Practice Essentials
Traumatic aortic disruption is a time-sensitive injury requiring rapid and accurate diagnosis to prevent death. Although the clinical, or mechanism, score is of primary importance in the prompt diagnosis of patients with traumatic aortic injury (TAI), the radiologic findings play a vital supportive role. TAI is initially characterized by contained rupture (pseudoaneurysm), which is relatively clinically silent. After a variable period of time, contained rupture is followed by a rapid transition to free, uncontained pseudoaneurysm rupture; exsanguination; and death. The clinical challenges are to rapidly stabilize the patient and then transport the patient to a level I trauma center for evaluation, diagnosis, and definitive treatment before free rupture occurs. [1, 2]
Approximately 80% of patients with acute TAI will die before reaching the hospital. In a Japanese study by Katayama et al, later timing of the first CT scanning was associated with a higher incidence of death. Patients were divided into 3 groups: early (≤26 min), middle (27-40 min), and late (≥41 min) phases, based on the time interval from hospital arrival to start of first CT scanning. A total of 421 patients were assessed. Mortality was 7.7% (11/142) for the early group, 11.1% (15/135) for the middle group, and 17.6% (25/144) for the late group. [1, 3, 2, 4]
Blunt TAI results most frequently from high impact deceleration (eg, high-velocity motor vehicle accidents) and falls from a height. It is important that radiologists are familiar with both the direct (intimal flap, pseudoaneurysm, aortic contour irregularity and contrast extravasation) and indirect (periaortic haematoma) imaging findings. [5]
Signs of an underlying aortic injury include widening of the mediastinum, apical pleural capping, an abnormal aortic contour, and deviation of an endotracheal or nasogastric tube to the right. Chest radiographs can be helpful but should not delay cross-sectional imaging if warranted. Chest radiography is better used to assess for life-threatening injuries, such as tension pneumothorax and a large hemothorax requiring immediate drainage. [5]
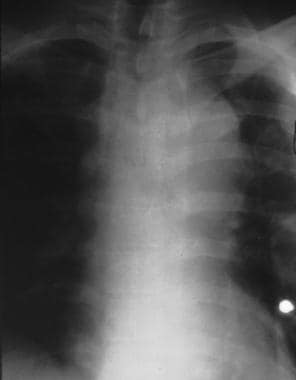
(TAI images are shown below.)
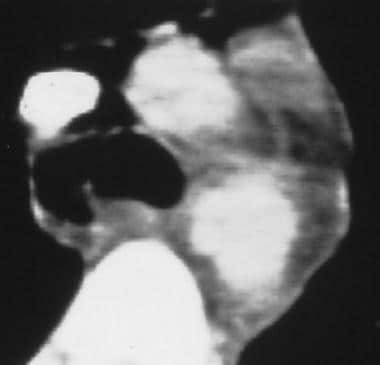
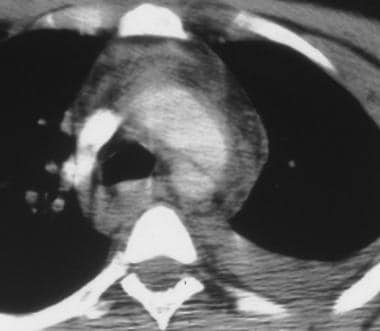 Aorta, trauma. CT scan shows aortic disruption at the aortic isthmus. Increased attenuation is present in the mediastinum; this indicates hematoma and a left pleural effusion. The linear lucency across the aortic lumen may be an artifact. The pseudoaneurysm is not seen on this image.
Aorta, trauma. CT scan shows aortic disruption at the aortic isthmus. Increased attenuation is present in the mediastinum; this indicates hematoma and a left pleural effusion. The linear lucency across the aortic lumen may be an artifact. The pseudoaneurysm is not seen on this image.
