral and tibial metaphysis; the pelvis, spine, clavicle, and mandible may also be involved. [38]
Gadolinium-based contrast agents such as gadopentetate dimeglumine, gadobenate dimeglumine, gadodiamide, gadoversetamide, and gadoteridol have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans.
Ultrasonography
The physical properties of bone do not usually lend themselves to ultrasonographic investigation, because of the reflection of sound waves at a soft tissue–bone interface. However, the periosteum, early new-bone formation, and soft tissue changes alongside dense bone may be imaged. There have been occasional reports of the use of sonography in cases of acute osteomyelitis, but its role in evaluating chronic osteomyelitis is probably limited.
Cleveland and Peck reported a case in which high-resolution ultrasonography was instrumental in establishing a diagnosis of chronic osteomyelitis. [39] Sonograms depicted a periosteal reaction and associated soft tissue involvement.
Larcos and associates found that 2 of 19 patients had a false-positive sonographic diagnosis of acute osteomyelitis. They concluded that ultrasonographic results might be potentially misleading, and they emphasized the importance of clinical judgment and role of other test results. [40]
High false-positive and false-negative rates are expected in cases of chronic osteomyelitis.
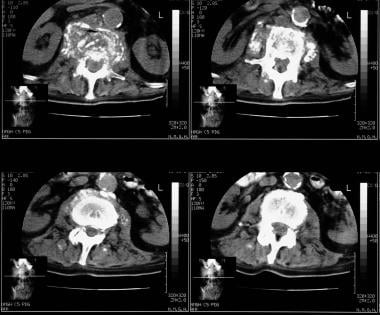
Nuclear Imaging
Technetium-99m diphosphonate bone scanning
Tc-99m methylene diphosphonate (MDP) bone scans are usually positive 24 hours after an acute infection, and the scans demonstrate a well-defined focus of tracer activity 1-2 hours after the injection. This finding is correlated with radiotracer in the same area on dynamic scans (see the images below). [41, 42]
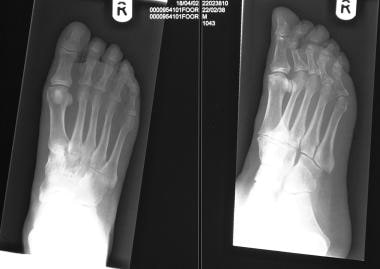 Osteomyelitis, chronic. Radiographs of the foot of a 52-year-old diabetic man with symptoms show no bone abnormality. (See also the next 2 images.)
Osteomyelitis, chronic. Radiographs of the foot of a 52-year-old diabetic man with symptoms show no bone abnormality. (See also the next 2 images.)
 Osteomyelitis, chronic. Radiographs of the foot of the same patient as in the previous image obtained 2 weeks later show patchy loss of bone density in the distal fourth metatarsal bone.
Osteomyelitis, chronic. Radiographs of the foot of the same patient as in the previous image obtained 2 weeks later show patchy loss of bone density in the distal fourth metatarsal bone.
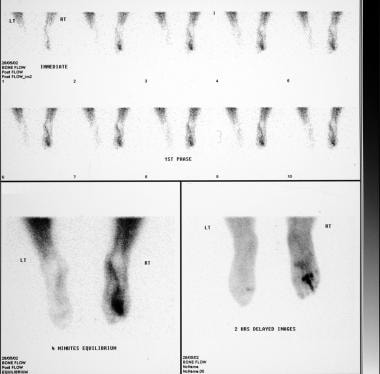 Osteomyelitis, chronic. Three-phase technetium-99m diphosphonate bone scans of the same patient as in the previous 2 images show increased activity in the third and fourth metatarsal bones and in the third toe.
Osteomyelitis, chronic. Three-phase technetium-99m diphosphonate bone scans of the same patient as in the previous 2 images show increased activity in the third and fourth metatarsal bones and in the third toe.
Bone scintigraphy may show focal uptake at the affected site. Osteomyelitis may be multifocal, and bone scintigraphy is particularly valuable in looking for other sites of infection.
MDP scans are positive in most patients with subacute and chronic osteomyelitis. Increased focal activity may persist in sterile disease for up to 2 years following successful therapy. (See the images below.)
 Osteomyelitis, chronic. A 20-year-old patient underwent intramedullary nail fixation of a tibial fracture 2 years before presenting with a painful leg. Radiographs show no evidence of osteomyelitis. (See also the next 5 images.)
