Practice Essentials
Osteomalacia is characterized by incomplete mineralization of normal osteoid tissue following closure of the growth plates. Osteomalacia may be part of the spectrum of osseous abnormalities that can be observed in patients with chronic renal insufficiency; this condition is referred to as renal osteodystrophy. Renal osteodystrophy combines features of secondary hyperparathyroidism, rickets, osteomalacia, and osteoporosis. Findings of rickets and osteomalacia occur in children, and findings of osteomalacia and secondary hyperparathyroidism occur in adults. Both too-high or too-low serum alkaline phosphatase (ALP) levels are important for diagnosis, [1, 2, 3, 4, 5, 6]
Clinically, osteomalacia is subtler than rickets, particularly in mild or moderate disease. Mildly affected patients may present with nonspecific bone pain and tenderness and possibly hypotonia. Severely affected patients may have difficulty ambulating and may walk with a waddling gait. Milkman syndrome is a condition in which the patient experiences multiple insufficiency fractures that are often bilateral and symmetric. [7] Typical sites include the concave surface of the femoral neck, axillary margin of the scapula, pubic rami, and ribs. Skeletal deformity can occur in the vertebral bodies and skull (basilar invagination), and fractures can occur in the vertebrae and long bones.
The immature skeleton may reveal the following characteristic findings:
-
In neonates, posterior flattening and squaring of the skull (eg, craniotabes) may be observed.
-
In older children, scoliosis, vertebral endplate deformities, basilar invagination of the skull, triradiate deformity of the pelvis, and slipped capital femoral epiphysis may be observed.
Renal osteodystrophy may also present with nonspecific signs and symptoms, including weakness, bone pain, and skeletal deformity. Presentation varies markedly with age. Adults may present with findings of osteomalacia, while children typically show growth retardation. As a result, complications differ depending on the patient's age. The most common complication of renal osteodystrophy is fracture, which may be insufficiency fractures through osteomalacic bone or pathologic fractures through brown tumors or amyloid deposits. Dialysis patients may experience carpal tunnel syndrome, osteomyelitis, septic arthritis, and osteonecrosis. Renal transplant patients may experience osteonecrosis, tendinitis, tendon rupture, and fracture. (See the images below.)
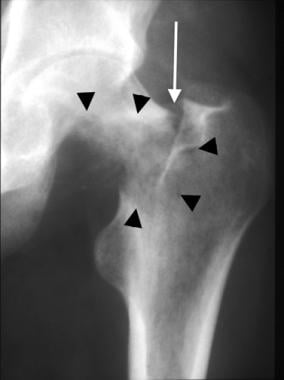 Anteroposterior radiograph of the hip in a dialysis patient reveals erosion of a large portion of the medial femoral neck and trochanteric region from amyloid deposition (arrowheads) with a pathologic fracture in the basocervical portion of the femoral neck (arrow).
Anteroposterior radiograph of the hip in a dialysis patient reveals erosion of a large portion of the medial femoral neck and trochanteric region from amyloid deposition (arrowheads) with a pathologic fracture in the basocervical portion of the femoral neck (arrow).
 Coronal T1-weighted MRI of the knee in a renal transplant patient on steroids reveals serpentine hypointensity in the metaphyseal and subchondral regions (black arrows) with secondary chondral collapse of the lateral femoral condyle (white arrow).
Coronal T1-weighted MRI of the knee in a renal transplant patient on steroids reveals serpentine hypointensity in the metaphyseal and subchondral regions (black arrows) with secondary chondral collapse of the lateral femoral condyle (white arrow).
Rickets and osteomalacia are different manifestations of the same underlying pathologic process, depending on whether the patient is a child or an adult, respectively. The demarcation is made at the time of closure of the growth plates. Renal osteodystrophy causes rachitic and some osteomalacic changes in the child and osteomalacia and secondary hyperparathyroidism in adults.
The ESRD patient profile in the United States, by age range, according to the US Renal Data System, is as follows [8] :
-
Younger than 21 years - 1.4% of patients
-
Ages 21-44 years - 14.6% of patients
-
Ages 45-64 years - 44.0% of patients
-
Ages 65-74 years - 23.8% of patients
-
Older than 74 years - 16.2% of patients
The histopathologic findings of renal osteodystrophy are commonly used to further classify the condition into high bone turnover states, such as osteitis fibrosa and hyperparathyroidism, and low bone turnover states, such as adynamic bone disease or heavy metal-induced osteomalacia. [9]
Imaging modalities
Radiographic examination in patients with osteomalacia may reveal only osteopenia. Bone dual energy x-ray absorptiometry (DEXA or DXA) scan usually shows decreased bone mineral density (BMD) because of decreased mineralization. [3] Characteristically, however, coarsened trabecula is observed. Complications such as Looser zones (see the image below) and complete fractures can be diagnosed radiographically. [10, 11]
 Magnified anteroposterior radiograph of the proximal tibia in a patient with chronic renal failure reveals a Looser fracture (pseudofracture) at the proximal medial tibia (arrow).
Magnified anteroposterior radiograph of the proximal tibia in a patient with chronic renal failure reveals a Looser fracture (pseudofracture) at the proximal medial tibia (arrow).