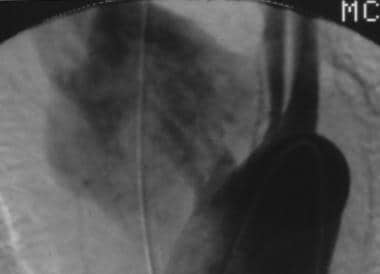
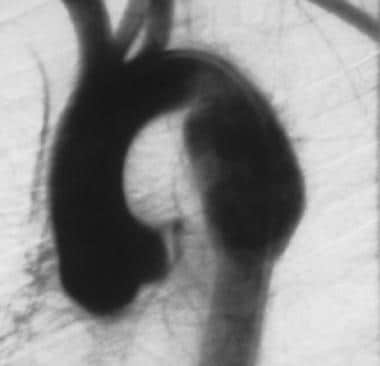
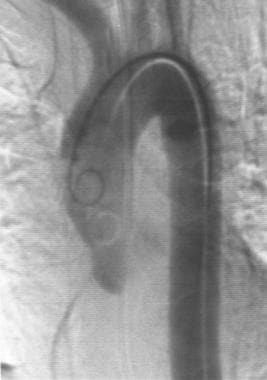
 Aorta, trauma. Left anterior oblique (45°) angiogram shows aortic disruption at the aortic isthmus. An irregular outpouching is present with an intimal flap and an angular transition that represents a contained disruption at the isthmus. This appearance is in contrast to the otherwise normal-appearing vessels.
Aorta, trauma. Left anterior oblique (45°) angiogram shows aortic disruption at the aortic isthmus. An irregular outpouching is present with an intimal flap and an angular transition that represents a contained disruption at the isthmus. This appearance is in contrast to the otherwise normal-appearing vessels.
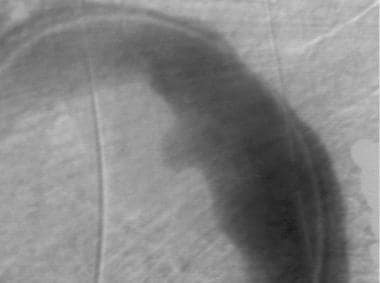
 Aorta, trauma. Left anterior oblique (45°) angiogram shows disruption of the innominate artery. A fairly well-contained pseudoaneurysm originates near the innominate artery.
Aorta, trauma. Left anterior oblique (45°) angiogram shows disruption of the innominate artery. A fairly well-contained pseudoaneurysm originates near the innominate artery.
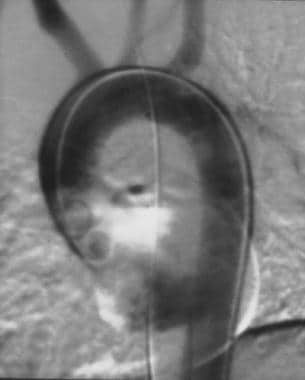
 Aorta, trauma. Posteroanterior angiogram shows disruption of the innominate artery. This delayed image shows continuing expansion of the extravasation of contrast material. The outer margins of the pseudoaneurysm are better delineated on this image than on others.
Aorta, trauma. Posteroanterior angiogram shows disruption of the innominate artery. This delayed image shows continuing expansion of the extravasation of contrast material. The outer margins of the pseudoaneurysm are better delineated on this image than on others.
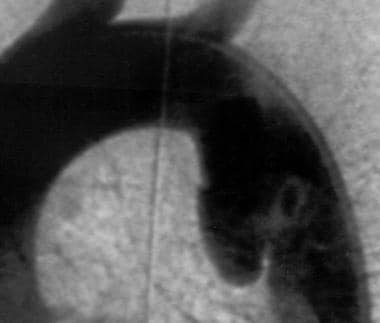
 Aorta, trauma. Left anterior oblique (45°) angiogram shows disruption of the innominate artery. A well-circumscribed narrow-neck pseudoaneurysm is noted along the superior margin of the aortic isthmus. The findings suggest a daughter injury immediately distal to the main outpouching.
Aorta, trauma. Left anterior oblique (45°) angiogram shows disruption of the innominate artery. A well-circumscribed narrow-neck pseudoaneurysm is noted along the superior margin of the aortic isthmus. The findings suggest a daughter injury immediately distal to the main outpouching.