Osteomyelitis, chronic. A 20-year-old patient underwent intramedullary nail fixation of a tibial fracture 2 years before presenting with a painful leg. Radiographs show no evidence of osteomyelitis. (See also the next 5 images.)
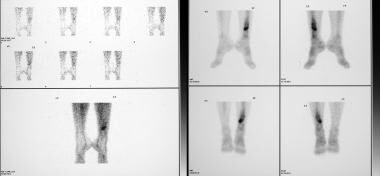 Osteomyelitis, chronic. Three-phase technetium-99m diphosphonate bone scans in the same patient as in the previous image and in the next 4 images show changes suggestive of osteomyelitis.
Osteomyelitis, chronic. Three-phase technetium-99m diphosphonate bone scans in the same patient as in the previous image and in the next 4 images show changes suggestive of osteomyelitis.
 Osteomyelitis, chronic. This 69-year-old man presented with epigastric pain. Plain radiograph of the lumbar spine shows changes of osteoarthritis (see also the next 3 images).
Osteomyelitis, chronic. This 69-year-old man presented with epigastric pain. Plain radiograph of the lumbar spine shows changes of osteoarthritis (see also the next 3 images).
 Osteomyelitis, chronic. Technetium-99m diphosphonate bone scan in the same patient as in the previous image and next image show increased activity in the upper lumbar spine.
Osteomyelitis, chronic. Technetium-99m diphosphonate bone scan in the same patient as in the previous image and next image show increased activity in the upper lumbar spine.
 Osteomyelitis, chronic. T1- and T2-weighted sagittal MRIs show bone marrow edema in L1 and obliteration of the disk space between L1 and L2. (See also the previous 5 images.)
Osteomyelitis, chronic. T1- and T2-weighted sagittal MRIs show bone marrow edema in L1 and obliteration of the disk space between L1 and L2. (See also the previous 5 images.)
MDP scans are highly sensitive, and the whole body may be imaged with a relatively low whole-body radiation dose. The sensitivity of MDP has variably been reported in the range of 32 to 100%, but the overall sensitivity is more than 90% in adults in the absence of complicating factors. Sensitivity is lower with earlier studies; in neonates; and in elderly persons with osteoporosis, severe peripheral vascular disease, and metabolic bone disease. The specificity is variably reported in the range of 0-100%.
The sensitivity of MDP scans may be improved by use of a 3-phase bone scan. On such scans, focal activity is usually associated with mild, diffusely increased, regional activity distal to the sight of osteomyelitis. Occasionally, photon deficient (cold) defects are seen.
Gallium-67 scanning
Mechanisms of 67Ga citrate uptake include the following: (1) direct leukocyte and bacterial uptake, (2) lactoferrin and transferring binding, (3) increased vascularity, and (4) increased bone turnover. [43, 44]
Criteria for a positive gallium scan include uptake exceeding that of the bone scan and/or uptake that differs in distribution in comparison to that on bone scans.
Johnson et al evaluated 22 diabetic patients with osteomyelitis by using gallium scans. The results yielded a sensitivity of 100%, a specificity of 40%, and an accuracy of 73%. In Schauwecker's review of the literature, the sensitivity was 81% and the specificity was 69%. [45]
Gallium scanning has a proven role in the monitoring of treatment.
If patients with suspected acute osteomyelitis are currently untreated and if 99mTc diphosphonate and gallium scans show concordant patterns, the scans are interpreted as follows:
-
If 99mTc diphosphonate uptake is less than gallium uptake, infection is suggested.
-
If 99mTc diphosphonate uptake is greater than gallium uptake, reactive bone is suggested.
-
If 99mTc diphosphonate and gallium uptake are discordant and if uptake is truly in bone, the likely diagnosis is osteomyelitis.
The sensitivity and specificity are 22-100% and 0-100%, respectively. Ga-67 scanning is more specific than MDP scanning, with relatively good images. Ga-67 is a better imaging agent in cases of chronic osteomyelitis; it is particularly good for imaging fungal infections. It also appears to be better than WBC for detecting vertebral osteomyelitis. The main disadvantages are its longer imaging time (72 hr), its higher radiation dose, and the fact that it is unsuitable for use in pediatric patients.
