Practice Essentials
Mesothelioma is a malignant neoplasm originating from pleural or peritoneal surfaces; this condition is usually associated with occupational exposure to asbestos. Wagner et al connected asbestos to mesothelioma in a classic 1960 study of 33 patients with mesothelioma who were exposed to asbestos in a mining area in South Africa's North Western Cape Province. [1] Of the 33 patients, 32 had been exposed to crocidolite, the most carcinogenic type of asbestos.
Asbestos mining and production peaked from the 1930s-1960s, and asbestos was used in a variety of products ranging from construction supplies to brake linings. During World War II, hundreds of thousands of civilian and military workers, through their occupations, were exposed to asbestos. Production slowed dramatically in the 1970s as the health risks of asbestos became known. Governmental restrictions were placed on its use, and alternative materials became available. Despite these changes, asbestos continues to be used in the manufacture of some fire safety products.
The clinical latency period between asbestos exposure and mesothelioma development is 35-40 years, and as a result, the number of mesothelioma patients has continued to rise despite decreased asbestos production. The most common findings on physical examination (79%) are signs of pleural effusion (eg, dullness to percussion, decreased breath sounds).
The diagnosis of mesothelioma should be made with care. A clinical history of asbestos exposure and radiologic findings that are consistent with mesothelioma warrant inclusion of mesothelioma in the differential diagnosis, but it is important to stress that a diagnosis of mesothelioma cannot be made exclusively with imaging studies. More common diseases, such as benign asbestos-related pleural disease and metastatic adenocarcinoma, can look radiographically identical to mesothelioma. Biopsy with special staining and immunohistochemical and ultrastructural analysis are absolutely essential for the accurate diagnosis of mesothelioma. [2, 3, 4, 5, 6]
Chest radiography is the initial screening examination, while computed tomography (CT) scanning is preferred for staging the tumor. Chest radiography has limited usefulness. The radiographic findings of mesothelioma are nonspecific and are observed in other diseases, including metastatic carcinoma, lymphoma, and benign asbestos disease. Small malignant pleural effusions may not be observed on standard radiographs. Alternatively, large pleural effusions can obscure pleural thickening or masses; therefore, disease extent is frequently underestimated in radiographs.
CT scanning provides more and better information than plain radiography with regard to tumor characteristics and extent. CT is the imaging modality of choice to assess pleural disease and has shown sensitivity and specificity for identifying malignancy. A unilateral pleural effusion is seen in 30-80% of patients. Diffuse pleural thickening or extensive lobular pleural-based masses are seen in about 50% of cases. [3, 7, 8, 9]
Although MRI is superior to CT scanning in some areas, this advantage did not change the surgical treatment in a study by Heelan et al. [10] They compared the accuracy of MRI and CT in preoperative staging of 65 patients with malignant pleural mesothelioma and found that they were nearly equivalent in diagnostic accuracy; however, MRI was found to be more accurate in detecting solitary foci of chest wall invasion and endothoracic fascia involvement and in assessing invasion of the diaphragm. MRI complements CT scanning in some patients. MRI provides better delineation of soft tissues (better soft-tissue contrast) and allows imaging in the sagittal and coronal planes. [11, 12, 13] Neither CT scanning nor MRI provides an unequivocal diagnosis of mesothelioma; tissue biopsy is required for the definitive diagnosis.
Positron emission tomography (PET) scanning may also be useful in delineating the extent of tumor or metastases. [14, 15, 16, 17, 18] Ohno et al reported that whole-body MRI and FDG PET/MRI with signal intensity (SI) had superior diagnostic accuracy for N factor assessment and staging than conventional imaging with FDG PET/MRI without SI assessment and FDG PET/CT in a study comparing imaging evaluations in 23 patients. [19]
The increased metabolic activity of tumor cells causes increased standardized uptake value (SUV) of malignant pleural epithelioma, making PET and PET/CT important complementary techniques. Studies have shown that an SUV cutoff of 2.0-2.2 could differentiate between malignant and benign pleural disease with a sensitivity of 91-100% and a specificity of 78-100%. [20, 21, 22, 23, 24, 25, 26]
Qureshi et al demonstrated that ultrasonography has an overall sensitivity of 79% and specificity of 100% in differentiating malignant from benign effusions. [27]
A study of 164 patients with malignant mesothelioma identified distant metastatic disease in 67% of cases. The most common locations were the contralateral lung (35%), parenchymal lung (26%), and bone (19%). [28] Mesothelioma is very difficult to treat; the treatment is usually surgical, although other treatment options such as chemotherapy and radiotherapy are used. The 2 primary surgical interventions are pleurectomy and extrapleural pneumonectomy (EPP). [29]
Guidelines
All major US and European guidelines recommend the following tests be performed in the initial evaluation and diagnosis of malignant pleural mesothelioma (MPM) [30, 2, 31, 32] :
-
Chest CT with contrast
-
Thoracentesis for cytologic assessment
-
Pleural biopsy (thoracoscopic biopsy is preferred)
In addition, soluble mesothelin-related peptide (SMRP) measurement is optional and may correlate with disease status, according to National Comprehensive Cancer Network (NCCN) guidelines. [32]
Radiography
The most common mesothelioma finding on radiographs is unilateral, concentric, plaquelike, or nodular pleural thickening (as seen in the images below). Pleural effusions are common and may obscure the presence of the underlying pleural thickening. The tumor frequently extends into the fissures, which become thickened and irregular in contour. A slight right-sided predominance is observed, possibly because of a larger pleural surface area. The tumor can rigidly encase the lung, causing compression of lung parenchyma, diaphragm elevation, intercostal space narrowing, and mediastinal shift toward the tumor. Calcified pleural plaques are present in 20% of patients with mesothelioma and are usually related to the previous asbestos exposure.
