Practice Essentials
Solitary fibrous tumors of the pleura (SFTPs) are rare, slow-growing tumors that arise from CD34-positive dendritic mesenchymal cells and represent less than 5% of all tumors of the pleura. SFTPs commonly arise from the submesothelial fibroblasts of the visceral pleura rather than the parietal pleura and are often larger than 10 cm. SFTPs are benign in up to 80% of cases, but they can become malignant. Large tumors (>15 cm) may compress the trachea and lung tissue, causing cough, chest tightness, dyspnea, and even respiratory insufficiency. [1, 2, 3, 4]
SFTPs exist in benign and malignant forms. Only rarely is the localized fibrous tumor invasive or does it cause local recurrence after resection. The ratio of benign to malignant tumors is 7:1. The diagnosis of SFTP is important because the tumor is potentially resectable for cure despite its typically large size. In many cases, resection can repeatedly be used to treat recurrence, although usually with increasing difficulty. [5, 6, 7, 8]
Often, SFTP is discovered incidentally on chest radiographs. Most patients are asymptomatic until the tumor grows large and has a compressive effect causing cough, chest pain, or dyspnea. [9] Other reported symptoms include digital clubbing, pleural effusion, and, in rare cases, refractory hypoglycemia. [9, 10]
Findings on CT and MRI can suggest the diagnosis of SFTP. However, histopathologic examination is needed for a definitive diagnosis. [11, 12, 13] Nuclear STAT6 immunoreactivity can be helpful in cases where the diagnosis is uncertain. [14]
Chest radiographic findings are nonspecific, and the lesion can sometimes be obscured by associated pleural effusion. CT and MRI scans may show characteristic findings that are suggestive of SFTP but that are not always pathognomonic. The pleural origin of large lesions can be difficult to detect, especially on chest radiographs and even on CT and MRI scans.
(An example of a benign SFTP is shown in the images below.)
 Posteroanterior chest radiograph in a 70-year-old woman who presented with chest discomfort. A well-circumscribed, pleural-based mass is seen in the upper left hemithorax. The angle between the mass and the chest wall is obtuse. The lesion was resected and found to be a benign localized fibrous tumor of the pleura.
Posteroanterior chest radiograph in a 70-year-old woman who presented with chest discomfort. A well-circumscribed, pleural-based mass is seen in the upper left hemithorax. The angle between the mass and the chest wall is obtuse. The lesion was resected and found to be a benign localized fibrous tumor of the pleura.
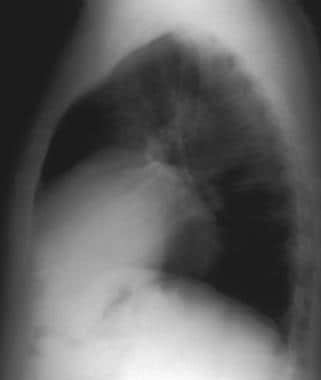
 Lateral chest radiograph in a 70-year-old woman who presented with chest discomfort (same patient as in the previous image).
Lateral chest radiograph in a 70-year-old woman who presented with chest discomfort (same patient as in the previous image).
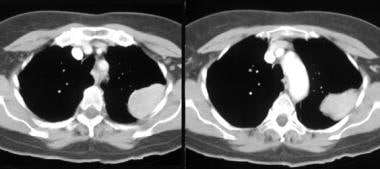 Chest computed tomography (CT) scans in a 70-year-old woman who presented with chest discomfort demonstrate a pleural, noncalcified soft-tissue mass with smooth, lobulated margins (same patient as in the previous 2 images). The mass enhances slightly more than the soft tissue of the chest wall. No evidence of chest wall invasion is seen.
Chest computed tomography (CT) scans in a 70-year-old woman who presented with chest discomfort demonstrate a pleural, noncalcified soft-tissue mass with smooth, lobulated margins (same patient as in the previous 2 images). The mass enhances slightly more than the soft tissue of the chest wall. No evidence of chest wall invasion is seen.
Radiography
In most patients, an SFTP is detected as an incidental finding on a chest radiograph, appearing as a well-circumscribed, homogeneous soft-tissue mass that is related closely to the pleura.
