Practice Essentials
Primary osteoarthritis is typically diagnosed on the basis of clinical and radiographic imaging findings. Radiographic findings may be normal in the early stages of the disease, because cartilage is not directly visualized. [1, 2, 3, 4, 5, 6, 7] Eventually, cartilage loss manifests as joint-space narrowing. Osteoarthritis, the most common type of joint disease, is a heterogeneous group of conditions that result in common histopathologic and radiologic changes. It is a degenerative disorder that results from the biochemical breakdown of articular cartilage in the synovial joints. Although osteoarthritis is thought to be largely due to excessive wear and tear, secondary nonspecific inflammatory changes may also affect the joints. By definition, the etiology of primary osteoarthritis is unknown, but the pathology and pathogenesis of osteoarthritis have been extensively studied. [8, 9, 10, 11, 12, 13, 14]
There is radiographic evidence of osteoarthritis in most individuals by 65 years of age and in about 80% of individuals older than 75 years. Osteoarthritis most commonly involves the hands, knees, feet, and facet joints of the spine and hips, with the knee being most commonly affected. [1, 15] The European League Against Rheumatism (EULAR) recommends plain radiography as the initial imaging modality for the assessment of knee or hand osteoarthritis. Findings on plain radiography include joint space narrowing, subchondral sclerosis, subchondral cysts, and osteophyte formation. [16, 17, 2] MRI may be helpful when the diagnosis is uncertain to evaluate surrounding joint structures. Compositional MRI is becoming more important because of its ability to assess premorphologic biochemical compositional changes of articular and periarticular tissues. Ultrasonography can be used to assess inflammatory changes such as osteophytes and joint effusions. [2, 18, 19, 3, 20, 21]
(Osteoarthritis is displayed in the images below.)
 Standing anteroposterior (AP) radiograph of the knees reveals bilateral medial femorotibial compartment narrowing and sharpening of the tibial spines; this finding is typical of osteoarthritis.
Standing anteroposterior (AP) radiograph of the knees reveals bilateral medial femorotibial compartment narrowing and sharpening of the tibial spines; this finding is typical of osteoarthritis.
 Posteroanterior (PA) radiograph of the hand reveals narrowing, osteophytes, and subchondral cysts affecting the distal interphalangeal joints; this finding is typical of osteoarthritis.
Posteroanterior (PA) radiograph of the hand reveals narrowing, osteophytes, and subchondral cysts affecting the distal interphalangeal joints; this finding is typical of osteoarthritis.
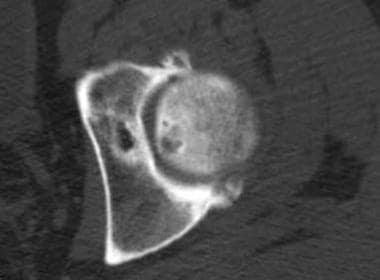 Transverse CT scan image obtained through the superior aspect of the hip reveals joint narrowing, osteophyte formation, and subchondral cysts typical of osteoarthritis.
Transverse CT scan image obtained through the superior aspect of the hip reveals joint narrowing, osteophyte formation, and subchondral cysts typical of osteoarthritis.
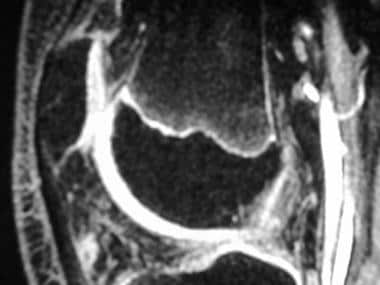
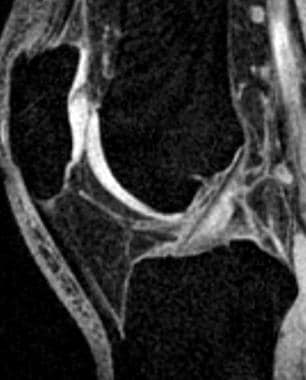
 Sagittal 3-dimensional gradient-echo fat-saturated MRI of the knee reveals full-thickness thinning of the articular cartilage of the lateral femoral condyle posteriorly with underlying degenerative subchondral marrow changes.
Sagittal 3-dimensional gradient-echo fat-saturated MRI of the knee reveals full-thickness thinning of the articular cartilage of the lateral femoral condyle posteriorly with underlying degenerative subchondral marrow changes.