Indium-111 WBC
In-111 WBC scans may show normal lung uptake for up to 7 hours. At 24 hours, spleen activity greater than that in the liver and marrow is seen. Uptake is increased in cases of both acute and chronic osteomyelitis. Occasional cold (up to 12%) may occur in areas with significant red marrow, where uptake in the marrow is greater than that in the inflamed site. [46, 47, 48]
In-111–labeled WBCs are generally more specific than MDP or 67Ga and enable faster imaging than 67Ga scanning. The sensitivity is 83%, and the specificity is 94%. Previous antibiotic or steroid therapy does not affect the sensitivity. The disadvantages include the need for 50 mL of blood for labeling, its complicated formulation, and a higher radiation dose. Hence,111In techniques are not suitable for pediatric patients. The images are also relatively poor and may take up to 24 hours to acquire because of the low dosage.
Tc hexamethylenepropyleneamineoxime
Tc-99m hexamethylenepropyleneamineoxime (HMPAO) scanning is similar to 111In scanning, though more activity may be seen in other organs. The main advantages of 99mTc HMPAO WBC scanning are its faster imaging, its lower radiation dose, and the use of lower-energy photons for better images. Also, single-photon emission CT (SPECT) images may be obtained if required. The disadvantages include the need for phlebotomy, complicated labeling, and a "dirtier" image. The sensitivity and specificity are 95% and 85%, respectively.
2-[Fluorine 18]-fluoro-2-deoxy-D-glucose positron emission tomography
FDG is a nonspecific tracer that accumulates at sites of infection and inflammation. FDG PET imaging plays a major role in the treatment of patients with suspected infection and inflammation. PET has shown value in the diagnosis of chronic osteomyelitis, infected prostheses, and fever of unknown origin. Because of its ability to quantitate the rate of FDG uptake, PET may prove to be a powerful modality for monitoring disease activity and responses to therapy. Thus, the detection and characterization of infection and inflammation may become a major clinical indication in the day-to-day practice of PET imaging.
Meller and associates prospectively compared 111In-labeled WBCs with FDG by using a dual-head coincidence camera (DHCC) and found that FDG DHCC imaging was superior to 111In WBC scintigraphy for the diagnosis of chronic osteomyelitis in the central skeleton. During diagnostic workup, chronic osteomyelitis was proved in 11 of 36 regions of suspected skeletal infection and was subsequently excluded in 25. In addition, soft tissue infection was present in 5 patients, and septic arthritis was present in 3. In 28 patients, 111In WBC results were true-positive in 2 of 11 regions with proven chronic osteomyelitis; results were true-negative in 21 of 23 regions without further evidence of chronic osteomyelitis. False-positive results occurred in 2 regions, and false-negative results occurred in 9 regions suspected for chronic osteomyelitis. [49]
After studying applications of nuclear medicine techniques in children with peripheral bone osteomyelitis, Signore et al concluded that these techniques have the advantage of assessing the whole body in one session to determine multifocal involvement. [50]
Zhuang and associates examined 22 patients with possible osteomyelitis (5 cases involving the tibia, 5 involving the spine, 4 involving the proximal femur, 4 involving the pelvis, 2 involving the maxilla, and 2 involving the feet) who underwent FDG PET and in whom operative or clinical follow-up data were available; FDG PET correctly depicted the presence or absence of chronic osteomyelitis in 20 of 22 patients. FDG PET led to correct identification all 6 patients with chronic osteomyelitis but produced 2 false-positive results. [51]
In the study by Zhuang et al, the final diagnosis was made at surgical exploration or clinical follow-up during a 1-year period. Six patients had chronic osteomyelitis, and 16 did not have osteomyelitis. This study had a sensitivity of 100%, a specificity of 87.5%, and an accuracy of 90.9%. The authors concluded that FDG PET is a highly effective imaging method for excluding osteomyelitis when a negative scan is obtained. However, positive results are caused not only by osteomyelitis but also by inflammation in the bone or surrounding soft tissues as a result of other causes. Overall, FDG PET may prove to be the preferred study in the care of patients with possible chronic osteomyelitis. [51]
Bouter and his team studied the role of the chemokine receptor CXCR4 as a target in imaging of infectious and inflammatory diseases. They compared the results of 68Ga-Pentixafor-PET/CT against histologic and bacteriologic findings, as well as bone scintigraphy, white blood cell scintigraphy, and 18F-FDG-PET/CT. They concluded that 68Ga-Pentixafor-PET/CT was suitable for diagnosing chronic infections of the skeleton. [52]
Hulsen et al compared hybrid FDG PET/MRI to FDG PET/CT in the diagnosis and operative planning of chronic osteomyelitis in 5 patients with suspected chronic osteomyelitis in an extremity, and they found that FDG PET/MRI led to the same diagnosis and provided at least the same diagnostic information as PET/CT, but PET/MRI was able to provide additional soft tissue information. [53]
Leukocyte and marrow scintigraphy
Palestro and associates evaluated the role of combined leukocyte and marrow scintigraphy in the assessment of radiographically confirmed neuropathic or Charcot joints in 17 patients. [54] Studies demonstrating labeled leukocyte accumulation without corresponding activity on marrow images were classified as positive for osteomyelitis. Six patients also underwent 3-phase bone scintigraphy. Bone scans were interpreted as positive for osteomyelitis when focal hyperperfusion, focal hyperemia, and focal bony uptake were present on delayed images. [43, 54]
Bone images were also interpreted with labeled-leukocyte images by using 2 criteria for a positive study. One criterion was labeled-leukocyte activity in a region demonstrating abnormal activity on the bone scan, which was more intense than adjacent marrow activity or marrow activity in the corresponding region of the contralateral foot. The second criterion was either a spatially incongruent distribution of the 2 tracers or hyperintense activity on the leukocyte study, as compared to the bone scan.