The findings of renal osteodystrophy diagnosed with conventional radiography include osseous resorption, soft tissue calcification, osteopenia, amyloid deposition, and fracture. [12]
Bone biopsy is considered the gold standard for diagnosis and classification of renal osteodystrophy. [13, 14]
Bone scans may reveal diffuse skeletal uptake of radiopharmaceutical with a superscan appearance that can be confused with metastatic disease. However, the extremities typically have a greater level of increased uptake with secondary hyperparathyroidism than is expected with metastatic disease. In addition, bone scans may reveal pseudofractures or sites of extraskeletal calcification, which also may be distinctive for secondary hyperparathyroidism. Bone scan findings usually are supportive of, but are of limited primary diagnostic value to, renal osteodystrophy. [3]
CT helps evaluate pathologic fracture. Amyloidosis may cause erosion in and around a joint, resulting in subtle radiographic signs that are more clearly delineated with cross-sectional imaging techniques such as CT. [15]
MRI helps evaluate the soft tissues for ligament rupture, and CT can help evaluate pathologic fracture. Amyloidosis may cause erosion in and around a joint, resulting in subtle radiographic signs, while amyloid deposits can be visualized directly on MRI. [15]
Radiographic usefulness in the diagnosis of hyperparathyroidism is limited because of the accuracy of current laboratory testing. However, secondary pathology may result from osteomalacic changes in the skeleton (eg, insufficiency fractures), and pathologic fractures may occur through a brown tumor. If this pathology is suggested (and may not be evident on radiographic studies), cross-sectional imaging may be warranted to exclude the findings.
Cross-sectional imaging may be needed to exclude hip fracture in a severely osteomalacic hip, similar to the imaging needed in older persons with osteoporosis. Substantial morbidity and mortality are associated with delayed diagnosis or misdiagnosis in these patients.
Differential diagnosis
The radiographic appearance of osteomalacia may be normal or similar to findings noted with osteoporosis. However, coarseness of the trabeculae may differentiate osteomalacia from osteoporosis. The differential diagnosis of generalized osteopenia includes osteomalacia, hyperparathyroidism, and multiple myeloma. [16]
The differential diagnosis of renal osteodystrophy varies depending on the sites of involvement. The causes of soft tissue calcification include collagen vascular disease, hydroxyapatite crystal deposition disease, hypervitaminosis, and idiopathic tumoral calcinosis.
Bone resorption in a periarticular distribution may resemble rheumatoid arthritis. Sacroiliac joint involvement by subchondral bone resorption resembles disease from ankylosing spondylitis and inflammatory bowel disease. Focal deposition of amyloid and brown tumors may resemble neoplasm. Diffuse spinal osteopenia may be a manifestation of multiple myeloma. A differential diagnosis for osseous sclerosis typically includes metastatic disease, sickle cell disease, radiation, myelofibrosis, mastocytosis, hypoparathyroidism, and Paget disease. (See the images below.)
 Anteroposterior radiograph of the distal forearm in a patient with chronic renal failure reveals an expansile lytic lesion (brown tumor) in the distal ulna (arrows).
Anteroposterior radiograph of the distal forearm in a patient with chronic renal failure reveals an expansile lytic lesion (brown tumor) in the distal ulna (arrows).
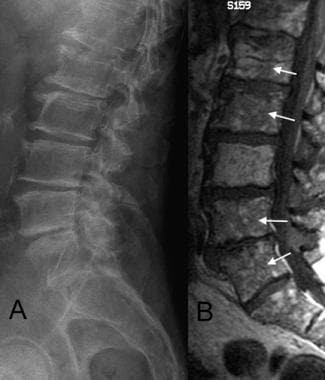 A. Lateral radiograph of the spine in a patient with multiple myelomas reveals diffuse osteopenia with no focal lesions. B. Sagittal T1-weighted MRI of the spine in the same patient reveals diffuse marrow replacement (arrows) indicative of diffuse myelomatoid involvement.
A. Lateral radiograph of the spine in a patient with multiple myelomas reveals diffuse osteopenia with no focal lesions. B. Sagittal T1-weighted MRI of the spine in the same patient reveals diffuse marrow replacement (arrows) indicative of diffuse myelomatoid involvement.
Chondrocalcinosis can be seen with pyrophosphate arthropathy, hemochromatosis, ochronosis, and gout. The differential diagnosis for rachitic changes includes hypophosphatasia and the Schmid type of metaphyseal chondrodysplasia.
Anatomy
Sclerosis may appear patchy and nonspecific, or it may show a characteristic pattern, such as predominant endplate involvement in the spine (see the images below). Soft tissue calcifications may take the form of the large, cloudlike collections in a periarticular distribution known as tumoral calcinosis. These collections are composed mostly of calcium hydroxyapatite and may form a milky substance that may contain fluid levels. Tumoral calcinosis typically is periarticular and noted frequently around the hips and shoulders, although it also may be found around smaller joints.
 Anteroposterior radiograph of the forefoot in a patient with chronic renal failure reveals diffuse osteosclerosis.
Anteroposterior radiograph of the forefoot in a patient with chronic renal failure reveals diffuse osteosclerosis.