 Spot delayed technetium-99m methylene diphosphonate (MDP) bone scintigram reveals focal increased radiotracer accumulation at the basilar joints and several interphalangeal joints (circles); this finding is compatible with osteoarthritis.
Spot delayed technetium-99m methylene diphosphonate (MDP) bone scintigram reveals focal increased radiotracer accumulation at the basilar joints and several interphalangeal joints (circles); this finding is compatible with osteoarthritis.
Although the progression of knee osteoarthritis is typically gradual, a subgroup of approximately 20% of patients develop accelerated knee osteoarthritis (AKOA), with rapid progression to advanced-stage disease in as little as 12 months. An analysis of data from the Osteoarthritis Initiative reported that 1 in 7 patients with AKOA received total knee replacement, with a median time of only 2.3 years from an increase in severity to knee replacement. [22, 23]
Historically, osteoarthritis has been divided into primary and secondary forms, although this division is somewhat artificial. Secondary osteoarthritis is conceptually easier to understand. It refers to degenerative disease of the synovial joints that results from some predisposing condition, usually trauma, that has adversely altered the articular cartilage and/or subchondral bone of the affected joints. Secondary osteoarthritis often occurs in relatively young individuals.
The definition of primary osteoarthritis is more nebulous. In the broadest sense of the term, primary osteoarthritis is an idiopathic phenomenon, occurring in previously intact joints, with no apparent initiating factor. Primary osteoarthritis is related to the aging process and typically occurs in older individuals. Some clinicians limit primary osteoarthritis to the joints of the hands (specifically the distal interphalangeal joints, proximal interphalangeal joints, and joints at the base of the thumb), whereas others include the knees, hips, spine (apophyseal articulations), and hands as potential sites of involvement.
The term primary or idiopathic osteoarthritis may become obsolete as underlying causes of osteoarthritis are discovered. For instance, many investigators believe that most cases of primary osteoarthritis of the hip may, in fact, be due to subtle or even unrecognizable congenital or developmental defects.
Imaging modalities
Radiographically, the erosions are centrally located, in contrast to the marginal erosions in rheumatoid arthritis. Osteophytes are present; consequently, interphalangeal joints may assume a gull-wing configuration, with central erosions flanked by raised lips of bone. Periarticular soft-tissue swelling is evident. Osseous fusion, which severely limits joint motion, may occur.
(See the images below.)
 Close-up radiograph of the fifth digit shows osteophytes and central erosions resulting in a "gull wing" appearance.
Close-up radiograph of the fifth digit shows osteophytes and central erosions resulting in a "gull wing" appearance.
 Close-up radiograph shows fusion of the distal interphalangeal (DIP) joint of the fifth finger; this finding is compatible with advanced erosive osteoarthritis.
Close-up radiograph shows fusion of the distal interphalangeal (DIP) joint of the fifth finger; this finding is compatible with advanced erosive osteoarthritis.
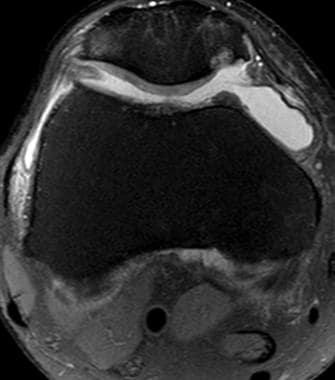
Chondromalacia patellae, which most commonly occurs in young adults, is a syndrome of crepitus and pain at the anterior knee associated with cartilaginous changes along the undersurface of the patella (see the image below). Conventional radiographs provide little information. Although arthrography enables a more direct assessment of cartilaginous integrity, many consider MRI to be the initial imaging study of choice.
 Transverse fast spin-echo T2-weighted fat-saturated MR image of the knee reveals increased signal intensity within the articular cartilage of the patella reflecting degeneration.
Transverse fast spin-echo T2-weighted fat-saturated MR image of the knee reveals increased signal intensity within the articular cartilage of the patella reflecting degeneration.
Fast spin-echo images (eg, fast spin-echo T2-weighted fat-suppressed images) or gradient-echo images (eg, T1-weighted 3-dimensional fat-suppressed images) can be used for the detection of cartilaginous ulceration, which is classically focal and located along the medial facet of the patella.
