Practice Essentials
Arachnoid cysts are benign cysts that occur in the cerebrospinal axis in relation to the arachnoid membrane and that do not communicate with the ventricular system. They usually contain clear, colorless fluid that is most likely normal cerebrospinal fluid; rarely, they contain xanthochromic fluid. Most are developmental anomalies. A small number of arachnoid cysts are acquired, such as those occurring in association with neoplasms or those resulting from adhesions occurring in association with leptomeningitis, hemorrhage, or surgery. They constitute approximately 1% of intracranial masses; 50-60% occur in the middle cranial fossa. Cysts in the middle cranial fossa are found more frequently in males than in females; they occur predominantly on the left side. Most arise as developmental anomalies. A small number of arachnoid cysts are associated with neoplasms. CT imaging is often sufficient to make the diagnosis, but when additional information is needed, MRI is the imaging modality of choice to evaluate anatomic location, size, and structures involved. MRI can also help refine the differential diagnosis. [1, 2]
The radiologist needs to evaluate the brain structures for mass effect secondary to the arachnoid cyst, such as a subtle mass effect on a cranial nerve or a prominent mass effect resulting in brain herniation. Immediate intervention is necessary if the cyst is in a critical location causing hydrocephalus or if a large cyst is resulting in mass effect and brain herniation. [1]
Spinal meningeal cysts were classified by Nabors et al as follows [3] :
-
Type I: Spinal extradural without spinal nerve root fibers (type Ia: extradural spinal arachnoid cyst; type Ib: sacral meningocele).
-
Type II: Spinal extradural with spinal nerve root fibers.
-
Type III: Spinal intradural.
(See the images below.)
 T2-weighted sagittal MRI image (see next image for axial view) of the brain in a 28-year-old woman with an incidental finding of a superior cerebellar cistern arachnoid cyst (arrow).
T2-weighted sagittal MRI image (see next image for axial view) of the brain in a 28-year-old woman with an incidental finding of a superior cerebellar cistern arachnoid cyst (arrow).
 T2-weighted axial MRI image (see previous image for sagittal view) of the brain in a 28-year-old woman with an incidental finding of a superior cerebellar cistern arachnoid cyst (arrow).
T2-weighted axial MRI image (see previous image for sagittal view) of the brain in a 28-year-old woman with an incidental finding of a superior cerebellar cistern arachnoid cyst (arrow).
Arachnoid cysts also occur within the spinal canal; in such cases, arachnoid cysts or arachnoid diverticula may be located subdurally or in the epidural space, respectively. Spinal arachnoid cysts are commonly located dorsal to the cord in the thoracic region. A cyst in this location is usually secondary to a congenital or acquired defect and is situated in an extradural location. Intradural spinal arachnoid cysts are secondary to a congenital deficiency within the arachnoidal trabecula, especially in the septum posticum, or are the result of adhesions resulting from previous infection or trauma. Microscopic examination shows that their walls are formed from a splitting of the arachnoid membrane, with an inner and outer leaflet surrounding the cyst cavity. [4]
Spinal arachnoid cysts are generally misdiagnosed, because symptoms are often nonspecific. Often, the cysts are an incidental finding on magnetic resonance imaging (MRI). Usually, arachnoid cysts are asymptomatic; this is true even of cysts that are quite large. The most commonly associated clinical features are headache, calvarial bulging, and seizures; focal neurologic signs occur less frequently. Controversy surrounds the treatment of arachnoid cysts.
Some clinicians advocate treating only patients with symptomatic cysts, whereas others believe that even asymptomatic cysts should be decompressed to avoid future complications. The most effective surgical treatment appears to be excision of the outer cyst membrane and cystoperitoneal shunting. [5, 6, 7, 8] Cysts that cause symptoms from cord compression are best evaluated with MRI; they should be surgically excised, if possible.
A genetic link to arachnoid cysts has been described. Chudley-McCullough syndrome is an autosomal recessive disorder associated with severe-to-profound sensorineural hearing loss and partial agenesis of the corpus callosum. Other brain anomalies reported with the syndrome include frontal polymicrogyria and gray matter heterotopia, cerebellar dysplasia, ventriculomegaly, and arachnoid cysts. Despite these significant brain anomalies, these patients do not present with neurodevelopmental abnormalities, except for hearing loss.