 Lateral radiograph of the spine in a patient with chronic renal failure reveals characteristic endplate sclerosis (arrows) referred to as rugger-jersey spine.
Lateral radiograph of the spine in a patient with chronic renal failure reveals characteristic endplate sclerosis (arrows) referred to as rugger-jersey spine.
 Oblique radiograph of the hand in a dialysis patient reveals multifocal, large, amorphous calcific deposits (tumoral calcinosis) around the hand and wrist (arrows).
Oblique radiograph of the hand in a dialysis patient reveals multifocal, large, amorphous calcific deposits (tumoral calcinosis) around the hand and wrist (arrows).
Chondrocalcinosis may occur in fibrocartilage and hyaline cartilage and often occurs in the knee (see the images below). Other sites commonly affected by chondrocalcinosis include the pubic symphysis and triangular fibrocartilage of the wrist. Calcification also may occur in ligaments and tendons and in the vasculature.
 Anteroposterior radiograph of the knee in a patient with chronic renal failure reveals chondrocalcinosis of the meniscal fibrocartilage (white arrow) and articular hyaline cartilage (black arrow).
Anteroposterior radiograph of the knee in a patient with chronic renal failure reveals chondrocalcinosis of the meniscal fibrocartilage (white arrow) and articular hyaline cartilage (black arrow).
 Oblique radiograph of the wrist in a patient with chronic renal failure reveals chondrocalcinosis of the triangular fibrocartilage (arrow).
Oblique radiograph of the wrist in a patient with chronic renal failure reveals chondrocalcinosis of the triangular fibrocartilage (arrow).
 Lateral radiograph of the knee in a patient with chronic renal failure reveals calcification of the patellar tendon (arrows).
Lateral radiograph of the knee in a patient with chronic renal failure reveals calcification of the patellar tendon (arrows).
 Anteroposterior radiograph of the fingers in a patient with chronic renal failure reveals calcification of the vasculature (arrows), as well as resorption of the distal tufts (arrowheads).
Anteroposterior radiograph of the fingers in a patient with chronic renal failure reveals calcification of the vasculature (arrows), as well as resorption of the distal tufts (arrowheads).
Bone resorption typically is classified as subchondral, trabecular, endosteal, intracortical, subperiosteal, subligamentous, and subtendinous (see the images below). Involvement of the hands and feet by subperiosteal resorption typically occurs along the radial aspect of the middle phalanges and the cortical bone of the tufts of the distal phalanges. Subperiosteal resorption at the joint margins resembles marginal erosions of rheumatoid arthritis. Classically, the skull is affected by trabecular bone resorption, creating a salt-and-pepper appearance in the calvarium.
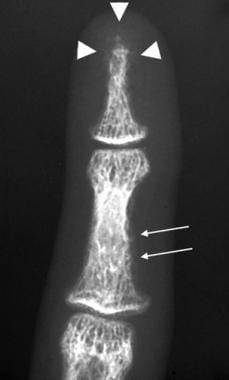 Anteroposterior radiograph of the finger in a patient with renal failure reveals subperiosteal resorption along the radial aspect of the middle phalanx (arrows), as well as resorption of the distal tuft (arrowheads).
Anteroposterior radiograph of the finger in a patient with renal failure reveals subperiosteal resorption along the radial aspect of the middle phalanx (arrows), as well as resorption of the distal tuft (arrowheads).
 Anteroposterior radiograph of the hand in a patient with chronic renal failure reveals subchondral and subperiosteal bone resorption predominating at the joint margins (arrows), which resembles the erosions of rheumatoid arthritis.
Anteroposterior radiograph of the hand in a patient with chronic renal failure reveals subchondral and subperiosteal bone resorption predominating at the joint margins (arrows), which resembles the erosions of rheumatoid arthritis.
 Lateral radiograph of the calvarium reveals punctate trabecular bone resorption that has a salt-and-pepper appearance.
Lateral radiograph of the calvarium reveals punctate trabecular bone resorption that has a salt-and-pepper appearance.
Subligamentous and subtendinous bone resorption typically occurs in the clavicle underlying the coracoclavicular ligaments, as well as at the calcaneal attachment of the plantar aponeurosis, the triceps insertion on the olecranon, the humeral tuberosities, the femoral trochanters, and the ischial tuberosities (see the images below). Subchondral bone resorption may be seen in locations that include the distal clavicles, sacroiliac joints, and pubic symphysis. Other characteristic sites involved by bone resorption include the proximal medial cortical surface of long bones and the lamina dura of the mandible.
 Anteroposterior radiograph of the shoulder in a patient with renal failure reveals subligamentous resorption underlying the clavicular attachment of the coracoclavicular ligament (white arrow) and subchondral erosion of the distal clavicle (black arrow).
Anteroposterior radiograph of the shoulder in a patient with renal failure reveals subligamentous resorption underlying the clavicular attachment of the coracoclavicular ligament (white arrow) and subchondral erosion of the distal clavicle (black arrow).
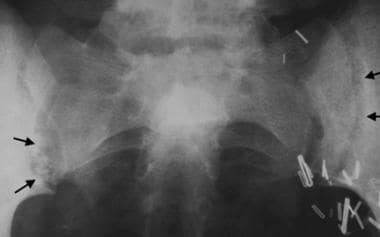 Anteroposterior radiograph of the sacroiliac joints reveals subchondral erosion at the articular surface bilaterally (arrows).