Radiologists may aid in the treatment of osteoarthritis by administering image-guided intra-articular injections of steroids. After the introduction of the needle into the joint and before steroid administration, aspiration of as much synovial fluid as possible should be attempted. This procedure often provides symptomatic relief for the patient and allows laboratory evaluation of the fluid, if necessary. Infected joint fluid and bacteremia are contraindications to steroid injection.
Radiography
Conventional radiographs remain the primary imaging modality for diagnosis of osteoarthritis. The diagnosis can be made with a high degree of confidence when joint narrowing, subchondral sclerosis, and osteophyte formation are seen. One important characteristic of primary osteoarthritis is that different abnormalities are found in the pressure (ie, contact) and nonpressure areas of the affected joint. In the highly stressed (ie, pressure) areas of the joint, radiographs can depict joint space loss, as well as subchondral bony sclerosis and cyst formation. In the areas without high contact pressures, osteophytes can be detected. Bilateral symmetry is often seen in cases of primary osteoarthritis, particularly when the hands are affected. [4, 5, 24, 25]
The European League Against Rheumatism (EULAR) recommends plain radiography as the initial imaging modality for the assessment of knee or hand osteoarthritis. Findings on plain radiography include joint space narrowing, subchondral sclerosis, subchondral cysts, and osteophyte formation. [16, 17]
With the onset of osteoarthritis, articular cartilage loses its smooth texture and becomes coarsened. This change leads to a sharp increase in frictional forces. Subsequently, cracks and tears, which lead to cartilage softening and flaking, are noted histologically. The net loss of articular cartilage appears as a reduction of the joint space on radiographs.
In major weight-bearing joints, a greater loss of joint space occurs at those areas subjected to the greatest pressures; this effect is in contrast to that of inflammatory arthritides, in which uniform joint-space narrowing is the rule. In the osteoarthritic knee, for example, one commonly observes the greatest loss of joint space in the medial femorotibial compartment (see the image below), although the lateral femorotibial compartment and patellofemoral compartment may also be affected. Collapse of the medial or lateral compartments may result in varus or valgus deformities, respectively. Hence, weight-bearing radiographs are preferred for evaluation of the osteoarthritic knee to depict such deformities, as well as to provide an accurate assessment of joint-space narrowing.
 Standing anteroposterior (AP) radiograph of the knees reveals bilateral medial femorotibial compartment narrowing and sharpening of the tibial spines; this finding is typical of osteoarthritis.
Standing anteroposterior (AP) radiograph of the knees reveals bilateral medial femorotibial compartment narrowing and sharpening of the tibial spines; this finding is typical of osteoarthritis.
Radiographs of the entire lower extremity (ie, load-line views) are also useful for demonstrating varus or valgus malalignment. Axial projections are best for evaluating the patellofemoral joint. When the patellofemoral compartment is involved (see the image below), the lateral facet of the patella is more frequently affected than the medial facet, and lateral patellar subluxation may be noted. Osteoarthritic changes of the patellofemoral articulation may be seen on lateral projections.
 Lateral radiograph of the knee reveals patellofemoral compartment narrowing and osteophytosis. A prominent Parson bump is also seen. Large ossified intra-articular bodies are evident.
Lateral radiograph of the knee reveals patellofemoral compartment narrowing and osteophytosis. A prominent Parson bump is also seen. Large ossified intra-articular bodies are evident.
In the osteoarthritic hip (see the image below), the superior aspect of the joint is typically the most narrowed; axial and medial migration of the femoral head is less commonly seen.
 Anteroposterior (AP) radiograph of the hip reveals severe superior migration of the femoral head (which reflects loss of articular cartilage), subchondral sclerosis, prominent osteophytes, and a large Egger cyst in the superior acetabulum. Mild flattening of the superior aspect of the femoral head is present.
Anteroposterior (AP) radiograph of the hip reveals severe superior migration of the femoral head (which reflects loss of articular cartilage), subchondral sclerosis, prominent osteophytes, and a large Egger cyst in the superior acetabulum. Mild flattening of the superior aspect of the femoral head is present.