DNA from affected families has revealed 4 molecular variations in the G protein–signaling modulator 2 gene, GPSM2. Subsequent brain imaging of these individuals revealed frontal polymicrogyria, abnormal corpus callosum, and gray matter heterotopia, consistent with a Chudley-McCullough syndrome diagnosis, but no ventriculomegaly. The gene product, GPSM2 is required for orienting the mitotic spindle during cell division in multiple tissues, suggesting that the brain malformations are due to defects in asymmetric cell divisions during development. [9]
Prenatal Diagnosis
Arachnoid cysts can be seen on prenatal ultrasound anatomic scans, although the finding is rare; in one study of 33,621 scans, arachnoid cysts were identified in 70 patients (0.2%). [10] The majority of children with a prenatal diagnosis had normal neurodevelopmental outcomes. [11, 12] Reported predictors of abnormal outcomes include large size (>2 cm), syndromic/genetic diagnosis, and/or the presence of other intracranial abnormalities. [10, 12]
Imaging modalities
MRI is the diagnostic procedure of choice because of its ability to demonstrate the exact location, extent, and relationship of the arachnoid cyst to adjacent brain or spinal cord. Myelography and computed tomography (CT) myelography remain of diagnostic value, especially for cases that are not definitive on MRI. Plain radiographic findings are nonspecific and have little to offer in the diagnosis of arachnoid cysts, although changes in skull contour may be detected on skull radiographs performed for other indications, such as trauma. [13, 14]
Cranial ultrasonography is an important diagnostic tool during the first year of life. Although symptomatic arachnoid cysts are comparatively rare in infants, ultrasound is useful as a noninvasive imaging technique with high yield in the detection and characterization of cystic masses. Although angiography may show associated anomalies of venous drainage and the relationship of the lesion to normal vasculature, which may be useful for surgical planning, in practice, angiography is rarely performed, because CT angiography or magnetic resonance angiography provides the same information noninvasively.
Every effort must be made to reliably detect arachnoid cysts, because most arachnoid cysts are an incidental finding and most patients are asymptomatic. Arachnoid cysts must be differentiated from the more serious cystic intracranial and intraspinal tumors. In cases involving larger arachnoid cysts, consideration should be given to the use of serial scans, because such cysts may enlarge over time; patients with such cysts may become candidates for surgery.
Skull radiographic findings cannot be relied upon because the signs are nonspecific. Arachnoid cysts may be confused with several intracranial cysts of various etiologies. The confusion is much more likely to occur with CT. CT attenuation values and signal intensities of arachnoid cysts parallel those of CSF, and difficulties may be encountered in cases of hemorrhagic cysts.
The most important differentiation to make is between arachnoid cysts and epidermoid cysts; MRI diffusion-weighted images (DWIs) make differentiating the 2 masses easier. Some arachnoid cysts contain proteinaceous fluid or blood; in such cases, signal loss on DWIs may not be marked, which may pose diagnostic problems. Also, tissue contrast with fluid-attenuated inversion recovery (FLAIR) imaging is similar to that with a T2-weighted image, but FLAIR shows no signal arising from the CSF. Thus, unlike with epidermoid cysts, arachnoid cysts containing CSF demonstrate a suppressed (low) signal on FLAIR.
In a study by Algin et al, the sensitivity and specificity of phase-contrast cine magnetic resonance imaging (PC-MRI) in identifying communications between IV-ACs and the CSF were found to be 100% and 54%, respectively. The investigators measured the sensitivity and specificity of intraventricular arachnoid cysts (IV-ACs) and their communication with CSF spaces using PC-MRI and compared the PC-MRI findings with those on MR cisternography (MRC) in 21 patients. In 7 IV-ACs, there was no communication detected on PC-MRI, and in 14 cases, a pulsatile CSF flow was seen into the IV-ACs. All the IV-ACs that were determined as noncommunicating on PC-MRI were corroborated on MRC. Six cases in which a communication was shown on PC-MRI were not corroborated on MRC. MRC revealed a total of 8 communicating and 13 noncommunicating IV-ACs in the 21 patients. [5]
MRI cisternography can be performed with or without contrast. Intrathecal contrast-enhanced MRI cisternography may demonstrate the connection between the arachnoid cyst and the surrounding CSF space. The MRI noncontrast techniques (constructive interference in steady-state [CISS], fast imaging employing steady-state acquisition [FIESTA], and 3D T2-weighted sampling perfection with application-optimized contrast with different flip-angle evolutions [3D SPACE]) show the arachnoid cyst wall and surrounding structures, such as cranial nerves and vessels. [1, 15, 16, 2]
Radiography
Plain radiographs have low sensitivity in the diagnosis of arachnoid cysts and contribute little to the diagnosis.