The lesion can arise anywhere along the pleura and can even be seen in the pulmonary fissures or along the mediastinal or diaphragmatic pleura (see the images below).
 Posteroanterior chest radiograph shows that a small mass projects over the left mediastinal margin, inferior to the left hilum.
Posteroanterior chest radiograph shows that a small mass projects over the left mediastinal margin, inferior to the left hilum.
 Lateral chest radiograph in the same patient as in the previous image demonstrates the mass overlying the middle mediastinum and deforming the anterior cardiovascular contour.
Lateral chest radiograph in the same patient as in the previous image demonstrates the mass overlying the middle mediastinum and deforming the anterior cardiovascular contour.
The margins with lung parenchyma are well defined in most patients, although in 2% of patients, the lesion is somewhat ill defined, and in another 2% of patients, the lesion is completely obscured by pleural effusion.
The angle with the chest wall or mediastinum is either acute (as seen in the images below) or obtuse. The obtuse angle is seen more often in small lesions, indicating the pleural origin of the lesion.
 Posteroanterior chest radiograph shows a mass with sharp, smooth margins in the upper right hemithorax. The angle between the lesion and the chest wall is acute.
Posteroanterior chest radiograph shows a mass with sharp, smooth margins in the upper right hemithorax. The angle between the lesion and the chest wall is acute.
Large tumors may present as an opaque hemithorax (as demonstrated in the images below).
 Posteroanterior chest radiograph shows a large mass in the lower right hemithorax, abutting the mediastinum and the right hemidiaphragm. A portion of the mass margin is obscured by adjacent minimal atelectasis.
Posteroanterior chest radiograph shows a large mass in the lower right hemithorax, abutting the mediastinum and the right hemidiaphragm. A portion of the mass margin is obscured by adjacent minimal atelectasis.
 Lateral chest radiograph in the same patient as in the previous image. The described mass is overlying the cardiac shadow.
Lateral chest radiograph in the same patient as in the previous image. The described mass is overlying the cardiac shadow.
Pleural effusion may occur in 17% of patients, especially in patients with the malignant variant of SFTP.
Chest radiographic findings are nonspecific; however, a change in the position of the lesion with respiration or gravity is particularly suggestive of a pedunculated SFTP.
The lesion may mimic a mass of parenchymal or mediastinal origin, and large lesions may simulate an elevated diaphragm.
(See the images below.)
Computed Tomography
Typically, an SFTP lesion appears as a smoothly marginated, soft-tissue–attenuating mass abutting the pleura, with a round or lobulated contour. On contrast-enhanced CT scans, the lesion enhances more than the soft tissue does, because of its rich vascularization. Nonenhancing areas within the mass are correlated with the presence of necrosis, hemorrhage, or degeneration.
Areas of low attenuation can be seen within an SFTP, especially when the lesion is large. Unlike other pleural lesions, the angle between the mass and the pleura is most often acute (although it can be obtuse, especially in small masses). A small, ipsilateral pleural effusion can be seen. Calcification is not common, but it can be seen. The detection of a pedicle or a change in the lesion's position is suggestive of an SFTP.
The lesion displaces the adjacent mediastinum and lung parenchyma, resulting in atelectasis.
The malignant form of SFTP cannot be confidently differentiated from the benign form by imaging. However, malignant lesions are typically larger than 10 cm and are more likely to be associated with central necrosis and a large pleural effusion.
Manifestations of SFTP on CT scans are usually not pathognomonic, although some CT findings are highly suggestive of the diagnosis.
Small lesions may mimic primary lung carcinoma; however, a localized fibrous tumor is not associated with metastases or lymphadenopathy.
In a study of CT characteristics of 60 benign and malignant SFTPs (49 benign, 11 malignant; diameters 1.1 to 18.9 cm), CT revealed characteristic patterns, including casting mold-like growth, rich blood supply, and geographic-patterned enhancement. Larger tumor size, inhomogeneous intensities, abundant intratumor blood vessels, and pleural effusions were more common with malignant tumors. Multislice CT angiography revealed feeding arteries and helped guide surgical management. [2]
Magnetic Resonance Imaging
Spin-echo, T1-weighted MRI scans predominantly demonstrate low to intermediate signal intensity, and T2-weighted images depict low signal intensity. The low intensity is attributed to the presence of fibrous, hypocellular tissue.