In the small joints of the hand (see the image below), radiographs often show narrowing of the entire joint. In some cases, the interphalangeal joint may be asymmetrically affected, and radial or ulnar deviation at the joint may be appreciated; volar subluxation, as seen with rheumatoid arthritis, seldom occurs.
 Posteroanterior (PA) radiograph of the hand reveals narrowing, osteophytes, and subchondral cysts affecting the distal interphalangeal joints; this finding is typical of osteoarthritis.
Posteroanterior (PA) radiograph of the hand reveals narrowing, osteophytes, and subchondral cysts affecting the distal interphalangeal joints; this finding is typical of osteoarthritis.
Valgus deformity often accompanies osteoarthritis of the first metatarsophalangeal joint (see the image below).
 Radiograph of the foot reveals narrowing, subchondral sclerosis, and osteophyte formation affecting the first metatarsophalangeal joint. A mild valgus deformity is present as well.
Radiograph of the foot reveals narrowing, subchondral sclerosis, and osteophyte formation affecting the first metatarsophalangeal joint. A mild valgus deformity is present as well.
As the cartilage is worn away, friction causes the exposed subchondral bone to become smooth and polished, giving it a shiny surface (eburnation). The bone also becomes rebuttressed and sclerotic, a finding that is seen radiographically, generally after visible joint space narrowing occurs. As degeneration progresses, sclerosis becomes more marked, infiltrating deeper into the bone. Sclerosis is often the most prominent radiographic finding when osteoarthritis affects the facet joints of the spine (see the image below).
 Oblique projection demonstrates gradual narrowing and sclerosis of the facet joints as one progresses down the lumbar spine.
Oblique projection demonstrates gradual narrowing and sclerosis of the facet joints as one progresses down the lumbar spine.
Cyst formation is a fundamental radiographic finding in patients with osteoarthritis. Osteoarthritic cysts are also referred to as subchondral cysts, pseudocysts, or geodes, the preferred European term. These lesions are generally 2-20 mm in diameter. On radiographic examination, communication with the articular space may or may not be seen. Osteoarthritic pseudocysts in the acetabulum are termed Egger cysts. Later in the disease, the subchondral bone weakens and compresses; bony collapse may be seen radiographically. This finding is commonly seen in advanced cases of osteoarthritis of the hip, in which flattening of the superior aspect of the femoral head typically occurs.
The fundamental radiographic finding in the less-stressed areas of the osteoarthritic joint is osteophytosis. Osteophytes are mushroom-shaped bony outgrowths that are generally seen at the margins of the joint. These outgrowths are capped by cartilage that gradually ossifies. The osteophytes vary in size and may be smooth or jagged. In the knee, sharpening of the tibial spines and the more typical marginal osteophytes may be present (see the image below).
 Standing radiograph of the knee reveals narrowing of the medial and lateral femorotibial compartments with marginal osteophytes.
Standing radiograph of the knee reveals narrowing of the medial and lateral femorotibial compartments with marginal osteophytes.
A bony prominence, known as the Parson bump, may develop just anterior to the tibial spines (see the image below). Growth of osteophytes is one of the best indicators of disease progression. Fractured osteophytes result in intra-articular loose bodies. Flexed views (ie, tunnel views, skier views) of the knees often demonstrate these loose bodies particularly well.
 Lateral radiograph of the knee reveals patellofemoral compartment narrowing and osteophytosis. A prominent Parson bump is also seen. Large ossified intra-articular bodies are evident.
Lateral radiograph of the knee reveals patellofemoral compartment narrowing and osteophytosis. A prominent Parson bump is also seen. Large ossified intra-articular bodies are evident.
As stated previously, primary osteoarthritis is most commonly seen in the hands. Bilateral symmetry is generally observed, with multiple fingers on each hand affected. Heberden nodes refer to bony prominences at the distal interphalangeal joints, whereas similar bony outgrowths at the proximal interphalangeal joints are called Bouchard nodes. Although they are generally present simultaneously, Heberden nodes are more common.
On frontal radiographs, medial or lateral subluxation may accompany the wavy joint surface. In most patients with osteoarthritis of the interphalangeal joints, the first carpometacarpal joint is also affected, often with some degree of radial subluxation of the metacarpal. The scaphotrapezium and scaphotrapezoid joints may also be affected.
(See the images below.)