Anteroposterior radiograph of the sacroiliac joints reveals subchondral erosion at the articular surface bilaterally (arrows).
 Anteroposterior radiograph of the humerus in a patient with chronic renal failure reveals subperiosteal resorption at the proximal medial aspect of the bone (arrow).
Anteroposterior radiograph of the humerus in a patient with chronic renal failure reveals subperiosteal resorption at the proximal medial aspect of the bone (arrow).
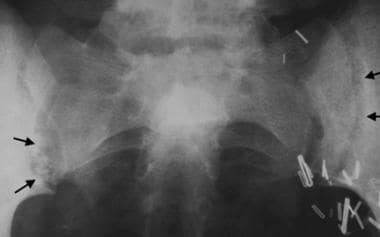
When renal osteodystrophy is encountered in children, rachitic changes and osteomalacia are the dominant findings (see the images below). Rachitic changes are apparent at the growth plates and include increased lucency, widening, elongation, irregularity, and cupping of the metaphyses. Changes of osteomalacia involve the mature trabecular bone. The parts of the skeleton affected most are the costochondral junctions of the middle ribs, distal femur, both ends of the tibia, distal radius and ulna, and proximal humerus.
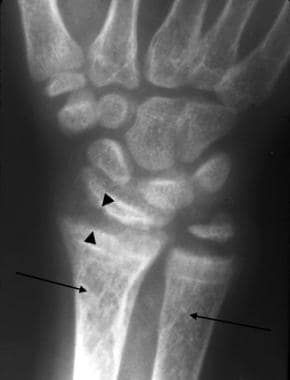 Anteroposterior radiograph of the wrist in a child with renal failure reveals cupping and fraying of the metaphysis and irregularity of the epiphyseal margins compatible with renal rickets (arrowheads). The coarsened trabeculae are a feature of osteomalacia (arrows).
Anteroposterior radiograph of the wrist in a child with renal failure reveals cupping and fraying of the metaphysis and irregularity of the epiphyseal margins compatible with renal rickets (arrowheads). The coarsened trabeculae are a feature of osteomalacia (arrows).
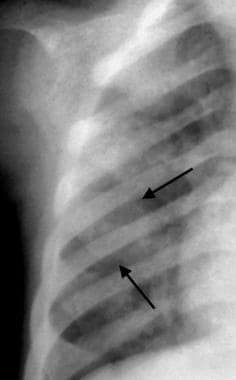 Anteroposterior radiograph of the right hemithorax in a child with chronic renal failure and rachitic rosary reveals abnormal widening of the anterior ribs at the costochondral junctions (arrows).
Anteroposterior radiograph of the right hemithorax in a child with chronic renal failure and rachitic rosary reveals abnormal widening of the anterior ribs at the costochondral junctions (arrows).
Pathophysiology
Renal osteodystrophy is a global term applied to all pathologic features of bone in patients with renal failure. The primary retention of phosphate by abnormal kidneys results in hyperphosphatemia, which causes hypocalcemia, resulting in secondary hyperparathyroidism. [17, 18] Therefore, the spectrum of clinical and radiographic findings in renal osteodystrophy may be a manifestation of any of these disorders.
Osteomalacia is a disorder of bone that results from hypomineralization following the cessation of bone growth. In contrast to rickets, which affects mineralization of growing bones, osteomalacia does not affect the growth plates; however, hypomineralization of trabecular and cortical bone occurs. [19, 20, 21, 22]
Normal bone mineralization depends on interdependent factors that supply adequate calcium and phosphate to the bones. Vitamin D maintains calcium and phosphate homeostasis through its action on bone, the GI tract, kidneys, and parathyroid glands. Vitamin D may be supplied in the diet or produced from a sterol precursor in the skin following exposure to ultraviolet light. Sequential hydroxylation is then required to produce the metabolically active form of vitamin D. Hydroxylation occurs first in the liver and then in the kidneys to produce 1,25-dihydroxyvitamin D3. Dysfunction in any one of these metabolic steps may result in rickets and osteomalacia in the growing child, as well as osteomalacia and secondary hyperparathyroidism in the adult.
The histopathology of osteosclerosis in renal osteodystrophy is complex and incompletely understood. Histologic evaluations of patients with renal osteodystrophy typically reveal osteoclastosis, osteoblastosis, and evidence of abnormally increased bone turnover. Additionally, an increased proportion of cancellous bone often exists. Calcium may be deposited in this cancellous bone as amorphous calcium phosphate rather than hydroxyapatite. This may help explain the increased osteosclerosis noted in some patients with renal osteodystrophy. Osteosclerosis also may be due to an increase in thickness and number of trabeculae in cancellous bone. Osteosclerosis is typically evident in areas with a large proportion of cancellous bone such as the spine. Osteosclerosis concentrated beneath the vertebral body endplates gives rise to the "P" appearance.