The results showed that the leukocyte and marrow studies were positive for osteomyelitis in 4 of 20 neuropathic joints. Osteomyelitis was present in 3 joints, whereas in the fourth, infection was confined to overlying soft tissues. None of the 16 neuropathic joints with negative leukocyte and marrow scans were infected. In 1 patient who underwent below-the-knee amputation, histologic analysis confirmed hematopoietically active marrow, which corresponded to areas of congruent activity on the leukocyte and marrow images.
Three-phase bone scintigraphy was positive in all 6 neuropathic joints studied; osteomyelitis was present in 2. With the first criterion, leukocyte and bone imaging was also positive in all 6. With the second criterion, leukocyte and bone imaging was positive in the 2 infected neuropathic joints, as well as in 3 uninfected ones. Leukocyte and marrow scintigraphy was positive in both infected joints; it was negative in the 4 joints that were not infected.
The authors concluded that labeled-leukocyte accumulation in the uninfected Charcot joint does occur and is related, at least in part, to hematopoietically active marrow. They found that leukocyte and marrow scintigraphy was a reliable way to distinguish between marrow and infection as the cause of labeled-leukocyte accumulation in the neuropathic joint. In their series, the combination of leukocyte scintigraphy and bone scintigraphy was superior to both 3-phase bone scanning and leukocyte scintigraphy. [54]
Lichtenstein and associates examined 32 patients with fractures of the limbs 15-30 minutes after an injection of 99mTc sulfur colloid. [55] In 17 of 19 patients in whom osteomyelitis was superimposed on various fractures, significant uptake of sulfur colloid was noted at the fracture sites. The sensitivity for the test was 89.5%. In 12 of 13 cases in which osteomyelitis was absent, the sulfur colloid scan was negative, giving a specificity of 92.3%. Hence, 99mTc sulfur colloid scan may be a successful method for detecting osteomyelitis as a complication of a limb fracture.
Richter et al found that IgG antibody besilesomab (Scintimun) imaging is accurate, efficacious, and safe in the diagnosis of peripheral bone infections and that it provides information comparable to that of 99mTc HMPAO–labeled WBCs. [56]
Findings in chronic recurrent osteomyelitis
Bone scans may be positive for up to 2 years after treatment. In-111 WBC scanning is not ideal because mononuclear cells predominate. Although the sensitivity of 111In WBC scanning in an acute infection is in the range of 100%, the sensitivity decreases to 73% in chronic disease. Ga-67 scanning is probably more sensitive; with this method, activity returns to normal after effective treatment. [57]
Findings in infected hip and knee prostheses
The clinical presentation of a loose and infected prosthesis may be similar to that of osteomyelitis; hence, imaging plays an important role. Characteristically, MDP scans show normal flow and perfusion but increased focal activity at the tip or acetabulum in loosening. With infection, all phases are abnormal, and activity is present along the shaft of the prosthesis. A combined 67Ga and MDP scan may increase accuracy when 67Ga activity is more intense or incongruent. In-111 WBC scans are probably better in evaluating infected prostheses.
Findings in diabetic foot
In the diabetic foot, neuropathic osteoarthropathy and cellulitis may be confused with osteomyelitis. MDP scanning is sensitive but not specific.Ga-67 scans are more specific. In this setting,111In WBCs are superior scanning agents because there is no red marrow in the bones of the feet. Unlike MDP scans,111In WBC scans are not positive in neuropathic bones or joints. The sensitivity and specificity have been reported to be 100% and 83-79%, respectively.