Foci of increased signal intensity can be seen on T2-weighted images. These foci correspond to the regions of decreased attenuation on CT scans and represent areas of necrosis, hemorrhage, or degeneration.
Intense enhancement is seen on gadolinium-enhanced T1-weighted images.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or magnetic resonance angiography scans. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
MRI machines can produce multiplanar images, and MRI has superior tissue characterization as compared to CT scanning; therefore, MRI is helpful in evaluating an SFTP and in defining its pleural origin and extension. After excluding calcifications, the presence of low signal intensity on T1- and T2-weighted images is highly suggestive of the fibrous nature of the lesion.
(T1- and T2-weighted images are shown below.)
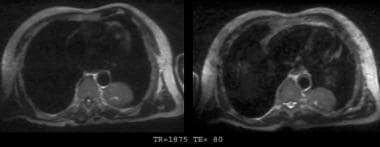
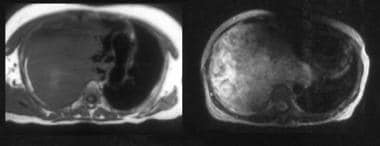 Magnetic resonance images of the chest in a 51-year-old woman. Left, T1-weighted image. Right, T2-weighted image. A large, heterogeneous mass is located in the right hemithorax. A significant associated mediastinal shift is seen, with no chest wall or mediastinal invasion. The mass has relatively low signal intensity on the T1-weighted image and has slightly increased signal intensity on the T2-weighted image.
Magnetic resonance images of the chest in a 51-year-old woman. Left, T1-weighted image. Right, T2-weighted image. A large, heterogeneous mass is located in the right hemithorax. A significant associated mediastinal shift is seen, with no chest wall or mediastinal invasion. The mass has relatively low signal intensity on the T1-weighted image and has slightly increased signal intensity on the T2-weighted image.
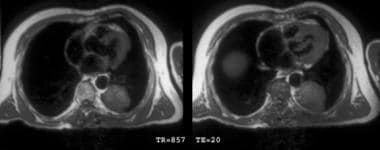 T1-weighted chest magnetic resonance images show a low–signal-intensity mass in the posterior aspect of the left hemithorax.
T1-weighted chest magnetic resonance images show a low–signal-intensity mass in the posterior aspect of the left hemithorax.
Ultrasonography
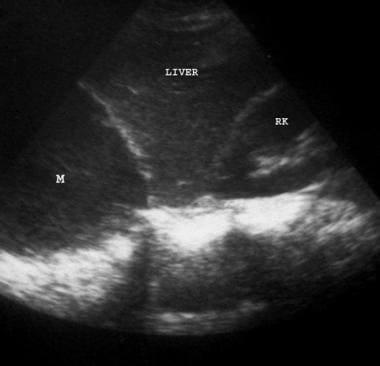
Ultrasonography plays a limited role in the diagnostic workup of pleural masses. [15] In some patients, however, ultrasonography may be performed to evaluate a pleural effusion or to guide procedures. The fibrous tumor typically demonstrates homogeneous low echogenicity, as in the image below. Associated pleural effusion appears anechoic.
Nuclear Imaging
A case report described the potential use of a fluorodeoxyglucose–positron emission tomography (FDG-PET) scan to evaluate the possibility of malignancy in SFTP. In this report, a high FDG uptake (with a standardized uptake ratio [SUR] of 3.0) was noted in a portion of the mass that exhibited malignant features histopathologically. [16] The article suggested that FDG-PET can be helpful to determine preoperatively the presence of malignancy in patients with SFTP, whose prognoses are usually difficult to predict. Yan et al report a case in which a PET diagnosis was confirmed by pathology. [17]
-
Posteroanterior chest radiograph in a 70-year-old woman who presented with chest discomfort. A well-circumscribed, pleural-based mass is seen in the upper left hemithorax. The angle between the mass and the chest wall is obtuse. The lesion was resected and found to be a benign localized fibrous tumor of the pleura.