Bone resorption in renal osteodystrophy is also quite complex. Renal retention of phosphate results in hyperphosphatemia, which reduces serum ionized calcium levels, therefore inducing hyperparathyroidism. The hyperparathyroidism increases bone resorption, which may normalize serum calcium levels by releasing the osseous storage of calcium. The various sites of bone resorption include the subperiosteal region of the phalanges, the phalangeal tufts, proximal femur, proximal tibia, proximal humerus, distal clavicle, and calvarial trabeculae.
The cause of osteomalacia in renal osteodystrophy is multifactorial. The low serum calcium level directly induced by hyperphosphatemia is a major factor. Hyperphosphatemia also decreases the efficacy of 1-hydroxylase, which decreases the levels of 1-25 dihydroxyvitamin D and, thus, the ability of the gut to absorb calcium. [23]
Aluminum-induced bone disease is an additional cause of osteomalacia. Aluminum negatively affects bone formation through inhibition of osteoblastic activity, as well as by hydroxyapatite crystal formation. Aluminum may be introduced from dialysate solutions, antacids, or aluminum-containing phosphate-binding agents used to combat the hyperphosphatemia of renal failure.
Metastatic deposition causes soft tissue calcifications. Elevated phosphate levels may result in a high calcium-phosphate product causing deposits in the soft tissues. This also can be affected by the degree of alkalosis, as well as by local tissue injury. Areas that are particularly affected by soft tissue calcification include medium-sized blood vessels, periarticular soft tissues (tumoral calcinosis), and viscera such as the heart, lung, and kidney.
Isaksson et al studied iliac crest biopsies from healthy bone and from patients with renal osteodystrophy and hyperparathyroid disease to characterize the composition of bone in high-turnover renal osteodystrophy, by use of Fourier transform infrared spectroscopic imaging (FTIRI). The samples from the renal osteodystrophy patients showed significantly lower carbonate-to-phosphate and carbonate-to-amide I ratios, and spatial variation across the trabeculae established a significantly lower degree of mineralization at the edges of the trabeculae in the osteodystrophy samples. [24]
Tumor-induced osteomalacia (TIO)
Oncogenic (tumor-induced) osteomalacia (TIO) is a rare paraneoplastic syndrome associated with neoplasms that produce fibroblast growth factor-23 (FGF-23), which inhibits phosphate reabsorption in the kidneys; bone demineralization follows. Most of these are peripheral tumors, but it has been described with an intracranial tumor that mimics a meningioma on imaging; histologically, the tumor is a low-grade phosphaturic mesenchymal tumor, mixed connective tissue variant. [25, 2, 6]
The tumor's low prevalence, small size, and variable location often result in years of muscular weakness and bone pain before diagnosis. With complete treatment, symptoms swiftly dissipate. Niemeier et al reported a case of a 63-year-old previously healthy man with a 20-month history of musculoskeletal symptoms before diagnosis and resection of the posterior tibial tumor. Postoperatively, the patient returned to his previous lifestyle when an insufficiency fracture required a prophylactic stabilization. [26, 27]
In 2020, the US Food and Drug Administration approved Crysvita (burosumab-twza) injection to treat patients aged 2 years and older with tumor-induced osteomalacia. The drug is indicated for FGF23-related hypophosphatemia in tumor-induced osteomalacia associated with phosphaturic mesenchymal tumors that cannot be curatively resected or localized. The dosage is 0.5 mg SC every 4 weeks initially, which may be increased up to 2 mg/kg every 2 weeks, but not to exceed 180 mg/dose. [28]
Antiviral-induced osteomalacia
The long-term use of antiviral medications (eg, adefovir and tenofovir) to treat chronic hepatitis B and HIV infection has been reported to be associated with proximal renal tubular dysfunction resulting in significant hypophosphatemic osteomalacia. [29, 30, 31] Cases of low-dose adefovir-induced hypophosphatemic osteomalacia that initially presented with diffuse musculoskeletal pain have been reported. [21]
Radiography
Radiographic examination in patients with osteomalacia may reveal only osteopenia. Characteristically, however, coarsened trabecula is present. Complications such as Looser zones and complete fractures can be diagnosed radiographically. Findings of renal osteodystrophy diagnosed with conventional radiography include osseous resorption, soft tissue calcification, osteopenia, amyloid deposition, and fracture. [32, 33] (See the images below.)
 Magnified anteroposterior radiograph of the proximal tibia in a patient with chronic renal failure reveals a Looser fracture (pseudofracture) at the proximal medial tibia (arrow).
Magnified anteroposterior radiograph of the proximal tibia in a patient with chronic renal failure reveals a Looser fracture (pseudofracture) at the proximal medial tibia (arrow).
 Lateral radiograph of the leg in a child with chronic renal failure reveals anterior bowing of the distal tibia.
Lateral radiograph of the leg in a child with chronic renal failure reveals anterior bowing of the distal tibia.
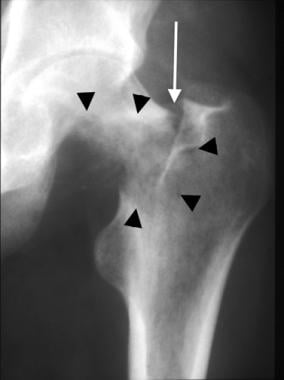 Anteroposterior radiograph of the hip in a dialysis patient reveals erosion of a large portion of the medial femoral neck and trochanteric region from amyloid deposition (arrowheads) with a pathologic fracture in the basocervical portion of the femoral neck (arrow).