Lung nodules and hilar masses usually result from direct mesothelioma tumor extension into the lung parenchyma and mediastinal structures, such as lymph nodes, the pericardium, and the heart. Mechanical distortion of the hemithorax, chest wall masses, periosteal rib reaction or rib destruction by the tumor are signs of advanced disease. Although usually unilateral, direct extension of the tumor across the mediastinum into the contralateral hemithorax does occur.
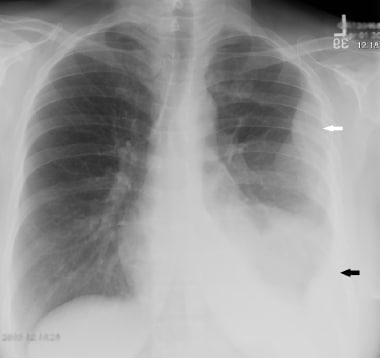
 Chest radiograph (CXR) of a 50-year-old male who presented with chronic dry cough of a few months' duration. The radiograph shows lobulated pleural-based masses in the right hemithorax peripherally (white arrows). Pleural biopsy confirmed malignant mesothelioma. No pleural effusion is present.
Chest radiograph (CXR) of a 50-year-old male who presented with chronic dry cough of a few months' duration. The radiograph shows lobulated pleural-based masses in the right hemithorax peripherally (white arrows). Pleural biopsy confirmed malignant mesothelioma. No pleural effusion is present.
 This 63-year-old woman presented with chest pain. Chest radiograph demonstrates lobulated left pleural-based mass (white arrow) along with a small pleural effusion (black arrow). The lobulated mass was confirmed to be malignant mesothelioma on biopsy.
This 63-year-old woman presented with chest pain. Chest radiograph demonstrates lobulated left pleural-based mass (white arrow) along with a small pleural effusion (black arrow). The lobulated mass was confirmed to be malignant mesothelioma on biopsy.
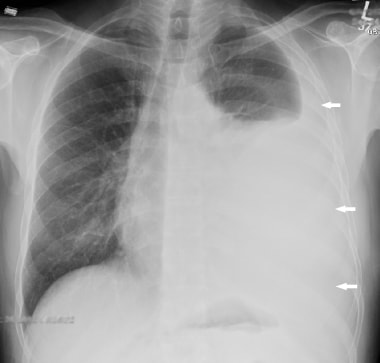 This 57-year-old man presented with shortness of breath. Chest radiograph showed a moderate-sized left pleural effusion (white arrows). Cytology indicated malignant mesothelioma.
This 57-year-old man presented with shortness of breath. Chest radiograph showed a moderate-sized left pleural effusion (white arrows). Cytology indicated malignant mesothelioma.
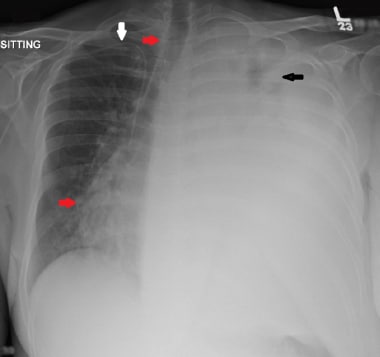 This chest radiograph is of a 47-year-old male patient with known malignant mesothelioma not responding to treatment. There is a large left pleural effusion with very little remaining aeration in the left upper lung (black arrow). There is contralateral tracheal and mediastinal shift (red arrows). A right subclavian central venous access line is in-situ (white arrow).
This chest radiograph is of a 47-year-old male patient with known malignant mesothelioma not responding to treatment. There is a large left pleural effusion with very little remaining aeration in the left upper lung (black arrow). There is contralateral tracheal and mediastinal shift (red arrows). A right subclavian central venous access line is in-situ (white arrow).
Although a definite diagnosis cannot be made on the basis of plain film findings, new unilateral pleural thickening or effusion in a patient who has a history of exposure to asbestos is highly suggestive of mesothelioma.
