Practice Essentials
Oncocytoma is the most common benign solid renal tumor and accounts for 3-7% of all primary renal neoplasms. [1, 2, 3, 4, 5] Oncocytoma affects mainly older patients, often in the seventh decade of life. Oncocytomas most often are discovered incidentally by imaging during a workup for other conditions. About one third of patients have signs and/or symptoms, with flank/abdominal pain, hematuria, and/or a flank mass among the most common. Rare familial cases have been described, and many patients have Birt-Hogg-Dubé syndrome. [6, 7]
As a result of variations in its classic appearance, difficulty in standardizing diagnostic criteria, and entities that mimic oncocytoma, such as eosinophilic variant chromophobe renal cell carcinoma (RCC) and succinate dehydrogenase–deficient RCC, pathologic diagnosis remains a challenge. [5] The differential diagnosis of oncocytoma includes other neoplasms with eosinophilic or oncocytic cytoplasm and primarily chromophobe RCC, as well as clear cell RCC with eosinophilic cytoplasm—an oncocytic variant of papillary RCC. Infrequently, oncocytoid RCC occurring after neuroblastoma and epithelioid angiomyolipoma should be included in the differential diagnosis. [2, 8, 9, 10, 11, 12, 13, 14]
Renal oncocytomas are slow-growing tumors that tend to be small, unilateral, and asymptomatic. Large oncocytomas are rare and can be difficult to distinguish from RCCs on the basis of clinical findings or imaging characteristics alone. Papillary adenomas are also benign renal neoplasms, but they arise from the renal tubular epithelium and almost always are located within the cortex. [15]
Because onocytoma is a benign disease, differentiating it from RCC is important, in that it can often be treated conservatively. [10, 13, 14] The central stellate scar can help differentiate renal oncocytoma, but this scar may also be seen in cases of RCC, thereby limiting its accuracy as a differentiating feature. [4]
Oncocytosis is a rare condition characterized by multiple oncocytic tumors with histologic features, including renal oncocytoma, hybrid oncocytic tumor, and, occasionally, chromophobe RCC. Oncocytic nodules may be present in 1 or both kidneys, usually with a single dominant nodule. [4, 7, 16]
Imaging modalities
The morbidity rate of kidney cancer has been increasing. Patient treatment and prognosis depend on the specific histologic type of tumor. Unfortunately, different renal tumors can have similar histologic features, making differential diagnostics challenging. With more than 95% confidence, the nested pattern, myxoid stroma, granular cytoplasm, and round nuclei are likely indicative of renal oncocytoma, whereas varying nuclear size, raisinoid nuclei, and reticular cytoplasm indicate a higher likelihood of chromophobe RCC. These features should be analyzed for confirmation. [17]
Computed tomography (CT) scanning of the abdomen, combined with intravenous administration of iodinated contrast medium, is the examination of choice and the best modality for evaluating a solid renal mass. This technique assists in detection and localization of the tumor, and CT scanning may help in characterizing the mass, especially if fat-containing lesions (eg, angiomyolipomas) are present. Additionally, staging of the tumor can be performed to classify the extent of the lesion, regional lymphadenopathy, vascular involvement, and metastases. CT scanning also helps in detection of calcifications and in differentiation of a complex cyst from a solid neoplasm. [2, 8, 9, 11, 12, 13, 18, 19, 20]
Imaging characteristics of oncocytoma and RCC overlap, and differentiating an oncocytoma from an RCC and other solid renal neoplasms is not always possible with ultrasonography, CT scanning, or magnetic resonance imaging (MRI). The presence of a central scar on CT scanning or on MRI and a spoke-wheel pattern of vessels on angiography are often suggestive of oncocytoma but are not entirely specific. [2, 9, 11, 12, 13, 18]
Because of overlap in imaging features and histologic appearances between oncocytoma and RCC, accurate differentiation on preoperative imaging or percutaneous biopsy remains difficult. Diagnosis is often retrospectively established via gross pathology and microscopy with special stains. [2, 9, 11, 12, 13, 18]
(See the images below.)