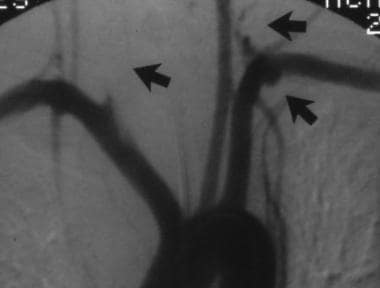 Aorta, trauma. Posteroanterior angiogram shows multiple great-vessel injuries. The image shows a cut-off of the left vertebral artery and a pseudoaneurysm of the left subclavian artery. The right common carotid artery is also occluded. The occlusions are probably due to intimal flap ballooning into the vessel lumen that occludes it.
Aorta, trauma. Posteroanterior angiogram shows multiple great-vessel injuries. The image shows a cut-off of the left vertebral artery and a pseudoaneurysm of the left subclavian artery. The right common carotid artery is also occluded. The occlusions are probably due to intimal flap ballooning into the vessel lumen that occludes it.
 Aorta, trauma. Image shows the contour deformity and the calcified rim of a chronic posttraumatic aortic pseudoaneurysm.
Aorta, trauma. Image shows the contour deformity and the calcified rim of a chronic posttraumatic aortic pseudoaneurysm.
 Aorta, trauma. The image shows the intimal irregularity and intraluminal thrombus of the distal abdominal aorta and the proximal common iliac arteries. This obese patient had a seat-belt injury to the abdominal aorta. Physical examination showed significant ecchymosis of the abdomen. Radiographs showed blurring of the psoas margin with displacement of the ureters.
Aorta, trauma. The image shows the intimal irregularity and intraluminal thrombus of the distal abdominal aorta and the proximal common iliac arteries. This obese patient had a seat-belt injury to the abdominal aorta. Physical examination showed significant ecchymosis of the abdomen. Radiographs showed blurring of the psoas margin with displacement of the ureters.
Blunt traumatic aortic injury is usually located distal to the left subclavian artery, but injuries have also been reported in other locations in the descending thoracic aorta. [6]
Preferred examination
Plain radiography is usually the first test to be performed. The optimal upright posteroanterior (PA) chest evaluation is often deferred for a portable examination with the patient still on the backboard.
Computed tomography (CT) scanning and angiography are the prime imaging modalities in the planning of treatment for blunt trauma. The choice between CT scanning and angiography may depend on institutional preferences, the patient's condition, and the likelihood of other injuries. For example, a patient with hemorrhage from a crushed pelvis would undergo angiography first, whereas a hemodynamically stable patient with a suspected renal or splenic injury would undergo CT scanning first. [7, 8, 9, 10, 11, 12, 3, 13]
Diagnostic imaging should be deferred in patients presenting in hypovolemic shock or cardiac arrest. Advanced (64-slice and greater) spiral CT can produce near-angiographic-quality images, and when available, it should be considered the diagnostic procedure of choice for TAI. Angiography is appropriate in cases where endovascular intervention (eg, stent-graft) is contemplated.
CT angiography has a sensitivity of 98% and a specificity of 100% in the assessment for TAI and is indicated in all cases of high-velocity trauma. Patel et al recommended CT angiography to evaluate the aorta using multiplanar reformatting (aortic injury is most conspicuous in the sagittal-oblique plane [left anterior oblique; 20-90 degrees]) and identify the following [5] :
-
Lower curvature contour of the aortic arch
-
Intimal tear/flap
-
Pseudoaneurysm formation
-
Mediastinal hematoma
-
Periaortic hematoma
-
Presence of hemothorax
-
Additional injuries, including fractures (vertebral, scapula, first/second ribs)
Except in cases involving exsanguinating hemorrhage from a pelvic fracture, angiography has no role in the early treatment of a patient with polytrauma who is in unstable condition. Magnetic resonance imaging (MRI) generally has no role in the acute evaluation of polytrauma. Some centers advocate the early use of transesophageal echocardiography. [14, 15]
Guidelines
According to the American College of Radiology (ACR) Appropriateness Criteria, chest CT with IV contrast, whole-body CT with IV contrast, chest CT angiography with IV contrast, or a radiography trauma series is usually appropriate for the initial imaging of major blunt chest trauma in hemodynamically stable patients. These modalities are considered equivalent to provide the clinical information needed for effective management. [16]
The Eastern Association for the Surgery of Trauma (EAST) published a practice management guideline on evaluation and management of blunt traumatic aortic injury (BTAI), which included the following recommendations [17] :
-
Patients with suspected BTAI - Strong recommendation in favor of computed tomography (CT) of the chest with IV contrast for diagnosis of clinically significant BTAI.