 Close-up radiograph of the wrist shows osteoarthritic changes at the first carpometacarpal joint, with severe narrowing and sclerosis of the trapezium-scaphoid and trapezoid-scaphoid (triscaphe) articulations.
Close-up radiograph of the wrist shows osteoarthritic changes at the first carpometacarpal joint, with severe narrowing and sclerosis of the trapezium-scaphoid and trapezoid-scaphoid (triscaphe) articulations.
Small joint effusions are not uncommon in osteoarthritic joints. Chondrocalcinosis and periarticular calcium hydroxyapatite deposition may also be seen. Mucinous cysts arise from the capsules of interphalangeal joints and may present radiographically as small periarticular soft-tissue masses.
Imaging pearls
Radiographic findings may be normal in the early stages of the disease, because cartilage is not directly visualized. Eventually, cartilage loss manifests as joint-space narrowing.
Primary osteoarthritis is most commonly seen in the hands.
Several radiographic grading systems have been proposed, but currently, no single system is adequate for evaluation of osteoarthritis at all joints.
The radiographic appearance of primary generalized osteoarthritis (PGOA) is indistinguishable from that of nonfamilial primary osteoarthritis, although the disease typically progresses relatively rapidly and appears severe on images.
In erosive (ie, inflammatory) osteoarthritis, the erosions are centrally located, in contrast to the marginal erosions in rheumatoid arthritis.
For chondromalacia patellae, conventional radiographs provide little information. Although arthrography enables a more direct assessment of cartilaginous integrity, many consider MRI to be the initial imaging study of choice.
Computed Tomography
CT is rarely used for the diagnosis of primary osteoarthritis, although it may be used for the diagnosis of malalignment of the patellofemoral joint or the foot and ankle joints. It may also be useful in evaluating the osseous detail of the vertebral column, particularly the facet joints.
(Osteoarthritis is displayed in the CT images below.)
 Transverse CT scan image obtained through the lower lumbar spine shows sclerosis of the facet joints.
Transverse CT scan image obtained through the lower lumbar spine shows sclerosis of the facet joints.
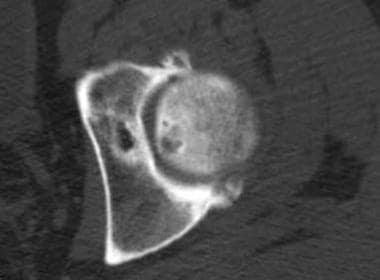 Transverse CT scan image obtained through the superior aspect of the hip reveals joint narrowing, osteophyte formation, and subchondral cysts typical of osteoarthritis.
Transverse CT scan image obtained through the superior aspect of the hip reveals joint narrowing, osteophyte formation, and subchondral cysts typical of osteoarthritis.
In patients who cannot tolerate MRI, CT scanning after the intra-articular injection of contrast material can be useful for the depiction of articular cartilage disease and the diagnosis of osteoarthritis or loose bodies in a variety of joints. CT is also well suited for the demonstration of hip joint osteoarthritis, but this examination is rarely ordered, except for preoperative planning.
Magnetic Resonance Imaging
Although MRI can depict many of the same findings of osteoarthritis as radiographs do, including joint narrowing, subchondral osseous changes, and osteophytes, radiographs remain the imaging method of choice in the diagnosis of osteoarthritis because they are more cost-effective than other methods and because they can be obtained more readily and quickly. [26, 27, 28, 29, 24]
Compositional MRI is becoming more important because of its ability to assess premorphologic biochemical compositional changes of articular and periarticular tissues. [18, 19, 20]
Fast spin-echo images (eg, fast spin-echo T2-weighted fat-suppressed images) or gradient-echo images (eg, T1-weighted 3-dimensional fat-suppressed images) can be used for the detection of cartilaginous ulceration, which is classically focal and located along the medial facet of the patella.
For chondromalacia patellae, conventional radiographs provide little information. Although arthrography enables a more direct assessment of cartilaginous integrity, many consider MRI to be the initial imaging study of choice.
Unlike radiography, MRI can depict articular cartilage directly; this feature of MRI has been the subject of multiple research studies over the past several years, particularly focusing on the cartilage of the knee (see the images below). A variety of pulse sequences have been described, but the most commonly used include spoiled gradient-recalled echo (SPGR) and fast spin-echo imaging.