-
Lateral chest radiograph in a 70-year-old woman who presented with chest discomfort (same patient as in the previous image).
-
Chest computed tomography (CT) scans in a 70-year-old woman who presented with chest discomfort demonstrate a pleural, noncalcified soft-tissue mass with smooth, lobulated margins (same patient as in the previous 2 images). The mass enhances slightly more than the soft tissue of the chest wall. No evidence of chest wall invasion is seen.
-
Posteroanterior chest radiograph shows a mass with sharp, smooth margins in the upper right hemithorax. The angle between the lesion and the chest wall is acute.
-
Lateral chest radiograph in the same patient as in the previous image.
-
Posteroanterior chest radiograph shows a large mass in the lower right hemithorax, abutting the mediastinum and the right hemidiaphragm. A portion of the mass margin is obscured by adjacent minimal atelectasis.
-
Lateral chest radiograph in the same patient as in the previous image. The described mass is overlying the cardiac shadow.
-
Computed tomography (CT) scans of the chest demonstrate a large, somewhat heterogeneous soft-tissue mass in the right hemithorax. A mild mediastinal shift is due to the mass. The mass has well-defined, smooth margins. No evidence of chest wall or mediastinal invasion is noted.
-
Posteroanterior chest radiograph in a 78-year-old man reveals a large, homogeneous opacity in the left hemithorax; this is partially obscured by associated pleural effusion.
-
Computed tomography (CT) scans of the chest in a 78-year-old man demonstrate an inhomogeneous soft-tissue mass with well-defined margins and a central area of decreased attenuation (same patient as in the previous image). The configuration of the mass suggests that it resides within the major fissure. A small amount of compressive atelectasis is identified in the left upper lobe. No evidence of adjacent rib erosion or extension through the chest wall is seen. Small, bilateral pleural effusions are present.
-
Posteroanterior chest radiograph shows that a small mass projects over the left mediastinal margin, inferior to the left hilum.
-
Lateral chest radiograph in the same patient as in the previous image demonstrates the mass overlying the middle mediastinum and deforming the anterior cardiovascular contour.
-
Posteroanterior chest radiograph shows that a retrocardiac mass with smooth margins abuts the medial aspect of the left hemidiaphragm.
-
Lateral chest radiograph in the same patient as in the previous image. A mass with smooth margins abuts the posterior aspect of the left hemidiaphragm. The angle between the mass and the diaphragm is acute.
-
Posteroanterior chest radiograph shows a large mass in the lower right hemithorax. The mass abuts the mediastinum and the right hemidiaphragm, mimicking the elevation of the right hemidiaphragm.
-
Lateral chest radiograph in the same patient as in the previous image.
-
Ultrasonogram of the lower right chest. A hypoechoic, homogeneous mass (M) is compressing the right diaphragm and displacing the liver inferiorly.
-
Contrast-enhanced chest computed tomography (CT) scans in a 51-year-old woman demonstrate a large, heterogeneous mass in the right hemithorax. A significant associated mediastinal shift is present. No chest wall invasion is noted, and a fat plane is separating the aorta and the esophagus from the mass.
-
Magnetic resonance images of the chest in a 51-year-old woman. Left, T1-weighted image. Right, T2-weighted image. A large, heterogeneous mass is located in the right hemithorax. A significant associated mediastinal shift is seen, with no chest wall or mediastinal invasion. The mass has relatively low signal intensity on the T1-weighted image and has slightly increased signal intensity on the T2-weighted image.
-
T1-weighted chest magnetic resonance images show a low–signal-intensity mass in the posterior aspect of the left hemithorax.
-
T2-weighted magnetic resonance images of the same patient as in the previous image. The noted mass has low signal intensity, with a linear focal area of increased signal intensity (necrosis vs degeneration).
-
Chest computed tomography (CT) scans demonstrate a large, heterogeneous mass in the left hemithorax. An associated mediastinal shift is present, with no chest wall invasion.
-
Angiography in the same patient as in the previous image. The right hemithorax mass demonstrates increased vascularity.
-
Gross pathologic specimen of a resected tumor shows a well-circumscribed, encapsulated mass.