-
Osteomyelitis, chronic. Sclerosing osteomyelitis of the lower tibia. Note the bone expansion and marked sclerosis.
-
Osteomyelitis, chronic. Sequestrum of the lower tibia.
-
Osteomyelitis, chronic. Image in a 56-year-old man with diabetes shows chronic osteomyelitis of the calcaneum. Note air in the soft tissues.
-
Osteomyelitis, chronic. Radiograph (left) and isotopic bone scans (right) show sclerosing osteomyelitis of the tibia.
-
Osteomyelitis, chronic. This 24-year-old man with psoriatic arthropathy presented with pain over the first metatarsal bone, hallux, and heel, with increased plasma viscosity. Radiographs of the right foot show a normal first metatarsal bone, but the cortex of the proximal phalanx of the hallux is irregular. (See also the next 3 images.)
-
Osteomyelitis, chronic. Three-phase technetium-99m diphosphonate bone scans (perfusion component) show increased activity in the whole of the heel, the tarsus, the proximal and distal phalanges of the hallux, and the proximal phalanx of the second toe.
-
Osteomyelitis, chronic. Three-phase technetium-99m diphosphonate bone scans (static component) show increased activity in the heel and in the first and second toes and in the fifth tarsotarsometatarsal joint.
-
Osteomyelitis, chronic. Nonenhanced axial CT scans through the first and second toes shows cortical irregularity of the distal phalanx of the hallux; this finding is suggestive of chronic osteomyelitis. The final diagnosis was osteomyelitis of the first and second toes, plantar fasciitis, and psoriatic arthritis of the fifth metatarsal-phalangeal joint.
-
Osteomyelitis, chronic. Plain radiographs show Garrès sclerosing osteomyelitis. (See also the next image.)
-
Osteomyelitis, chronic. Technetium-99m diphosphonate bone scans show increased activity in the region with Garrès sclerosing osteomyelitis.
-
Osteomyelitis, chronic. CT scans show vertebral osteomyelitis associated with a psoas abscess.
-
Osteomyelitis, chronic. Chest radiograph of a 12-year-old patient presenting with pain and swelling of the left clavicle. Note the expansion, sclerosis, and periosteal reaction of the clavicle. (See also the next 3 images)
-
Osteomyelitis, chronic. Conventional tomograms of the left clavicle of the same patient as in the previous image show the inflammatory lesion in the clavicle more clearly.
-
Osteomyelitis, chronic. Short-tau inversion recovery (STIR) MRIs show bone marrow edema of the clavicle and periclavicular fluid (pus).
-
Osteomyelitis, chronic. T1-weighted nonenhanced (top) and gadolinium-enhanced (bottom) axial MRIs show the enhancement at the inflammatory site in the clavicle. (See also the previous 3 images.)
-
Osteomyelitis, chronic. Radiographs of the foot of a 52-year-old diabetic man with symptoms show no bone abnormality. (See also the next 2 images.)
-
Osteomyelitis, chronic. Radiographs of the foot of the same patient as in the previous image obtained 2 weeks later show patchy loss of bone density in the distal fourth metatarsal bone.
-
Osteomyelitis, chronic. Three-phase technetium-99m diphosphonate bone scans of the same patient as in the previous 2 images show increased activity in the third and fourth metatarsal bones and in the third toe.
-
Osteomyelitis, chronic. Indium-111–labeled WBC scans show an infected right-knee prosthesis.
-
Osteomyelitis, chronic. A 20-year-old patient underwent intramedullary nail fixation of a tibial fracture 2 years before presenting with a painful leg. Radiographs show no evidence of osteomyelitis. (See also the next 5 images.)
-
Osteomyelitis, chronic. Three-phase technetium-99m diphosphonate bone scans in the same patient as in the previous image and in the next 4 images show changes suggestive of osteomyelitis.
-
Osteomyelitis, chronic. This 69-year-old man presented with epigastric pain. Plain radiograph of the lumbar spine shows changes of osteoarthritis (see also the next 3 images).
-
Osteomyelitis, chronic. Axial CT scans show destruction of L1. Note the air in the soft tissues.
-
Osteomyelitis, chronic. Technetium-99m diphosphonate bone scan in the same patient as in the previous image and next image show increased activity in the upper lumbar spine.
-
Osteomyelitis, chronic. T1- and T2-weighted sagittal MRIs show bone marrow edema in L1 and obliteration of the disk space between L1 and L2. (See also the previous 5 images.)