Anteroposterior radiograph of the hip in a dialysis patient reveals erosion of a large portion of the medial femoral neck and trochanteric region from amyloid deposition (arrowheads) with a pathologic fracture in the basocervical portion of the femoral neck (arrow).
 Anteroposterior radiograph of the forefoot in a patient with chronic renal failure reveals diffuse osteosclerosis.
Anteroposterior radiograph of the forefoot in a patient with chronic renal failure reveals diffuse osteosclerosis.
 Lateral radiograph of the spine in a patient with chronic renal failure reveals characteristic endplate sclerosis (arrows) referred to as rugger-jersey spine.
Lateral radiograph of the spine in a patient with chronic renal failure reveals characteristic endplate sclerosis (arrows) referred to as rugger-jersey spine.
 Oblique radiograph of the hand in a dialysis patient reveals multifocal, large, amorphous calcific deposits (tumoral calcinosis) around the hand and wrist (arrows).
Oblique radiograph of the hand in a dialysis patient reveals multifocal, large, amorphous calcific deposits (tumoral calcinosis) around the hand and wrist (arrows).
 Anteroposterior radiograph of the knee in a patient with chronic renal failure reveals chondrocalcinosis of the meniscal fibrocartilage (white arrow) and articular hyaline cartilage (black arrow).
Anteroposterior radiograph of the knee in a patient with chronic renal failure reveals chondrocalcinosis of the meniscal fibrocartilage (white arrow) and articular hyaline cartilage (black arrow).
 Oblique radiograph of the wrist in a patient with chronic renal failure reveals chondrocalcinosis of the triangular fibrocartilage (arrow).
Oblique radiograph of the wrist in a patient with chronic renal failure reveals chondrocalcinosis of the triangular fibrocartilage (arrow).
 Lateral radiograph of the knee in a patient with chronic renal failure reveals calcification of the patellar tendon (arrows).
Lateral radiograph of the knee in a patient with chronic renal failure reveals calcification of the patellar tendon (arrows).
 Anteroposterior radiograph of the fingers in a patient with chronic renal failure reveals calcification of the vasculature (arrows), as well as resorption of the distal tufts (arrowheads).
Anteroposterior radiograph of the fingers in a patient with chronic renal failure reveals calcification of the vasculature (arrows), as well as resorption of the distal tufts (arrowheads).
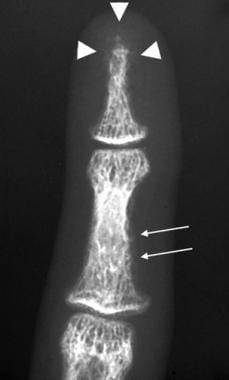 Anteroposterior radiograph of the finger in a patient with renal failure reveals subperiosteal resorption along the radial aspect of the middle phalanx (arrows), as well as resorption of the distal tuft (arrowheads).
Anteroposterior radiograph of the finger in a patient with renal failure reveals subperiosteal resorption along the radial aspect of the middle phalanx (arrows), as well as resorption of the distal tuft (arrowheads).
 Anteroposterior radiograph of the hand in a patient with chronic renal failure reveals subchondral and subperiosteal bone resorption predominating at the joint margins (arrows), which resembles the erosions of rheumatoid arthritis.
Anteroposterior radiograph of the hand in a patient with chronic renal failure reveals subchondral and subperiosteal bone resorption predominating at the joint margins (arrows), which resembles the erosions of rheumatoid arthritis.
 Lateral radiograph of the calvarium reveals punctate trabecular bone resorption that has a salt-and-pepper appearance.
Lateral radiograph of the calvarium reveals punctate trabecular bone resorption that has a salt-and-pepper appearance.
 Anteroposterior radiograph of the shoulder in a patient with renal failure reveals subligamentous resorption underlying the clavicular attachment of the coracoclavicular ligament (white arrow) and subchondral erosion of the distal clavicle (black arrow).
Anteroposterior radiograph of the shoulder in a patient with renal failure reveals subligamentous resorption underlying the clavicular attachment of the coracoclavicular ligament (white arrow) and subchondral erosion of the distal clavicle (black arrow).
 Anteroposterior radiograph of the sacroiliac joints reveals subchondral erosion at the articular surface bilaterally (arrows).
Anteroposterior radiograph of the sacroiliac joints reveals subchondral erosion at the articular surface bilaterally (arrows).
 Anteroposterior radiograph of the humerus in a patient with chronic renal failure reveals subperiosteal resorption at the proximal medial aspect of the bone (arrow).
Anteroposterior radiograph of the humerus in a patient with chronic renal failure reveals subperiosteal resorption at the proximal medial aspect of the bone (arrow).