 T1-weighted coronal MRI of the knee shows typical findings of osteoarthritis, including narrowing and subchondral changes at the medial femorotibial compartment and osteophyte formation.
T1-weighted coronal MRI of the knee shows typical findings of osteoarthritis, including narrowing and subchondral changes at the medial femorotibial compartment and osteophyte formation.
 Sagittal 3-dimensional gradient-echo fat-saturated MRI of the knee reveals normal hyperintense articular cartilage.
Sagittal 3-dimensional gradient-echo fat-saturated MRI of the knee reveals normal hyperintense articular cartilage.
 Sagittal 3-dimensional gradient-echo fat-saturated MRI of the knee reveals a full-thickness fissure of the articular cartilage of the patella.
Sagittal 3-dimensional gradient-echo fat-saturated MRI of the knee reveals a full-thickness fissure of the articular cartilage of the patella.
Three-dimensional gradient-echo images with fat saturation display the hyaline cartilage as high signal intensity tissue relative to bone, fat, and fluid. Abnormalities are seen as alterations of morphology of the normally bright cartilage—for example, fissuring or thinning. With intermediate- or T2-weighted fast spin-echo images, normal articular cartilage is of intermediate signal intensity. Cartilage abnormalities can be seen as regions of relatively increased intrasubstance signal intensity or as morphologic defects such as fissuring or thinning.
(See the images below.)
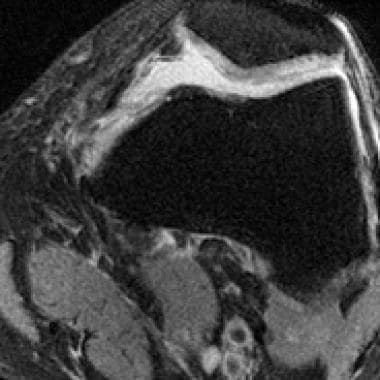
 Sagittal 3-dimensional gradient-echo fat-saturated MRI of the knee reveals full-thickness thinning of the articular cartilage of the lateral femoral condyle posteriorly with underlying degenerative subchondral marrow changes.
Sagittal 3-dimensional gradient-echo fat-saturated MRI of the knee reveals full-thickness thinning of the articular cartilage of the lateral femoral condyle posteriorly with underlying degenerative subchondral marrow changes.
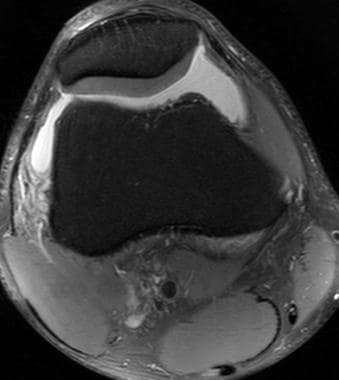 Transverse fast spin-echo T2-weighted fat-saturated MR image depicts normal intermediate signal intensity patellar cartilage well outlined against joint effusion.
Transverse fast spin-echo T2-weighted fat-saturated MR image depicts normal intermediate signal intensity patellar cartilage well outlined against joint effusion.
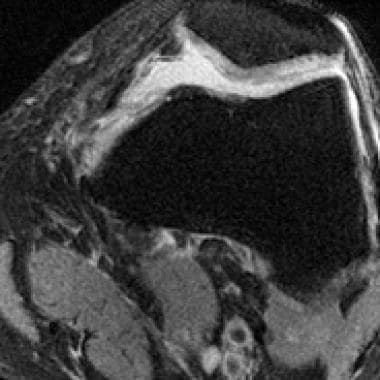 Transverse fast spin-echo T2-weighted fat-saturated MR image of the knee reveals increased signal intensity within the articular cartilage of the patella reflecting degeneration.
Transverse fast spin-echo T2-weighted fat-saturated MR image of the knee reveals increased signal intensity within the articular cartilage of the patella reflecting degeneration.
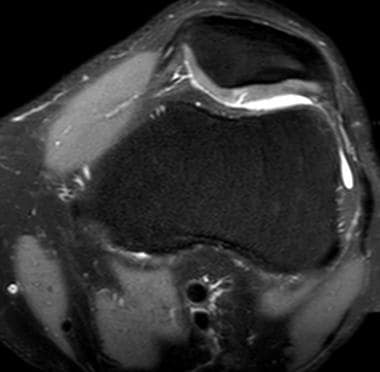 Transverse fat-suppressed fast spin-echo T2-weighted MR image reveals a fissure of the patellar cartilage filling with joint fluid.