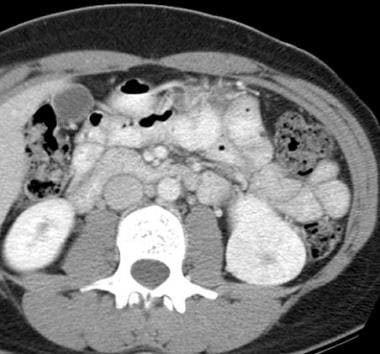 Contrast-enhanced computed tomography (CT) scan of the abdomen obtained during the nephrographic phase. This CT scan shows a well-defined, enhancing mass lesion in the lower pole of the left kidney. A central hypoattenuating stellate scar is seen.
Contrast-enhanced computed tomography (CT) scan of the abdomen obtained during the nephrographic phase. This CT scan shows a well-defined, enhancing mass lesion in the lower pole of the left kidney. A central hypoattenuating stellate scar is seen.
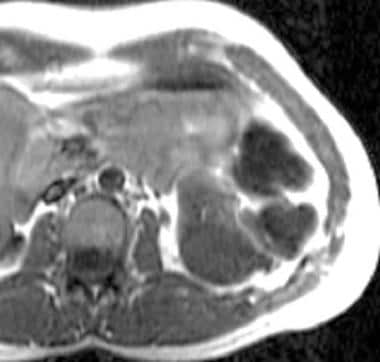 T1-weighted magnetic resonance image (MRI). This MRI shows a homogeneous, hypointense, well-defined mass in the lower pole of the kidney.
T1-weighted magnetic resonance image (MRI). This MRI shows a homogeneous, hypointense, well-defined mass in the lower pole of the kidney.
Radiography
The degree of confidence is low for detecting oncocytomas with radiographs. Plain radiographic findings are nonspecific, and images may show a large, soft tissue mass in the renal area with displacement of fat planes. Calcification is rare.
Excretory urography shows a large mass with a renal contour abnormality and compression of the collecting system. False-positive results may be found with any lesion that causes a renal contour abnormality. Examples include a renal cyst, any renal mass, and focal infection. In addition, any retroperitoneal tumor may have a similar appearance.
False-negative findings are due to the small size of the tumor and the presence of overlapping bowel.
Computed Tomography
On nonenhanced CT scans, oncocytomas appear isoattenuating or slightly hyperattenuating relative to the kidney parenchyma. [18] On contrast-enhanced CT scans obtained during the nephrographic phase, the mass appears less attenuating than the renal parenchyma. [2, 9, 11, 12, 13, 19, 20, 21]
(See the images below.)
 Contrast-enhanced computed tomography (CT) scan of the abdomen obtained during the nephrographic phase. This CT scan shows a well-defined, enhancing mass lesion in the lower pole of the left kidney. A central hypoattenuating stellate scar is seen.
Contrast-enhanced computed tomography (CT) scan of the abdomen obtained during the nephrographic phase. This CT scan shows a well-defined, enhancing mass lesion in the lower pole of the left kidney. A central hypoattenuating stellate scar is seen.
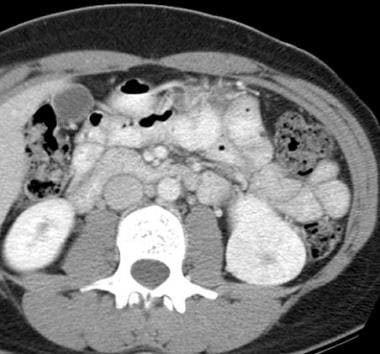
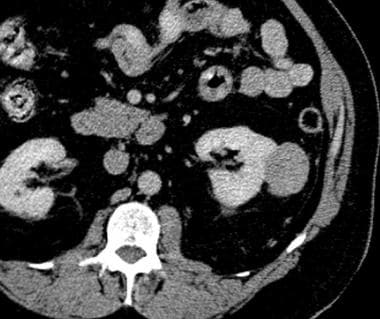 Contrast-enhanced computed tomography (CT) scan of the abdomen obtained during the nephrographic phase. This CT scan shows a well-defined, exophytic, solid mass from the midpole of the left kidney. The mass has an atypical appearance of an oncocytoma, is less attenuating than the renal parenchyma, and does not show a scar.
Contrast-enhanced computed tomography (CT) scan of the abdomen obtained during the nephrographic phase. This CT scan shows a well-defined, exophytic, solid mass from the midpole of the left kidney. The mass has an atypical appearance of an oncocytoma, is less attenuating than the renal parenchyma, and does not show a scar.