Forward bowing of the anterior cranial wall of the middle cranial fossa and elevation of the sphenoidal ridge have been reported findings on skull radiographs of patients with arachnoid cysts of the middle cranial fossa. However, such findings are difficult to assess; occasionally, patients with these features may be difficult to differentiate from normal patients. In addition, changes seen in other conditions, such as neurofibromatosis type I, may mimic these changes.
In infants, craniomegaly associated with widening of the fontanelle and thinning of the calvarium may be observed. However, these characteristics may be a normal variant and may be associated with other intracranial pathology.
The spinal canal may be widened, and erosion of the pedicles may occur. However, the differential diagnosis is wide and includes spinal cord tumors.
Computed Tomography
There is a wide differential diagnosis for both intracranial and intraspinal cystic lesions, and arachnoid cysts have several mimics. In particular, with hemorrhagic arachnoid cysts, difficulties are encountered when the cyst contents are no longer isodense to CSF.
Intracranial arachnoid cysts may be an incidental finding on CT scans. Typically, in cases of arachnoid cysts, the subarachnoid space is compressed by a cystic structure that may be unilocular or septate. The size of such structures varies. The septa may not always be visible (see the images below). The subjacent brain shows minimal mass effect.
 Unenhanced CT scan of the head in a 26-year-old man with a history of seizures since childhood (same patient as in the next image). The scan shows a large left frontoparietal cyst with a mass effect. The cyst was resected, and histologic analysis confirmed an arachnoid cyst.
Unenhanced CT scan of the head in a 26-year-old man with a history of seizures since childhood (same patient as in the next image). The scan shows a large left frontoparietal cyst with a mass effect. The cyst was resected, and histologic analysis confirmed an arachnoid cyst.
 Unenhanced CT scan of the head in a 26-year-old man with a history of seizures since childhood (same patient as in the previous image). The scan shows a large left frontoparietal cyst with a mass effect. The cyst was resected, and histologic analysis confirmed an arachnoid cyst.
Unenhanced CT scan of the head in a 26-year-old man with a history of seizures since childhood (same patient as in the previous image). The scan shows a large left frontoparietal cyst with a mass effect. The cyst was resected, and histologic analysis confirmed an arachnoid cyst.
On CT scans, arachnoid cysts are characterized by sharp, nonenhancing borders; they are isodense to CSF. On a bone window, remodeling of the skull may be evident. Arachnoid cysts seldom calcify. On CT cisternography, arachnoid cysts may be seen to have a smooth outer surface, in contradistinction to epidermoid cysts, which typically have an irregular outer surface that is likened to the surface of cauliflower. With respect to cyst filling, CT cisternography yields mixed results. Some cysts fill with contrast immediately; with others, either filling is delayed or no filling occurs.
On CT cisternography, nonionic iodinated contrast is injected intrathecally, and the amount of filling and the time it takes to fill the cyst can help guide management. If cysts fill completely and early, they are considered freely communicating, and treatment may not be necessary. [1, 15, 2]
Noncommunicating and slow-filling cysts are regarded as true arachnoid cysts, whereas communicating cysts are regarded as diverticula of the subarachnoid space. It has been proposed that noncommunicating cysts expand either as the result of a ball-valve mechanism or because of fluid secretion by the cyst wall, perhaps along an osmotic gradient.
On CT scanning, spinal arachnoid cysts may not be sufficiently characterized to preclude the need for further imaging. CT scanning of the spine is useful in establishing the differential diagnosis of nondiscogenic radiculopathy; in addition, it demonstrates bone detail well.
Magnetic Resonance Imaging
MRI is the diagnostic procedure of choice in the detection of intracranial and intraspinal arachnoid cysts because of its potential to demonstrate the exact location and extent of the cysts and their relationship to the brain and spinal cord. The most important mimic of an arachnoid cyst is an epidermoid cyst.