Transverse fat-suppressed fast spin-echo T2-weighted MR image reveals a fissure of the patellar cartilage filling with joint fluid.
 Transverse fat-suppressed fast spin-echo T2-weighted MR image reveals a full-thickness defect of the articular cartilage along the medial facet of the patella with underlying degenerative subchondral marrow changes.
Transverse fat-suppressed fast spin-echo T2-weighted MR image reveals a full-thickness defect of the articular cartilage along the medial facet of the patella with underlying degenerative subchondral marrow changes.
Several systems have been advocated for use in the grading of focal cartilage change; however, a simple description of the extent of disease (ie, surface, partial-thickness, or full-thickness irregularity with or without underlying subchondral bony change) is generally sufficient and prevents confusion that occurs with numeric grading systems. In patients with osteoarthritis not related to prior trauma, diffuse cartilaginous thinning is often noted; this affects the medial compartment more so than the lateral or patellofemoral compartments early in the disease. Later, tricompartmental cartilaginous thinning may be appreciated.
Although subchondral sclerosis often has low signal intensity on both T1- and T2-weighted images, a bone-marrow edema pattern (low signal intensity on T1-weighted images, high signal intensity on T2-weighted images) may also be seen. Zanetti et al concluded, on the basis of histologic findings in osteoarthritic knees that were treated with joint replacement, that this pattern usually represents histologically noncharacteristic abnormalities such as bone marrow fibrosis, bone marrow necrosis, and trabecular abnormalities, whereas actual edema is only a minor constituent. [30]
In addition to intermediate- or T2-weighted fast-spin-echo and 3-dimensional spoiled gradient echo sequences, a variety of additional MRI pulse sequences have been described for morphologic cartilage assessment, including 3-dimensional double-echo steady-state (DESS), driven equilibrium Fourier transform (DEFT), steady-state free precession (SSFP), and 3 dimensional fast-spin-echo sequences. [31]
Further development in the field of quantitative MRI has allowed the ability to probe biochemical changes associated with cartilage degeneration of early osteoarthritis prior to detection of gross morphologic abnormalities. Quantitative assessment of glycosaminoglycan content can be accomplished with MRI techniques such as delayed gadolinium-enhanced MRI of cartilage (dGEMRIC), sodium MRI, and T1rho measurement. Quantitative T2 relaxometry can measure cartilage water content and therefore also has the potential to detect degeneration at an earlier phase than can routine morphologic imaging sequences. [27]
Nuclear Imaging
Scintigraphic studies are of limited use for the diagnosis of osteoarthritis because increased uptake of the radiotracer can also be seen in several other hypervascular articular diseases. The image resolution of bone scintigraphy is much less than that of other imaging modalities. In joints affected with osteoarthritis, increased uptake of bone-seeking radiopharmaceuticals may be seen before any radiographic abnormalities are apparent. Tracer accumulation is concentrated in regions of bony eburnation and osteophyte formation (see the images below).
 Spot delayed technetium-99m methylene diphosphonate (MDP) bone scintigram reveals focal increased radiotracer accumulation at the basilar joints and several interphalangeal joints (circles); this finding is compatible with osteoarthritis.
Spot delayed technetium-99m methylene diphosphonate (MDP) bone scintigram reveals focal increased radiotracer accumulation at the basilar joints and several interphalangeal joints (circles); this finding is compatible with osteoarthritis.
 Radiograph obtained in the same patient as in the previous image shows only tiny osteophytes at the basilar and scaphotrapezium joints.
Radiograph obtained in the same patient as in the previous image shows only tiny osteophytes at the basilar and scaphotrapezium joints.
 Spot delayed technetium-99m methylene diphosphonate (MDP) bone scintigram reveals increased uptake of the radiopharmaceutical in the right hip joint.
Spot delayed technetium-99m methylene diphosphonate (MDP) bone scintigram reveals increased uptake of the radiopharmaceutical in the right hip joint.
-
Standing anteroposterior (AP) radiograph of the knees reveals bilateral medial femorotibial compartment narrowing and sharpening of the tibial spines; this finding is typical of osteoarthritis.