False-positive diagnosis based on imaging alone could be due to pleural metastases from adenocarcinoma, breast or other primary malignancies, involvement of the pleura by lymphoma or thymoma, or chronic infection. False-negative findings are possible with minimal small focus of pleural involvement by mesothelioma.
Computed Tomography
CT scan findings (examples of which are shown in the images below) are similar to those of plain films but are seen more clearly and in more detail. [33, 34] Furthermore, pleural thickening and effusion can be distinguished with CT scanning. Nodular pleural thickening, pleural thickening greater than 1 cm, involvement of the mediastinal pleural surface, and concentric pleural thickening are all highly suggestive of malignant pleural disease, either mesothelioma or metastases. The tumor extent along the pleural surfaces and into the mediastinum, diaphragm, or chest wall can be evaluated much better with CT scanning than with plain radiography. Chest wall invasion manifests as obliteration of fat planes or chest wall nodules. Diaphragmatic invasion, ascites, and omental caking are common CT scan findings of peritoneal mesothelioma. [3, 7, 8, 35, 36, 9]
Contrast-enhanced CT remains the most-frequent initial imaging technique for clinical staging of malignant pleural mesothelioma. The standard time delay between administration of contrast and CT imaging acquisition is 40-60 sec for optimal enhancement of tissues and opacification of arterial and venous structures. [2, 4, 5, 37, 38]
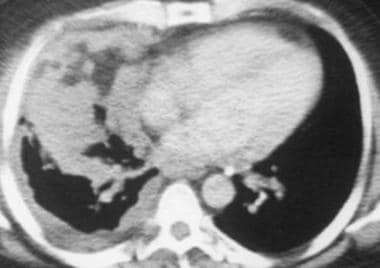
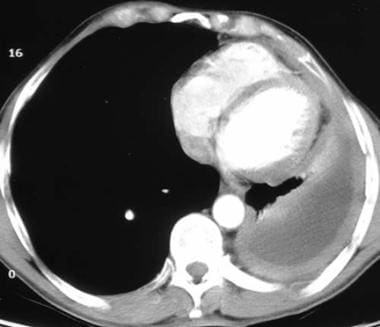 Computed tomography scan of a 58-year-old patient with mesothelioma and shortness of breath. This image shows the extensive pleural thickening that is characteristic of mesothelioma, effusion, and reduction in the volume of the affected hemithorax.
Computed tomography scan of a 58-year-old patient with mesothelioma and shortness of breath. This image shows the extensive pleural thickening that is characteristic of mesothelioma, effusion, and reduction in the volume of the affected hemithorax.
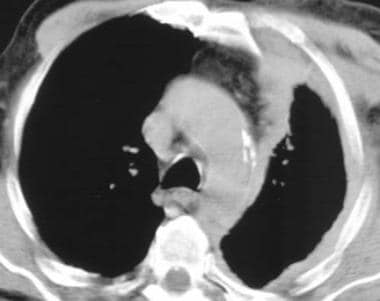
 Computed tomography scan of the chest. This image demonstrates mesothelioma that extends into the chest wall. Note the concentric left pleural thickening, pleural effusion, reduction in volume of the left hemithorax, and the tumor nodules within the chest wall.
Computed tomography scan of the chest. This image demonstrates mesothelioma that extends into the chest wall. Note the concentric left pleural thickening, pleural effusion, reduction in volume of the left hemithorax, and the tumor nodules within the chest wall.
 Computed tomography scan in a 48-year-old man with right-sided chest pain and a "tight sensation," who worked as a welder in a Norfolk, Virginia, shipyard. This image shows that the thick inhomogeneous pleural rind encases the lung (causing volume loss) and extends into the major fissure.
Computed tomography scan in a 48-year-old man with right-sided chest pain and a "tight sensation," who worked as a welder in a Norfolk, Virginia, shipyard. This image shows that the thick inhomogeneous pleural rind encases the lung (causing volume loss) and extends into the major fissure.
 Computed tomography scan in a 70-year-old man with chronic cough, hoarseness, and a 20-lb weight loss over 3-4 months. This image demonstrates the left lung is surrounded by a thickened pleura.
Computed tomography scan in a 70-year-old man with chronic cough, hoarseness, and a 20-lb weight loss over 3-4 months. This image demonstrates the left lung is surrounded by a thickened pleura.
 Computed tomography scan in a 71-year-old man with increasing dyspnea and a history of asbestos exposure several decades earlier. This image shows that the right lung is reduced in volume as a result of the encasing pleural rind. An associated pleural effusion and right lower-lobe rounded atelectasis are also seen.
Computed tomography scan in a 71-year-old man with increasing dyspnea and a history of asbestos exposure several decades earlier. This image shows that the right lung is reduced in volume as a result of the encasing pleural rind. An associated pleural effusion and right lower-lobe rounded atelectasis are also seen.