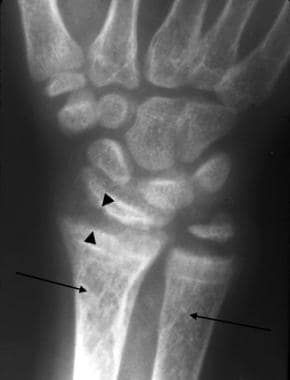 Anteroposterior radiograph of the wrist in a child with renal failure reveals cupping and fraying of the metaphysis and irregularity of the epiphyseal margins compatible with renal rickets (arrowheads). The coarsened trabeculae are a feature of osteomalacia (arrows).
Anteroposterior radiograph of the wrist in a child with renal failure reveals cupping and fraying of the metaphysis and irregularity of the epiphyseal margins compatible with renal rickets (arrowheads). The coarsened trabeculae are a feature of osteomalacia (arrows).
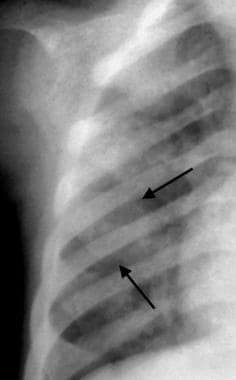 Anteroposterior radiograph of the right hemithorax in a child with chronic renal failure and rachitic rosary reveals abnormal widening of the anterior ribs at the costochondral junctions (arrows).
Anteroposterior radiograph of the right hemithorax in a child with chronic renal failure and rachitic rosary reveals abnormal widening of the anterior ribs at the costochondral junctions (arrows).
 Magnified anteroposterior radiograph of the proximal tibia in a patient with chronic renal failure reveals a Looser fracture (pseudofracture) at the proximal medial tibia (arrow).
Magnified anteroposterior radiograph of the proximal tibia in a patient with chronic renal failure reveals a Looser fracture (pseudofracture) at the proximal medial tibia (arrow).
 Anteroposterior radiograph of the distal forearm in a patient with chronic renal failure reveals an expansile lytic lesion (brown tumor) in the distal ulna (arrows).
Anteroposterior radiograph of the distal forearm in a patient with chronic renal failure reveals an expansile lytic lesion (brown tumor) in the distal ulna (arrows).
Magnetic Resonance Imaging
MRI helps evaluate soft tissues for ligament rupture and can evaluate pathologic fracture (see the image below). Amyloidosis may cause erosion in and around a joint, resulting in subtle radiographic signs, while amyloid deposits can be visualized directly on MRI.
Ultrasonography
Ultrasound provides a noninvasive, cost-effective, quick, repeatable, and portable modality in the diagnosis of renal osteodystrophy. Ultrasound is especially proficient at the evaluation of soft tissues, the parathyroid glands, and pathologic changes of the joints, as well as for detection of metastatic calcifications. [34]
Parathyroid glands are readily accessible for the detection of enlarged parathyroid gland in patients with secondary hyperparathyroidism; for the monitoring of pathologic changes; and for making decisions regarding the method of treatment on the basis of size and number of parathyroid glands. US can distinguish nodal from diffuse parathyroid hyperplasia and can provide a reliable method for obtaining a fine-needle aspiration biopsy.
Ultrasound can detect the pathologic changes associated with beta-2 amyloidosis, especially in the shoulder, which is most pronounced as rotator cuff thickness, hyperechoic amyloid deposits, and fluid in the joint. It can also be used for other joints and soft tissues for metastatic calcifications.
Quantitative bone ultrasound is based on different physical characteristics of the ultrasound, including transmission, speed of sound in m/sec, and broad-band attenuation in dB/MHz. These measures depend on the strength and architecture of the bones and can describe the changes in bone structure in dialysis patients by calculation of the Stiffness Index. The Stiffness Index is better than the standard bone densitometry by dual-energy x-ray absorptiometry, which only measures bone density. Combined ultrasound measurements of the bone in several locations may be successful in monitoring dialysis patients. [34]
Ultrasound is operator dependent, and bone penetration of the ultrasound beam has limitations, particularly in negotiating dense cortical bone. The differential diagnosis of bone resorption is wide.
Nuclear Imaging
Fluorine-18 (18F) fluorodeoxyglucose (FDG) positron emission tomography and computed tomography (18F FDG PET/CT) may reveal diffuse skeletal uptake of radiopharmaceutical with a superscan appearance that can be confused with metastatic disease. [35] However, the extremities typically have a greater level of increased uptake with secondary hyperparathyroidism than expected with metastatic disease. In addition, bone scans may reveal pseudofractures or sites of extraskeletal calcification, which also may be distinctive for secondary hyperparathyroidism.
In a cross-sectional study by Aaltonen et al, 26 patients on dialysis underwent a 18F-NaF (sodium fluoride) PET and a bone biopsy to measure bone turnover. On the basis of turnover-based classification of renal osteodystrophy, 12% had high turnover and 61% had low turnover bone disease. Using unified turnover-mineralization-volume (TMV)–based classification of renal osteodystrophy, 42% of patients had high turnover/hyperparathyroid bone disease and 23% had low turnover/adynamic bone disease. With unified TMV-based classification, 18F-NaF PET had an AUC of 0.86 in discriminating between hyperparathyroid bone disease and other types of renal osteodystrophy. [36]
-
Lateral radiograph of the leg in a child with chronic renal failure reveals anterior bowing of the distal tibia.