-
Anteroposterior (AP) radiograph of the hip reveals severe superior migration of the femoral head (which reflects loss of articular cartilage), subchondral sclerosis, prominent osteophytes, and a large Egger cyst in the superior acetabulum. Mild flattening of the superior aspect of the femoral head is present.
-
Posteroanterior (PA) radiograph of the hand reveals narrowing, osteophytes, and subchondral cysts affecting the distal interphalangeal joints; this finding is typical of osteoarthritis.
-
Radiograph of the foot reveals narrowing, subchondral sclerosis, and osteophyte formation affecting the first metatarsophalangeal joint. A mild valgus deformity is present as well.
-
Oblique projection demonstrates gradual narrowing and sclerosis of the facet joints as one progresses down the lumbar spine.
-
Standing radiograph of the knee reveals narrowing of the medial and lateral femorotibial compartments with marginal osteophytes.
-
Lateral radiograph of the knee reveals patellofemoral compartment narrowing and osteophytosis. A prominent Parson bump is also seen. Large ossified intra-articular bodies are evident.
-
Radiograph demonstrates narrowing and osteophytosis affecting the first carpometacarpal joint.
-
Close-up radiograph of the wrist shows osteoarthritic changes at the first carpometacarpal joint, with severe narrowing and sclerosis of the trapezium-scaphoid and trapezoid-scaphoid (triscaphe) articulations.
-
Transverse CT scan image obtained through the lower lumbar spine shows sclerosis of the facet joints.
-
Transverse CT scan image obtained through the superior aspect of the hip reveals joint narrowing, osteophyte formation, and subchondral cysts typical of osteoarthritis.
-
T1-weighted coronal MRI of the knee shows typical findings of osteoarthritis, including narrowing and subchondral changes at the medial femorotibial compartment and osteophyte formation.
-
Sagittal 3-dimensional gradient-echo fat-saturated MRI of the knee reveals normal hyperintense articular cartilage.
-
Sagittal 3-dimensional gradient-echo fat-saturated MRI of the knee reveals a full-thickness fissure of the articular cartilage of the patella.
-
Sagittal 3-dimensional gradient-echo fat-saturated MRI of the knee reveals full-thickness thinning of the articular cartilage of the lateral femoral condyle posteriorly with underlying degenerative subchondral marrow changes.
-
Transverse fast spin-echo T2-weighted fat-saturated MR image depicts normal intermediate signal intensity patellar cartilage well outlined against joint effusion.
-
Transverse fast spin-echo T2-weighted fat-saturated MR image of the knee reveals increased signal intensity within the articular cartilage of the patella reflecting degeneration.
-
Transverse fat-suppressed fast spin-echo T2-weighted MR image reveals a fissure of the patellar cartilage filling with joint fluid.
-
Transverse fat-suppressed fast spin-echo T2-weighted MR image reveals a full-thickness defect of the articular cartilage along the medial facet of the patella with underlying degenerative subchondral marrow changes.
-
Spot delayed technetium-99m methylene diphosphonate (MDP) bone scintigram reveals focal increased radiotracer accumulation at the basilar joints and several interphalangeal joints (circles); this finding is compatible with osteoarthritis.
-
Radiograph obtained in the same patient as in the previous image shows only tiny osteophytes at the basilar and scaphotrapezium joints.
-
Spot delayed technetium-99m methylene diphosphonate (MDP) bone scintigram reveals increased uptake of the radiopharmaceutical in the right hip joint.
-
Radiograph obtained in the same patient as in the previous image shows severe osteoarthritic disease (joint narrowing, subchondral sclerosis, osteophytosis) that affects the right hip.
-
Close-up posteroanterior (PA) radiograph of the hand reveals narrowing and osteophytes affecting multiple interphalangeal joints. Note the "gull-wing" configuration of the distal interphalangeal joint of the middle finger due to central erosion. There is also ankylosis of the distal interphalangeal joint of the index finger.
-
Close-up radiograph of the fifth digit shows osteophytes and central erosions resulting in a "gull wing" appearance.
-
Close-up radiograph shows fusion of the distal interphalangeal (DIP) joint of the fifth finger; this finding is compatible with advanced erosive osteoarthritis.