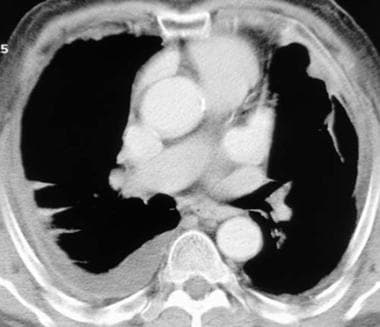
 Computed tomography (CT) scan in a male Veterans Administration patient with a history of asbestos exposure and an enlarging abdominal girth. This upper CT scan slice reveals the calcified pleural plaques along the diaphragmatic surface that are associated with asbestos exposure. Ascites is seen lateral to the liver. Aspiration of the ascitic fluid demonstrated mesothelioma.
Computed tomography (CT) scan in a male Veterans Administration patient with a history of asbestos exposure and an enlarging abdominal girth. This upper CT scan slice reveals the calcified pleural plaques along the diaphragmatic surface that are associated with asbestos exposure. Ascites is seen lateral to the liver. Aspiration of the ascitic fluid demonstrated mesothelioma.
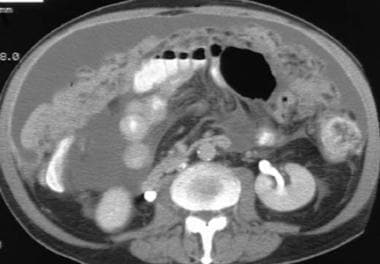 Computed tomography (CT) scan in a male Veterans Administration patient. This lower CT scan slice demonstrates ascites, omental caking, and mesenteric thickening.
Computed tomography (CT) scan in a male Veterans Administration patient. This lower CT scan slice demonstrates ascites, omental caking, and mesenteric thickening.
 Computed tomography scan in a 68-year-old man with known asbestos exposure. Multiple biopsies were negative for mesothelioma, and the chest findings were attributed to benign, asbestos-related pleural disease, which is a diagnosis of exclusion.
Computed tomography scan in a 68-year-old man with known asbestos exposure. Multiple biopsies were negative for mesothelioma, and the chest findings were attributed to benign, asbestos-related pleural disease, which is a diagnosis of exclusion.
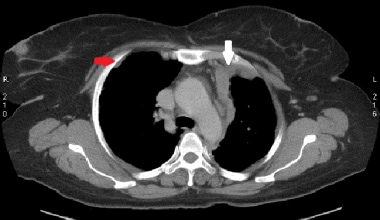 Axial slice from staging chest CT scan and biopsy in a 52-year-old woman confirmed malignant mesothelioma. There is lobulated irregular mediastinal and anterior parietal pleural thickening (white arrow). A non-calcified pleural plaque is visible on the right (red arrow).
Axial slice from staging chest CT scan and biopsy in a 52-year-old woman confirmed malignant mesothelioma. There is lobulated irregular mediastinal and anterior parietal pleural thickening (white arrow). A non-calcified pleural plaque is visible on the right (red arrow).
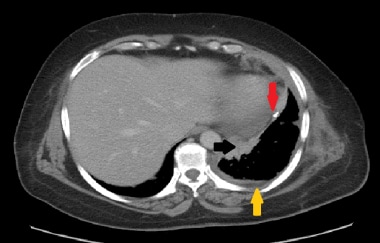 Axial slice from staging CT scan of a 67-year-old male construction worker. There is irregular pleural thickening due to malignant mesothelioma (black arrow). There is also a trace of pleural effusion (yellow arrow). A calcified pleural plaque can be seen, which is a hallmark of previous asbestos exposure (red arrow). Approximately 80% of malignant mesotheliomas occur in individuals who have been exposed to asbestos.
Axial slice from staging CT scan of a 67-year-old male construction worker. There is irregular pleural thickening due to malignant mesothelioma (black arrow). There is also a trace of pleural effusion (yellow arrow). A calcified pleural plaque can be seen, which is a hallmark of previous asbestos exposure (red arrow). Approximately 80% of malignant mesotheliomas occur in individuals who have been exposed to asbestos.
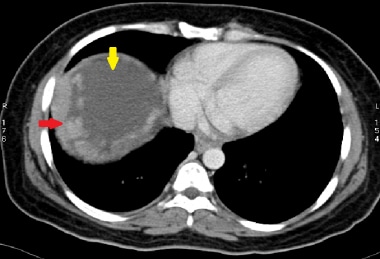
 A case of early right pleural malignant mesothelioma (red arrow). The CT scan was acquired without administering intravenous contrast due to renal impairment. There is also a small ipsilateral pleural effusion (yellow arrow).
A case of early right pleural malignant mesothelioma (red arrow). The CT scan was acquired without administering intravenous contrast due to renal impairment. There is also a small ipsilateral pleural effusion (yellow arrow).
 This 58-year-old patient presented with abdominal fullness. Axial slice from a CT scan shows irregular peritoneal thickening (red arrow), confirmed to be epithelioid malignant mesothelioma. There is also free fluid below the diaphragm (yellow arrow).