Intracranial
On MRI, arachnoid cysts appear as well-defined nonenhancing intracranial masses that are isointense to CSF (see the images below).
 T2-weighted sagittal MRI image (see next image for axial view) of the brain in a 28-year-old woman with an incidental finding of a superior cerebellar cistern arachnoid cyst (arrow).
T2-weighted sagittal MRI image (see next image for axial view) of the brain in a 28-year-old woman with an incidental finding of a superior cerebellar cistern arachnoid cyst (arrow).
 T2-weighted axial MRI image (see previous image for sagittal view) of the brain in a 28-year-old woman with an incidental finding of a superior cerebellar cistern arachnoid cyst (arrow).
T2-weighted axial MRI image (see previous image for sagittal view) of the brain in a 28-year-old woman with an incidental finding of a superior cerebellar cistern arachnoid cyst (arrow).
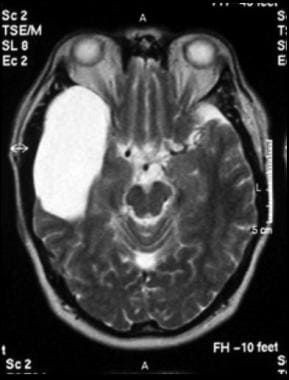 Axial T2-weighted MRI image through the midbrain, showing a right middle cranial fossa homogeneous lesion (same lesion as in the next 3 images) with CSF signal intensity and no perceptible wall or internal complexity. There is associated remodeling of the adjacent sphenoid bone and brain displacement. These imaging features are typical of an arachnoid cyst.
Axial T2-weighted MRI image through the midbrain, showing a right middle cranial fossa homogeneous lesion (same lesion as in the next 3 images) with CSF signal intensity and no perceptible wall or internal complexity. There is associated remodeling of the adjacent sphenoid bone and brain displacement. These imaging features are typical of an arachnoid cyst.
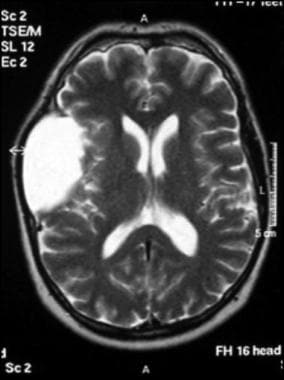 Axial T2-weighted MRI image through the body of the lateral ventricles, showing superior extension of a right middle cranial fossa lesion. The lesion is homogeneous, with no perceptible wall, no internal complexity, and CSF signal intensity. There is associated remodeling of the adjacent calvarium and brain displacement. These imaging features are typical of an arachnoid cyst.
Axial T2-weighted MRI image through the body of the lateral ventricles, showing superior extension of a right middle cranial fossa lesion. The lesion is homogeneous, with no perceptible wall, no internal complexity, and CSF signal intensity. There is associated remodeling of the adjacent calvarium and brain displacement. These imaging features are typical of an arachnoid cyst.
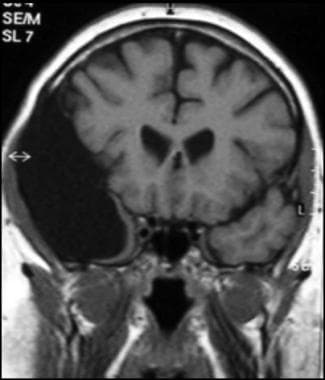 Coronal T1-weighted MRI image through a brain lesion, showing homogeneity of the lesion, lack of a perceptible wall, lack of internal complexity, and CSF signal intensity. There is associated remodeling of the adjacent calvarium and brain displacement. These imaging features are typical of an arachnoid cyst.
Coronal T1-weighted MRI image through a brain lesion, showing homogeneity of the lesion, lack of a perceptible wall, lack of internal complexity, and CSF signal intensity. There is associated remodeling of the adjacent calvarium and brain displacement. These imaging features are typical of an arachnoid cyst.
 Sagittal fluid-attenuated inversion recovery (FLAIR) weighted image through a brain lesion, showing homogeneity of the lesion, lack of a perceptible wall, lack of internal complexity, and CSF signal intensity. There is associated remodeling of the adjacent sphenoid bone and brain displacement. These imaging features are typical of an arachnoid cyst.