-
Patients diagnosed with BTAI - Strong recommendation in favor of using endovascular repair in patients without contraindications for such repair.
-
Patients diagnosed with BTAI - Suggestion in favor of delayed repair as opposed to immediate repair.
Radiography
After a clinical evaluation, most patients are best evaluated with chest radiography, followed by CT scanning, angiography, or immediate surgery, depending on the specific features of the case and institutional preferences. In the typical emergency department evaluation of a patient with blunt trauma, an initial screening radiograph of the chest and cervical spine is obtained. The patient's clinical condition, the severity and mechanism of the trauma, and the initial radiographic findings are used to determine whether angiography or CT scanning is indicated. [5, 18, 19, 20, 21, 22, 23, 24]
Chest radiographs can be helpful but should not delay cross-sectional imaging if warranted. Chest radiography is better used to assess for life-threatening injuries, such as tension pneumothorax and a large hemothorax requiring immediate drainage. [5]
Initial chest radiography has a significant false-negative rate in patients with TAI. Ekeh et al found that it failed to identify the possibility of blunt thoracic aortic injury in 11% of cases. Consequently, researchers recommend follow-up CT scanning or CT angiography in all patients with suspected TAI. [25, 26, 27]
(Radiographs of aortic trauma are shown below.)
 Aorta, trauma. Chest radiograph shows a chronic isthmus pseudoaneurysm, which is demonstrated as a smooth outpouching near the aortic knob. The calcified rim indicates that this injury is several years old.
Aorta, trauma. Chest radiograph shows a chronic isthmus pseudoaneurysm, which is demonstrated as a smooth outpouching near the aortic knob. The calcified rim indicates that this injury is several years old.
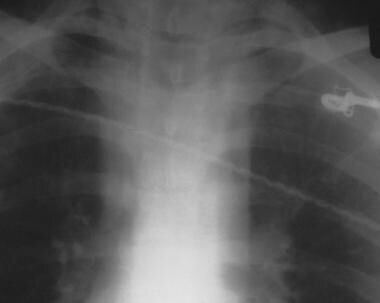 Aorta, trauma. Chest radiograph shows a focal isthmus pseudoaneurysm. The superior mediastinum is distorted, with a loss of the normal aortic knob contour. The right mediastinal edge is blurred as well. Although not measured, the mediastinum is also wide.
Aorta, trauma. Chest radiograph shows a focal isthmus pseudoaneurysm. The superior mediastinum is distorted, with a loss of the normal aortic knob contour. The right mediastinal edge is blurred as well. Although not measured, the mediastinum is also wide.
 Aorta, trauma. Chest radiograph shows an isthmus tear and atherosclerosis in a 79-year-old man. Image shows blurring of the aortic knob with a double shadow. The extensive subcutaneous emphysema probably related to another injury.
Aorta, trauma. Chest radiograph shows an isthmus tear and atherosclerosis in a 79-year-old man. Image shows blurring of the aortic knob with a double shadow. The extensive subcutaneous emphysema probably related to another injury.
Blunt aortic trauma (BAT) has several classic radiographic signs. These signs are more a result of multiple injuries or the radiographic technique used and less a specific sign of BAT. Regarding the well-known sign of mediastinal widening, some trauma radiologists believe that the mediastinal contour is a better indication of BAT than is the transverse diameter.
Diagnoses such as masses, infection, and chronic injury may simulate acute traumatic aortic injury.
Stark et al reviewed the chest radiographic results in 49 cases of aortic rupture and found that a widened mediastinum, partial blurring of the aortic shadow, a left apical cap, and right tracheal deviation were the most common findings. [28] No patient in the study had normal results. Unfortunately, those findings are often nonspecific, and they can be present in patients without significant aortic injury. Therefore, clinical evaluation is essential in determining which patients require further studies.