This 58-year-old patient presented with abdominal fullness. Axial slice from a CT scan shows irregular peritoneal thickening (red arrow), confirmed to be epithelioid malignant mesothelioma. There is also free fluid below the diaphragm (yellow arrow).
 Another case of malignant peritoneal mesothelioma in a 51-year-old man. There are irregular, enhancing peritoneal masses in the right upper abdomen (yellow arrows) with significant ascites. There is also omental caking (red arrow).
Another case of malignant peritoneal mesothelioma in a 51-year-old man. There are irregular, enhancing peritoneal masses in the right upper abdomen (yellow arrows) with significant ascites. There is also omental caking (red arrow).
 Coronal reformat from staging CT scan of a 70-year-old female patient with advanced left pleural malignant mesothelioma. There is a large heterogeneously enhancing mass occupying the lower left hemithorax (blue asterisk). There is complete encasement of the left hemithorax (green arrows). There is invasion of the mediastinum (red arrow) as well as early invasion into the lateral chest wall (yellow arrow).
Coronal reformat from staging CT scan of a 70-year-old female patient with advanced left pleural malignant mesothelioma. There is a large heterogeneously enhancing mass occupying the lower left hemithorax (blue asterisk). There is complete encasement of the left hemithorax (green arrows). There is invasion of the mediastinum (red arrow) as well as early invasion into the lateral chest wall (yellow arrow).
Magnetic Resonance Imaging
MRI produces images (an example is of which is shown below) in multiple planes and is superior to CT scanning in demonstrating solitary foci of chest wall invasion, endothoracic fascial involvement, and diaphragmatic invasion. [34, 39] Mesothelioma images on MRI demonstrate iso-intense T1 signals relative to the chest wall musculature and mild to moderately increased signals on T2-weighted images or enhancement on T1-weighted images that have been obtained following injection of gadolinium. Fibrous pleural plaques are usually isointense or less intense relative to muscle. Inflammatory pleural disease may mimic the increased MRI signal intensity of mesothelioma. [40]
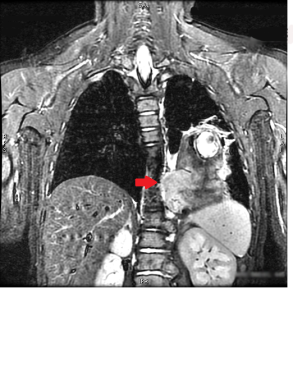
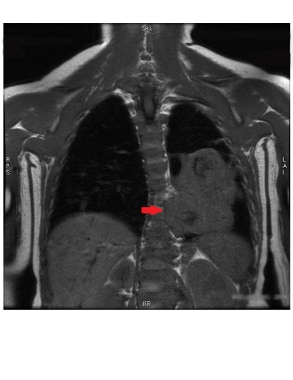 This T1-weighted coronal image shows malignant mesothelioma, which is isointense to the muscles. MRI has superior soft tissue resolution, with clear evidence of mediastinal invasion on this image (red arrow).
This T1-weighted coronal image shows malignant mesothelioma, which is isointense to the muscles. MRI has superior soft tissue resolution, with clear evidence of mediastinal invasion on this image (red arrow).
 This coronal T2-weighted STIR image demonstrates malignant mesothelioma to have slightly higher intensity than muscles (red arrow). These tumors can also be isointense to the muscles on T2-weighted sequences.
This coronal T2-weighted STIR image demonstrates malignant mesothelioma to have slightly higher intensity than muscles (red arrow). These tumors can also be isointense to the muscles on T2-weighted sequences.
 This gradient echo sagittal MRI image clearly shows evidence of malignant mesothelioma invasion into the chest wall (red arrows). MRI has superb soft tissue resolution and hence can help in cases where chest wall invasion is not clear on another imaging modalities.
This gradient echo sagittal MRI image clearly shows evidence of malignant mesothelioma invasion into the chest wall (red arrows). MRI has superb soft tissue resolution and hence can help in cases where chest wall invasion is not clear on another imaging modalities.
 Magnetic resonance imaging (MRI) scan in a 72-year-old Veterans Administration patient with left-sided mesothelioma. Note that the MRI scan well delineates the soft tissues and, in particular, the thoracoabdominal interface at the diaphragm.
Magnetic resonance imaging (MRI) scan in a 72-year-old Veterans Administration patient with left-sided mesothelioma. Note that the MRI scan well delineates the soft tissues and, in particular, the thoracoabdominal interface at the diaphragm.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Ultrasonography
Ultrasonography can demonstrate pleural thickening or effusions in patients with mesothelioma. This modality can be used as a guide for biopsy, but it is not typically used to assess the extent of disease in patients with mesothelioma. Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is an important diagnostic tool for malignant pleural mesothelioma (MPM). [41, 42, 43] Qureshi et al demonstrated that ultrasonography has an overall sensitivity of 79% and specificity of 100% in differentiating malignant from benign effusions. [27]
(See the images below.)