Oncocytomas are well encapsulated and have distinct margins, a smooth contour, and a homogeneous appearance. Tumors may range in size from 3 to 10 cm, and in symptomatic patients, lesions most often are larger than 5 cm.
A central hypoattenuating scar may be observed in 33% of cases, but this scar cannot be differentiated from the central necrosis commonly found in RCC. With the advent of multisection CT scanning, high-resolution thin sections through the kidneys may improve detection of the central scar.
Researchers have discussed the use of segmental enhancement inversion (SEI) to help identify small renal oncocytoma. SEI is evident when the renal oncocytoma is divided into 2 differently enhanced segments on corticomedullary phase images (30-40 seconds after contrast injection) that demonstrate reversal of the relative degree of enhancement on nephrographic phase images (120-180 seconds after contrast injection). Some studies have found that SEI is often noted with oncocytomas smaller than 3 cm, and central scars are seen more often with oncocytomas larger than 2.5 cm. [9, 22]
Calcification, necrosis, and hemorrhage are rare with oncocytoma. Typically, features of a malignant tumor—such as invasion or infiltration into perinephric fat, collecting system, or vessels—are absent. Likewise, regional lymphadenopathy and metastases are not encountered in patients with oncocytoma. Occasionally, multifocal or bilateral tumors may be found.
The degree of confidence for detecting this tumor on CT scanning is high. However, the degree of confidence in differentiating an oncocytoma from an RCC is low. Differentiating an oncocytoma from an RCC and from other solid renal tumors is not always possible. The presence of a central scar may help, but necrosis in RCC may mimic this finding. [9, 11, 12, 18]
In a retrospective study, Li and associates explored the utility of CT in differentiating renal oncocytoma and chromophobe RCC. In this study, the logistic regression model showed that location (right kidney), hypodensity on nonenhanced CT, SEI, and perirenal fascial thickening were highly predictive of renal oncocytoma. Combined indicators from the logistic regression model were used for receiver operating characteristic (ROC) analysis. The area under the ROC curve was 0.923 (P < 0.001). Sensitivity and specificity of the 4 factors combined for diagnosing renal oncocytoma were 88% and 86.3%, respectively. The correlation coefficient between necrosis and tumor size for all tumors, including both renal oncocytoma and chromophobe RCC, was 0.584, indicating a positive correlation (P < 0.001). Investigators concluded that CT imaging features of location (right kidney), hypodensity on nonenhanced CT, SEI, and perirenal fascia thickening were valuable indicators in distinguishing renal oncocytoma from chromophobe RCC. [23]
Baghdadi and colleagues evaluated the feasibility of an objective method using artificial intelligence (AI) and image processing in a semiautomated fashion for tumor-to-cortex peak early-phase enhancement ratio (PEER) to differentiate CD117(+) oncocytoma from the chromophobe subtype of RCC using convolutional neural networks (CNNs) on CT imaging. The mean ± SD Dice similarity score for segmentation was 0.66 ± 0.14 for the CNN model to identify kidney + tumor areas. Results show that PEER evaluation achieved accuracy of 95% in tumor type classification (100% sensitivity and 89% specificity) compared with final pathology results (root-meaning-square error [RMSE] of 0.15 for PEER ratio). Researchers concluded that deep learning could help to produce reliable discrimination of CD117(+) benign oncocytoma and malignant chromophobe RCC through PEER measurements obtained by computer vision. [24]
Magnetic Resonance Imaging
On nonenhanced T1-weighted MRI, oncocytomas are well-defined, homogeneous masses. They may appear isointense to hypointense relative to the renal cortex. On T2-weighted images, tumors are typically isointense to slightly hypointense; however, slight T2 hyperintensity has also been reported. [25]
(For MRIs of oncocytoma, see the images below.)
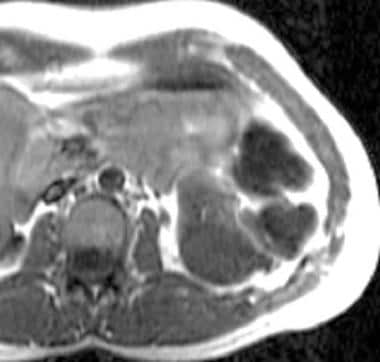 T1-weighted magnetic resonance image (MRI). This MRI shows a homogeneous, hypointense, well-defined mass in the lower pole of the kidney.