The incidences of radiographic signs of TAI, as reported by Stark et al, are as follows [28] :
-
Wide mediastinum - 70% (See the images below.)
-
Partial obliteration of the descending aorta - 67%
-
A left apical cap - 65%
-
Downward displacement of the left bronchus - 65%
-
Tracheal deviation to the right - 63%
-
Obscuration of the aortic arch - 55%
-
A right paratracheal stripe thickening - 53%
-
Deviation of the nasogastric (NG) tube to the right - 50%
-
Enlarged abnormal aortic contour - 39%
-
Left hemothorax - 35%
-
A displaced left paraspinal stripe - 35%
-
A displaced right paraspinal stripe - 33%
-
A fracture of the first rib - 16%
 Aorta, trauma. Chest radiograph shows widening of the mediastinal contour and deformity and blurred margins of the superior mediastinum.
Aorta, trauma. Chest radiograph shows widening of the mediastinal contour and deformity and blurred margins of the superior mediastinum.
Radiographic signs of TAI, as reported by Kirsh et al in a study of 43 patients, were as follows: widened mediastinum, 42 patients; abnormal aortic contour, 41 patients; deviation of the trachea to the right, 14 patients; depression of the left mainstem bronchus, 13 patients; left pleural effusion, 15 patients; and negative signs, 1 patient. [29]
The table below shows the poor predictive value of the classic chest radiographic signs of TAI.
Table 1. Frequency of Abnormal Radiographic Signs in Patients with Suspected TAI [30] (Open Table in a new window)
Sign |
Aortic Laceration, % |
Normal Aortographic Findings, % |
Mediastinum > 8 cm |
75.5 |
73.3 |
Indistinct descending aortic arch contour |
75.5 |
94.7 |
Indistinct descending aortic contour |
12.2 |
15.4 |
Trachea displaced to the right |
61.2 |
31.6 |
NG tube or esophagus displaced to the right |
66.7 |
23.1 |
Left mainstem bronchus displaced inferiorly |
53.1 |
26.3 |
Pleural apical cap |
36.7 |
42.1 |
Fracture of rib 1 or 2 |
17.0 |
30.0 |
Computed Tomography
Traumatic aortic injury (TAI) may be diagnosed from CT scans on the basis of direct or indirect signs. Direct signs (eg, aortic intimal flap, contour abnormality) are more accurate than indirect signs (eg, mediastinal, periaortic hematoma). CT scanning is an excellent screening modality for patients who are not undergoing aortography. It is particularly convenient in patients with polytrauma who are undergoing other CT scan studies at the same time. Acquisition parameters and protocols should be developed locally, based on equipment, physician preference, and patient condition. If CT angiographic reconstruction is used, the axial source images should be reviewed. [7, 8, 11, 3, 13]
(CT scans of aortic trauma are shown below.)
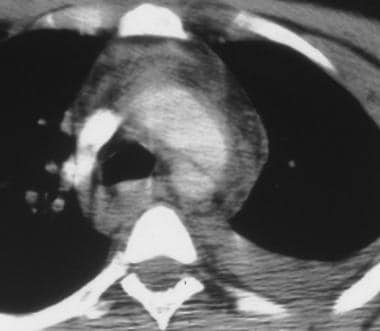 Aorta, trauma. CT scan shows aortic disruption at the aortic isthmus. Increased attenuation is present in the mediastinum; this indicates hematoma and a left pleural effusion. The linear lucency across the aortic lumen may be an artifact. The pseudoaneurysm is not seen on this image.
Aorta, trauma. CT scan shows aortic disruption at the aortic isthmus. Increased attenuation is present in the mediastinum; this indicates hematoma and a left pleural effusion. The linear lucency across the aortic lumen may be an artifact. The pseudoaneurysm is not seen on this image.
 Aorta, trauma. CT scan shows a focal isthmus pseudoaneurysm. The image shows increased attenuation of the mediastinum, which is consistent with mediastinal hematoma. The descending aortic contour is bilobed, consistent with pseudoaneurysm formation.