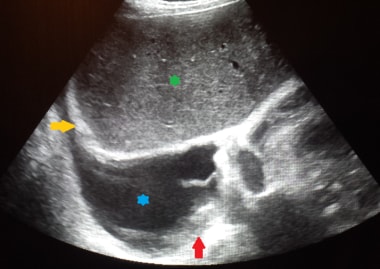 This ultrasound image of the right lower chest demonstrates biopsy proven malignant pleural mesothelioma (red arrow). There is a small to moderate pleural effusion (blue asterisk). Echogenic right hemidiaphragm (yellow arrow) and liver (green asterisk) are also visualised.
This ultrasound image of the right lower chest demonstrates biopsy proven malignant pleural mesothelioma (red arrow). There is a small to moderate pleural effusion (blue asterisk). Echogenic right hemidiaphragm (yellow arrow) and liver (green asterisk) are also visualised.
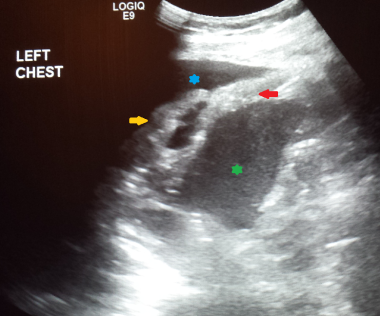 Left chest ultrasound in this patient demonstrated localized pleural thickening, subsequently confirmed as malignant mesothelioma (red arrow). The patient had presented with shortness of breath and easy fatigability. Collapsed left lower pulmonary lobe can be seen (yellow arrow) within pleural effusion (blue asterisk). Spleen is also visualized (green asterisk).
Left chest ultrasound in this patient demonstrated localized pleural thickening, subsequently confirmed as malignant mesothelioma (red arrow). The patient had presented with shortness of breath and easy fatigability. Collapsed left lower pulmonary lobe can be seen (yellow arrow) within pleural effusion (blue asterisk). Spleen is also visualized (green asterisk).
Nuclear Imaging
PET/CT
If surgical resection of the tumor is a possibility, a quantitative ventilation-perfusion scan helps in assessing the function of the contralateral lung.
Positron emission tomography (PET) scanning has been used, although not routinely, to evaluate mesothelioma and may help preoperatively by documenting the extent of lymph node involvement or distant metastases. [11, 14, 44, 45, 46, 47]
Yildirim et al examined the efficacy of using 2-[fluorine-18]fluoro-2-deoxy-D-glucose (FDG) PET and CT scanning together to differentiate malignant mesothelioma from asbestos-related benign pleural disease. In a study of 31 patients (17 with malignant mesotheliomas, 9 with benign asbestos pleurisies, 5 with diffuse pleural fibrosis), the authors found that FDG PET/CT scanning accurately detected malignant lesions in 15 of the 17 patients with these neoplasms and that the combined modalities had a sensitivity of 88.2%, specificity of 92.9%, and overall accuracy of 90.3%. In addition, benign pleural disease was correctly detected in 13 of 14 patients. [44]
A study by Mavi et al concluded that dual time-point FDG PET scanning seems to be an accurate means of differentiating malignant mesothelioma from benign pleural disease. In the study, which involved 55 patients, the authors found that at the second time point, FDG uptake in malignant lesions had increased over that at the first time point, while in benign lesions, uptake at the second time point had generally remained stable or had decreased. [45]
Evidence from a similar study by Yamamoto et al also suggested that dual time-point FDG PET is useful for differentiating malignant pleural mesothelioma from benign pleural lesions. [46, 48, 49, 50]
Pleural inflammation can also reveal increased uptake on PET scanning.
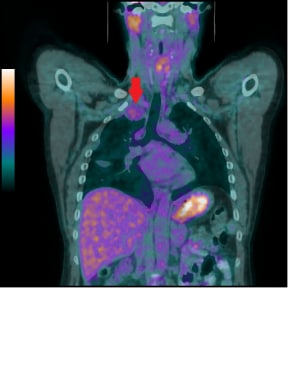
 This coronal 18F-FDG PET/CT demonstrates a markedly FDG avid (SUVmax 11.2) biopsy-proven malignant mesothelioma (red arrows). Physiologic tracer activity is also visible in the brain and urinary bladder.
This coronal 18F-FDG PET/CT demonstrates a markedly FDG avid (SUVmax 11.2) biopsy-proven malignant mesothelioma (red arrows). Physiologic tracer activity is also visible in the brain and urinary bladder.
 Malignant mesotheliomas are not always very FDG avid. In this case, only background-level FDG avidity (SUVmax 2.1) was demonstrated by the right apical malignant mesothelioma (red arrow).