T1-weighted magnetic resonance image (MRI). This MRI shows a homogeneous, hypointense, well-defined mass in the lower pole of the kidney.
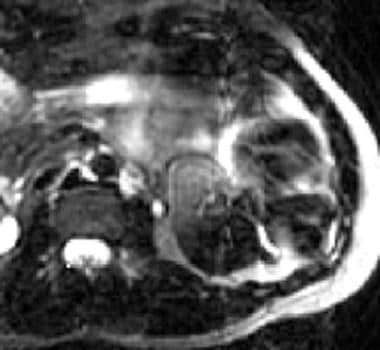 T2-weighted magnetic resonance image (MRI) of the kidney. This MRI shows that the lesion is hypointense and has a mildly hyperintense central scar (same patient as in previous image).
T2-weighted magnetic resonance image (MRI) of the kidney. This MRI shows that the lesion is hypointense and has a mildly hyperintense central scar (same patient as in previous image).
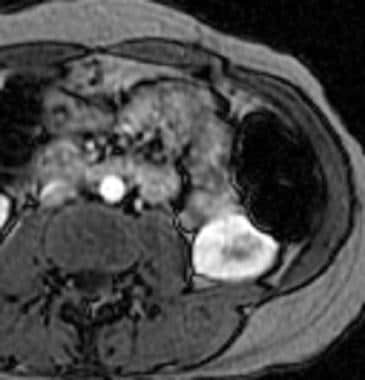 Contrast-enhanced T1-weighted magnetic resonance image (MRI). This MRI of the kidney shows homogeneous enhancement of the mass with a nonenhancing central scar. Note the lack of any tumoral invasion into the perinephric fat (same patient as in previous 2 images).
Contrast-enhanced T1-weighted magnetic resonance image (MRI). This MRI of the kidney shows homogeneous enhancement of the mass with a nonenhancing central scar. Note the lack of any tumoral invasion into the perinephric fat (same patient as in previous 2 images).
When present, the tumor scar may be seen as a hypointense, stellate area in the center of the lesion on T1- and T2-weighted MRI. However, tumor necrosis, a common feature of malignant masses, appears hypointense on T1-weighted images and hyperintense on T2-weighted images. Rarely, the central scar may appear bright on T2-weighted images.
After intravenous administration of gadopentetate dimeglumine contrast material, oncocytomas show homogeneous enhancement with a nonenhancing central scar.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). This disease has occurred in patients with moderate to end-stage renal disease after they were given a gadolinium-based contrast agent to enhance magnetic resonance imaging (MRI) or magnetic resonance angiography (MRA) scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
The degree of confidence with MRI for detecting this lesion is high, but the degree of confidence with this technique for making a specific diagnosis is low. Differentiating an oncocytoma from an RCC and from other solid renal tumors is not always possible.
Precise diagnosis and subtyping of kidney tumors are imperative for optimizing and personalizing treatment decisions for patients. Patients with the most common benign renal tumor—renal oncocytoma—may be overtreated with surgical resection because of limited preoperative diagnostic methods that can accurately identify the benign condition with certainty. In one study, desorption electrospray ionization (DESI)-mass spectrometry (MS) imaging was applied to study the metabolic and lipid profiles of various types of renal tissues, including normal kidney, renal oncocytoma, and RCC. Researchers found that metabolic data acquired by DESI-MS imaging in conjunction with statistical modeling allowed discrimination of renal tumors and may be used in the clinical setting to improve treatment of patients with kidney tumor. [26]
Ultrasonography
Renal oncocytomas are easily misdiagnosed as renal cancers, resulting in unnecessary radical nephrectomy. This review summarizes the use of ultrasound for diagnosis of renal oncocytoma. On 2-dimensional grayscale ultrasound, renal oncocytoma appears as a solid, well-defined, round or oval, and relatively isoechoic or slightly hyperechoic mass. On color Doppler flow imaging, the spoke-wheel sign is evident. On power Doppler flow imaging, renal oncocytomas show mixed penetrating and peripheral patterns. Renal oncocytomas usually appear as highly enhanced on contrast-enhanced ultrasound images, and as irregular nonenhanced areas within larger tumors. [27]
Ultrasonography has low sensitivity and specificity for detection and characterization of solid renal masses. However, this modality is useful for differentiating a solid mass from a complex cystic mass. On ultrasonography images, oncocytomas appear as well-defined, homogeneous, and hypoechoic to isoechoic masses. The central scar cannot be confidently identified on sonograms; however, when the scar is seen, especially with large lesions, it may appear echogenic. Color Doppler ultrasonography may show central radiating vessels. [28, 29] Small isoechoic lesions may be missed on sonograms. Larger lesions cannot be differentiated from other renal masses. However, RCCs often reveal more heterogeneous echogenicity and irregularly shaped and poorly demarcated margins with adjacent tissue. [8]
Nuclear Imaging
Scintigraphy is not routinely performed in evaluation of renal tumors. On technetium-99m (99mTc) dimercaptosuccinic acid (DMSA) scans, the oncocytoma appears as a photopenic area that displaces the renal cortex and collecting system.