-
Anteroposterior radiograph of the hip in a dialysis patient reveals erosion of a large portion of the medial femoral neck and trochanteric region from amyloid deposition (arrowheads) with a pathologic fracture in the basocervical portion of the femoral neck (arrow).
-
Coronal T1-weighted MRI of the knee in a renal transplant patient on steroids reveals serpentine hypointensity in the metaphyseal and subchondral regions (black arrows) with secondary chondral collapse of the lateral femoral condyle (white arrow).
-
Anteroposterior radiograph of the forefoot in a patient with chronic renal failure reveals diffuse osteosclerosis.
-
Lateral radiograph of the spine in a patient with chronic renal failure reveals characteristic endplate sclerosis (arrows) referred to as rugger-jersey spine.
-
Oblique radiograph of the hand in a dialysis patient reveals multifocal, large, amorphous calcific deposits (tumoral calcinosis) around the hand and wrist (arrows).
-
Anteroposterior radiograph of the knee in a patient with chronic renal failure reveals chondrocalcinosis of the meniscal fibrocartilage (white arrow) and articular hyaline cartilage (black arrow).
-
Oblique radiograph of the wrist in a patient with chronic renal failure reveals chondrocalcinosis of the triangular fibrocartilage (arrow).
-
Lateral radiograph of the knee in a patient with chronic renal failure reveals calcification of the patellar tendon (arrows).
-
Anteroposterior radiograph of the fingers in a patient with chronic renal failure reveals calcification of the vasculature (arrows), as well as resorption of the distal tufts (arrowheads).
-
Anteroposterior radiograph of the finger in a patient with renal failure reveals subperiosteal resorption along the radial aspect of the middle phalanx (arrows), as well as resorption of the distal tuft (arrowheads).
-
Anteroposterior radiograph of the hand in a patient with chronic renal failure reveals subchondral and subperiosteal bone resorption predominating at the joint margins (arrows), which resembles the erosions of rheumatoid arthritis.
-
Lateral radiograph of the calvarium reveals punctate trabecular bone resorption that has a salt-and-pepper appearance.
-
Anteroposterior radiograph of the shoulder in a patient with renal failure reveals subligamentous resorption underlying the clavicular attachment of the coracoclavicular ligament (white arrow) and subchondral erosion of the distal clavicle (black arrow).
-
Anteroposterior radiograph of the sacroiliac joints reveals subchondral erosion at the articular surface bilaterally (arrows).
-
Anteroposterior radiograph of the humerus in a patient with chronic renal failure reveals subperiosteal resorption at the proximal medial aspect of the bone (arrow).
-
Anteroposterior radiograph of the wrist in a child with renal failure reveals cupping and fraying of the metaphysis and irregularity of the epiphyseal margins compatible with renal rickets (arrowheads). The coarsened trabeculae are a feature of osteomalacia (arrows).
-
Anteroposterior radiograph of the right hemithorax in a child with chronic renal failure and rachitic rosary reveals abnormal widening of the anterior ribs at the costochondral junctions (arrows).
-
Magnified anteroposterior radiograph of the proximal tibia in a patient with chronic renal failure reveals a Looser fracture (pseudofracture) at the proximal medial tibia (arrow).
-
Anteroposterior radiograph of the distal forearm in a patient with chronic renal failure reveals an expansile lytic lesion (brown tumor) in the distal ulna (arrows).
-
A. Lateral radiograph of the spine in a patient with multiple myelomas reveals diffuse osteopenia with no focal lesions. B. Sagittal T1-weighted MRI of the spine in the same patient reveals diffuse marrow replacement (arrows) indicative of diffuse myelomatoid involvement.
-
Radiograph of a 33-year-old woman on chronic hemodialysis shows a generalized reduction in bone density, associated with cortical thinning and coarsening of the trabecular pattern. Courtesy of Colonel Mobeen Shafique, FCPS, FRCR, Head, Department of Radiology, Combined Military Hospital, Pakistan.
-
Radiograph of a 33-year-old woman on chronic hemodialysis shows a generalized reduction in bone density, associated with cortical thinning and coarsening of the trabecular pattern. Pseudo-fractures/Looser zones are evident in the left lower femoral shaft and along the medial aspect of the left femoral neck (yellow arrows). There is bilateral protrusio acetabuli, which is a feature of bone softening (white arrow). There are multiple centrally compressed vertebral bodies giving a "cod fish" appearance. Scoliosis of the thoracic spine secondary to bone softening is noted. There is fairly extensive nephrocalcinosis related to secondary hyperparathyroidism (red arrows). Relative preservation of the vertebral end plates gives rise to a "Rugger Jersey" spine. Courtesy of Colonel Mobeen Shafique, FCPS, FRCR, Head, Department of Radiology, Combined Military Hospital, Pakistan.
-
Radiograph of a 33-year-old woman on chronic hemodialysis shows a generalized reduction in bone density, associated with cortical thinning and coarsening of the trabecular pattern. Radiographs of the knees show a pseudo-fracture (yellow arrow) and "brown cysts" (orange arrow). Also noted are coarse trabecular patterns. Courtesy of Colonel Mobeen Shafique, FCPS, FRCR, Head, Department of Radiology, Combined Military Hospital, Pakistan.