Malignant mesotheliomas are not always very FDG avid. In this case, only background-level FDG avidity (SUVmax 2.1) was demonstrated by the right apical malignant mesothelioma (red arrow).
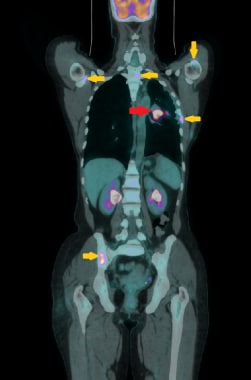 18F-FDG PET/CT demonstrates moderate FDG avidity (SUVmax 7.8) recurrence of malignant mesothelioma in the left lung (red arrow), along with scattered bone metastases (yellow arrows).
18F-FDG PET/CT demonstrates moderate FDG avidity (SUVmax 7.8) recurrence of malignant mesothelioma in the left lung (red arrow), along with scattered bone metastases (yellow arrows).
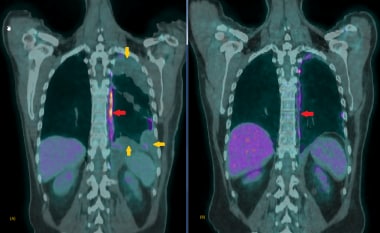 A relatively new and exciting application of 18F-FDG PET/CT is post-therapy response evaluation. Here is a case of malignant mesothelioma before (A) and after (B) systemic treatment. There is a partial response to treatment evidenced by the reduction in bulk and FDG avidity of the disease (red arrows). The SUVmax pre-treatment was 8.1, while that after treatment was 2.2. There is also interval reduction in pleural thickening and effusion (yellow arrows).
A relatively new and exciting application of 18F-FDG PET/CT is post-therapy response evaluation. Here is a case of malignant mesothelioma before (A) and after (B) systemic treatment. There is a partial response to treatment evidenced by the reduction in bulk and FDG avidity of the disease (red arrows). The SUVmax pre-treatment was 8.1, while that after treatment was 2.2. There is also interval reduction in pleural thickening and effusion (yellow arrows).
-
Chest radiograph (CXR) of a 50-year-old male who presented with chronic dry cough of a few months' duration. The radiograph shows lobulated pleural-based masses in the right hemithorax peripherally (white arrows). Pleural biopsy confirmed malignant mesothelioma. No pleural effusion is present.
-
This 63-year-old woman presented with chest pain. Chest radiograph demonstrates lobulated left pleural-based mass (white arrow) along with a small pleural effusion (black arrow). The lobulated mass was confirmed to be malignant mesothelioma on biopsy.
-
This 57-year-old man presented with shortness of breath. Chest radiograph showed a moderate-sized left pleural effusion (white arrows). Cytology indicated malignant mesothelioma.
-
This chest radiograph is of a 47-year-old male patient with known malignant mesothelioma not responding to treatment. There is a large left pleural effusion with very little remaining aeration in the left upper lung (black arrow). There is contralateral tracheal and mediastinal shift (red arrows). A right subclavian central venous access line is in-situ (white arrow).
-
Axial slice from staging chest CT scan and biopsy in a 52-year-old woman confirmed malignant mesothelioma. There is lobulated irregular mediastinal and anterior parietal pleural thickening (white arrow). A non-calcified pleural plaque is visible on the right (red arrow).
-
Axial slice from staging CT scan of a 67-year-old male construction worker. There is irregular pleural thickening due to malignant mesothelioma (black arrow). There is also a trace of pleural effusion (yellow arrow). A calcified pleural plaque can be seen, which is a hallmark of previous asbestos exposure (red arrow). Approximately 80% of malignant mesotheliomas occur in individuals who have been exposed to asbestos.
-
A case of early right pleural malignant mesothelioma (red arrow). The CT scan was acquired without administering intravenous contrast due to renal impairment. There is also a small ipsilateral pleural effusion (yellow arrow).
-
This 58-year-old patient presented with abdominal fullness. Axial slice from a CT scan shows irregular peritoneal thickening (red arrow), confirmed to be epithelioid malignant mesothelioma. There is also free fluid below the diaphragm (yellow arrow).
-
Another case of malignant peritoneal mesothelioma in a 51-year-old man. There are irregular, enhancing peritoneal masses in the right upper abdomen (yellow arrows) with significant ascites. There is also omental caking (red arrow).
-
Coronal reformat from staging CT scan of a 70-year-old female patient with advanced left pleural malignant mesothelioma. There is a large heterogeneously enhancing mass occupying the lower left hemithorax (blue asterisk). There is complete encasement of the left hemithorax (green arrows). There is invasion of the mediastinum (red arrow) as well as early invasion into the lateral chest wall (yellow arrow).
-
This ultrasound image of the right lower chest demonstrates biopsy proven malignant pleural mesothelioma (red arrow). There is a small to moderate pleural effusion (blue asterisk). Echogenic right hemidiaphragm (yellow arrow) and liver (green asterisk) are also visualised.