Sagittal fluid-attenuated inversion recovery (FLAIR) weighted image through a brain lesion, showing homogeneity of the lesion, lack of a perceptible wall, lack of internal complexity, and CSF signal intensity. There is associated remodeling of the adjacent sphenoid bone and brain displacement. These imaging features are typical of an arachnoid cyst.
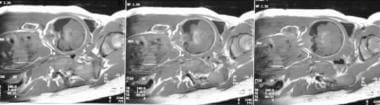 Prenatal coronal T1-weighted MRI images through the middle cranial fossa, showing a left temporal fossa homogeneous lesion (postnatal images of same patient seen in the next 2 images) with CSF signal intensity and no perceptible wall or internal complexity. There is associated displacement of adjacent brain. These imaging features are typical of an arachnoid cyst.
Prenatal coronal T1-weighted MRI images through the middle cranial fossa, showing a left temporal fossa homogeneous lesion (postnatal images of same patient seen in the next 2 images) with CSF signal intensity and no perceptible wall or internal complexity. There is associated displacement of adjacent brain. These imaging features are typical of an arachnoid cyst.
 Postnatal coronal T2-weighted MRI images through the middle cranial fossa, showing a left temporal fossa homogeneous lesion with CSF signal intensity and no perceptible wall or internal complexity. There is associated remodeling of adjacent calvarium, brain displacement, and a midline shift. These imaging features are typical of an arachnoid cyst.
Postnatal coronal T2-weighted MRI images through the middle cranial fossa, showing a left temporal fossa homogeneous lesion with CSF signal intensity and no perceptible wall or internal complexity. There is associated remodeling of adjacent calvarium, brain displacement, and a midline shift. These imaging features are typical of an arachnoid cyst.
 Postnatal coronal T1-weighted MRI images through the middle cranial fossa, showing a left temporal fossa homogeneous lesion with CSF signal intensity and no perceptible wall or internal complexity. There is associated remodeling of adjacent calvarium, brain displacement, and a midline shift. These imaging features are typical of an arachnoid cyst.
Postnatal coronal T1-weighted MRI images through the middle cranial fossa, showing a left temporal fossa homogeneous lesion with CSF signal intensity and no perceptible wall or internal complexity. There is associated remodeling of adjacent calvarium, brain displacement, and a midline shift. These imaging features are typical of an arachnoid cyst.
Diagnostic confusion occasionally arises between arachnoid cysts and epidermoid cysts. The 2 masses may have similar characteristics on T1-weighted and T2-weighted images, and neither shows enhancement with gadolinium. However, arachnoid cysts follow CSF signals on all sequences—in particular, on the FLAIR sequence—in contradistinction to epidermoid cysts. DWIs allow easier differentiation of the 2 masses.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
As a result of the CSF contents of arachnoid cysts, the signal intensity on DWI is low; epidermoid cysts tend to have a high signal on DWI.
Some arachnoid cysts contain proteinaceous fluid or blood. In such cases, signal loss on DWI may not be marked; this may pose diagnostic problems when using DWI.
FLAIR imaging demonstrates tissue contrast similar to that of T2-weighted images, but FLAIR shows no signal arising from the CSF. Therefore, FLAIR demonstrates a suppressed (low) signal in arachnoid cysts that contain CSF; in epidermoid cysts, that signal is typically higher.
A large cisterna magna (mega cisterna magna) occasionally may be confused with an arachnoid cyst. Mega cisterna magna may represent a normal variant (intact cerebellum and vermis), but it may be associated with Dandy-Walker syndrome, either full blown or a variant in which the vermis is either completely or partially absent. Mega cisterna magna and arachnoid cysts show CSF characteristics on T1-weighted, T2-weighted, DWI, and FLAIR sequences. However, whereas an arachnoid cyst may demonstrate mass effect with an en bloc displacement of the cerebellum and vermis, normal-variant mega cisterna magna demonstrates no mass effect, and the cerebellum and vermis remain intact.
Spinal
MRI of spinal arachnoid cysts demonstrates an oval, sharply demarcated extramedullary mass that may cause local displacement and/or spinal cord compression.