On fluorodeoxyglucose (FDG) positron emission tomography (PET) scanning, oncocytomas usually show less FDG uptake than RCCs. Uptake is usually isointense relative to the renal parenchyma. However, oncocytomas occasionally have uptake in the range similar to that of RCC uptake.
The degree of confidence with nuclear medicine is low. False-positive results are due to renal cysts or other photopenic renal masses. False-negative results occur if the mass is small, or when the lesion does not cause a renal contour abnormality.
Angiography
With the advent of CT scanning, routine angiography is not performed to diagnose renal masses. However, classic angiographic findings for oncocytoma include a spoke-wheel arrangement of tumoral vessels, homogeneous tumoral contrast during the capillary phase, sharp demarcation from kidney and surrounding areas, and a peritumoral halo (lucent rim sign). Bizarre neoplastic vessels are conspicuously absent, in contrast to RCC.
The degree of confidence with angiography is low. Hypovascular lesions may result in false-negative results, and hypervascular lesions may mimic RCCs.
Current and Future Evaluation and Treatment Approaches
Evaluation of renal oncocytomas is usually first done via imaging. Oncocytomas may be discovered incidentally. There are no precise radiologic criteria for distinguishing a benign oncocytoma from a malignant lesion such as renal cell carcinoma. However, central scar and hypervascularity can often be appreciated on imaging. A kidney mass can be evaluated with core biopsy, fine-needle aspiration, or resection. Oncocytomas are often small, and because 20-45% of small renal masses are ultimately found to be benign, active surveillance is an option often offered to patients. [30]
In a review on the topic of renal oncocytoma, Trevisani and colleagues stated that the real challenge in the oncocytoma treatment algorithm is related to misdiagnosis due to its resemblance, at initial radiologic assessment, to malignant renal cancer, with a completely different prognosis and differences in the use of medical treatment. Unfortunately, percutaneous renal biopsy is not frequently performed because of possible side effects related to the procedure. Therefore, most cases of oncocytoma are diagnosed after the surgical operation via partial or radical nephrectomy. For this reason, new reliable strategies to address this issue are needed. [31]
-
Contrast-enhanced computed tomography (CT) scan of the abdomen obtained during the nephrographic phase. This CT scan shows a well-defined, enhancing mass lesion in the lower pole of the left kidney. A central hypoattenuating stellate scar is seen.
-
Contrast-enhanced computed tomography (CT) scan of the abdomen obtained during the nephrographic phase. This CT scan shows a well-defined, exophytic, solid mass from the midpole of the left kidney. The mass has an atypical appearance of an oncocytoma, is less attenuating than the renal parenchyma, and does not show a scar.
-
T1-weighted magnetic resonance image (MRI). This MRI shows a homogeneous, hypointense, well-defined mass in the lower pole of the kidney.
-
T2-weighted magnetic resonance image (MRI) of the kidney. This MRI shows that the lesion is hypointense and has a mildly hyperintense central scar (same patient as in previous image).
-
Contrast-enhanced T1-weighted magnetic resonance image (MRI). This MRI of the kidney shows homogeneous enhancement of the mass with a nonenhancing central scar. Note the lack of any tumoral invasion into the perinephric fat (same patient as in previous 2 images).