-
Left chest ultrasound in this patient demonstrated localized pleural thickening, subsequently confirmed as malignant mesothelioma (red arrow). The patient had presented with shortness of breath and easy fatigability. Collapsed left lower pulmonary lobe can be seen (yellow arrow) within pleural effusion (blue asterisk). Spleen is also visualized (green asterisk).
-
This T1-weighted coronal image shows malignant mesothelioma, which is isointense to the muscles. MRI has superior soft tissue resolution, with clear evidence of mediastinal invasion on this image (red arrow).
-
This coronal T2-weighted STIR image demonstrates malignant mesothelioma to have slightly higher intensity than muscles (red arrow). These tumors can also be isointense to the muscles on T2-weighted sequences.
-
This gradient echo sagittal MRI image clearly shows evidence of malignant mesothelioma invasion into the chest wall (red arrows). MRI has superb soft tissue resolution and hence can help in cases where chest wall invasion is not clear on another imaging modalities.
-
This coronal 18F-FDG PET/CT demonstrates a markedly FDG avid (SUVmax 11.2) biopsy-proven malignant mesothelioma (red arrows). Physiologic tracer activity is also visible in the brain and urinary bladder.
-
Malignant mesotheliomas are not always very FDG avid. In this case, only background-level FDG avidity (SUVmax 2.1) was demonstrated by the right apical malignant mesothelioma (red arrow).
-
18F-FDG PET/CT demonstrates moderate FDG avidity (SUVmax 7.8) recurrence of malignant mesothelioma in the left lung (red arrow), along with scattered bone metastases (yellow arrows).
-
A relatively new and exciting application of 18F-FDG PET/CT is post-therapy response evaluation. Here is a case of malignant mesothelioma before (A) and after (B) systemic treatment. There is a partial response to treatment evidenced by the reduction in bulk and FDG avidity of the disease (red arrows). The SUVmax pre-treatment was 8.1, while that after treatment was 2.2. There is also interval reduction in pleural thickening and effusion (yellow arrows).
-
Chest radiograph of a 65-year-old man with left-sided chest pain and biopsy-proven mesothelioma. The left lateral pleura is thickened and lobulated, which is often observed with mesothelioma.
-
Chest radiograph of a 58-year-old patient with mesothelioma and shortness of breath. This image reveals diffuse, left-sided pleural thickening, a pleural effusion, and ipsilateral volume loss.
-
Computed tomography scan of a 58-year-old patient with mesothelioma and shortness of breath. This image shows the extensive pleural thickening that is characteristic of mesothelioma, effusion, and reduction in the volume of the affected hemithorax.
-
Chest radiograph of 65-year-old woman with a history of mastectomy for breast cancer who had recurrent pleural and parenchymal metastases. This lateral chest radiograph demonstrates thickening of the major fissure and blunting of the posterior costophrenic angle. This appearance is indistinguishable from that of mesothelioma.
-
Computed tomography scan in a 68-year-old man with known asbestos exposure. Multiple biopsies were negative for mesothelioma, and the chest findings were attributed to benign, asbestos-related pleural disease, which is a diagnosis of exclusion.
-
Computed tomography scan of the chest. This image demonstrates mesothelioma that extends into the chest wall. Note the concentric left pleural thickening, pleural effusion, reduction in volume of the left hemithorax, and the tumor nodules within the chest wall.
-
Computed tomography scan in a 48-year-old man with right-sided chest pain and a "tight sensation," who worked as a welder in a Norfolk, Virginia, shipyard. This image shows that the thick inhomogeneous pleural rind encases the lung (causing volume loss) and extends into the major fissure.
-
Computed tomography scan in a 70-year-old man with chronic cough, hoarseness, and a 20-lb weight loss over 3-4 months. This image demonstrates the left lung is surrounded by a thickened pleura.
-
Computed tomography scan in a 71-year-old man with increasing dyspnea and a history of asbestos exposure several decades earlier. This image shows that the right lung is reduced in volume as a result of the encasing pleural rind. An associated pleural effusion and right lower-lobe rounded atelectasis are also seen.
-
Magnetic resonance imaging (MRI) scan in a 72-year-old Veterans Administration patient with left-sided mesothelioma. Note that the MRI scan well delineates the soft tissues and, in particular, the thoracoabdominal interface at the diaphragm.
-
Computed tomography (CT) scan in a male Veterans Administration patient with a history of asbestos exposure and an enlarging abdominal girth. This upper CT scan slice reveals the calcified pleural plaques along the diaphragmatic surface that are associated with asbestos exposure. Ascites is seen lateral to the liver. Aspiration of the ascitic fluid demonstrated mesothelioma.
-
Computed tomography (CT) scan in a male Veterans Administration patient. This lower CT scan slice demonstrates ascites, omental caking, and mesenteric thickening.