The cyst is usually hyperintense to CSF on T2-weighted sequences because of the relative lack of CSF pulsation artifacts. [17, 18, 19, 20]
MRI cisternography can be performed with or without contrast. Intrathecal contrast-enhanced MRI cisternography may demonstrate the connection between the arachnoid cyst and the surrounding CSF space. The MRI noncontrast techniques (constructive interference in steady-state [CISS], fast imaging employing steady-state acquisition [FIESTA], and 3D T2-weighted sampling perfection with application-optimized contrast with different flip-angle evolutions [3D SPACE]) show the arachnoid cyst wall and surrounding structures, such as cranial nerves and vessels. [1, 15, 16, 2]
Ultrasonography
Ultrasonography has a high yield in the detection and characterization of cystic masses. Cranial ultrasonography is an important diagnostic tool during the first year of life. However, it is limited by the closure of the anterior fontanelle, which normally occurs in full-term infants 9-18 months of age.
Intracranial cysts and ventriculomegaly also may be detected and characterized by transcranial ultrasonography through a burr hole. [21]
Angiography
Findings on angiography indicate that there is a higher incidence of an absence of the middle cerebral vein in patients with arachnoid cysts of the middle fossa, as compared with the general population.
Angiographic findings indicate that among patients with arachnoid cysts of the middle fossa, there is a decrease in drainage of the middle cerebral vein into the cavernous sinus on the side of the cyst.
-
T2-weighted sagittal MRI image (see next image for axial view) of the brain in a 28-year-old woman with an incidental finding of a superior cerebellar cistern arachnoid cyst (arrow).
-
T2-weighted axial MRI image (see previous image for sagittal view) of the brain in a 28-year-old woman with an incidental finding of a superior cerebellar cistern arachnoid cyst (arrow).
-
Unenhanced CT scan of the head in a 26-year-old man with a history of seizures since childhood (same patient as in the next image). The scan shows a large left frontoparietal cyst with a mass effect. The cyst was resected, and histologic analysis confirmed an arachnoid cyst.
-
Unenhanced CT scan of the head in a 26-year-old man with a history of seizures since childhood (same patient as in the previous image). The scan shows a large left frontoparietal cyst with a mass effect. The cyst was resected, and histologic analysis confirmed an arachnoid cyst.
-
Axial T2-weighted MRI image through the midbrain, showing a right middle cranial fossa homogeneous lesion (same lesion as in the next 3 images) with CSF signal intensity and no perceptible wall or internal complexity. There is associated remodeling of the adjacent sphenoid bone and brain displacement. These imaging features are typical of an arachnoid cyst.
-
Axial T2-weighted MRI image through the body of the lateral ventricles, showing superior extension of a right middle cranial fossa lesion. The lesion is homogeneous, with no perceptible wall, no internal complexity, and CSF signal intensity. There is associated remodeling of the adjacent calvarium and brain displacement. These imaging features are typical of an arachnoid cyst.
-
Coronal T1-weighted MRI image through a brain lesion, showing homogeneity of the lesion, lack of a perceptible wall, lack of internal complexity, and CSF signal intensity. There is associated remodeling of the adjacent calvarium and brain displacement. These imaging features are typical of an arachnoid cyst.
-
Sagittal fluid-attenuated inversion recovery (FLAIR) weighted image through a brain lesion, showing homogeneity of the lesion, lack of a perceptible wall, lack of internal complexity, and CSF signal intensity. There is associated remodeling of the adjacent sphenoid bone and brain displacement. These imaging features are typical of an arachnoid cyst.
-
Prenatal coronal T1-weighted MRI images through the middle cranial fossa, showing a left temporal fossa homogeneous lesion (postnatal images of same patient seen in the next 2 images) with CSF signal intensity and no perceptible wall or internal complexity. There is associated displacement of adjacent brain. These imaging features are typical of an arachnoid cyst.
-
Postnatal coronal T2-weighted MRI images through the middle cranial fossa, showing a left temporal fossa homogeneous lesion with CSF signal intensity and no perceptible wall or internal complexity. There is associated remodeling of adjacent calvarium, brain displacement, and a midline shift. These imaging features are typical of an arachnoid cyst.
-
Postnatal coronal T1-weighted MRI images through the middle cranial fossa, showing a left temporal fossa homogeneous lesion with CSF signal intensity and no perceptible wall or internal complexity. There is associated remodeling of adjacent calvarium, brain displacement, and a midline shift. These imaging features are typical of an arachnoid cyst.