Aorta, trauma. CT scan shows a focal isthmus pseudoaneurysm. The image shows increased attenuation of the mediastinum, which is consistent with mediastinal hematoma. The descending aortic contour is bilobed, consistent with pseudoaneurysm formation.
The advantages of CT scanning are that it is quick, noninvasive, useful in evaluating multiple traumas at the same time, and capable of providing a larger field of interest, particularly with fast spiral technology. [31, 32, 33] The historic tradeoff between CT scanning and angiography was image resolution versus cross-sectional imaging. The submillimeter resolution available with angiography (cut-film and then digital subtraction angiography [DSA]) was invaluable for delineating the sometimes subtle findings of traumatic aortic disruption. CT scanning times were long, and sections were thick. Moreover, the intravascular density of contrast material on CT scans was far less than that which is currently achievable. False-negative results could occur with subtle injuries. False-positive CT scan findings were possible with mediastinal hemorrhage from venous bleeding and irregularities of the vessel wall due to atherosclerosis.
Multidetector spiral technology has allowed CT scanning to catch up to angiography in terms of image quality; 64- or 256-slice scanners can image with submillimeter-section thicknesses and a 512 × 512 image matrix rivaling DSA 1024 examinations. CT scanning is ideal for evaluating the nonarterial injuries in patients with polytrauma, such as patients with brain, spinal, pelvic, spleen, liver, and/or kidney injuries. A single intravenous administration of contrast material can be used for a combined vascular and nonvascular evaluation. Multidetector-row units may allow CT scanning to eventually become the new criterion standard. [24, 34, 35, 36]
Technological improvements, however, are a double-edged sword. With decreasing section thickness comes a commensurate increase in the number of images to be interpreted. Examinations involving 600-800 individual sections are possible. High-speed diagnostic workstations can help manage the data load. With these workstations, reviewers can rapidly scroll through high-resolution datasets and combine the data into fewer, thicker sections.
Another data-management tool brings diagnosis full circle to the angiographic interpretation of BAT images. Cross-sectional imaging may be processed with 3-dimensional (3D) and 2-dimensional (2D) surface reconstruction techniques. These reconstruction techniques produce images that simulate anatomic dissections and angiograms. The images allow the clinician to obtain an examination overview and to focus on particular areas of pathology or surgical interest. As technology improves, reconstructed images will eventually supplant source images in routine image interpretation.
The imaging endpoints of reconstructed CT scans and conventional angiograms are essentially similar. Similar interpretation approaches are likely to apply. Angiographic signs and interpretation skills should have significant overlap with the evaluation of CT angiograms.
The disadvantages of CT scanning are as follows: (1) CT scanning may be limited by partial-volume effects (eg, those due to small disruption or subtle intimal injury), (2) cardiac and respiratory motion (eg, artifact in the region of the aortic root) can affect the image quality, and (3) CT scanning can expose the patient to contrast material, particularly if angiography and/or embolization are required. These disadvantages are minimized with modern scanner technology.
Degree of confidence
Studies have shown that CT scanning is sensitive for TAI (83-100%) and that it has a negative predictive value (NPV) of 99-100%. Its specificity of 54-99.8% and its related positive predictive value (PPV) of 9-89% are generally lower than those of angiography.
Mirvis et al explained the reason for the lower specificity of CT scanning. The authors stratified the sensitivity and specificity results based on direct and indirect signs. Although direct signs were 99% specific, they reported that the specificity of indirect signs was only 87%. [37]
Further study is needed before the field of CT scanning in traumatology is considered mature. Most of the studies that show a 100% NPV for CT scanning is limited to clinical follow-up. Data about follow-up CT or angiography in patients with negative initial CT scan findings are limited.
However, in a study of blunt trauma patients that included 72 patients who underwent CT angiography (CTA) followed by catheter angiography, Sammer et al found that when CTA findings are indeterminate (ie, showing mediastinal hematoma without direct evidence of aortic or intrathoracic great vessel injury), conventional angiography is unlikely to show an aortic or intrathoracic great vessel injury and may be unnecessary. [38] In this study, isolated mediastinal hematoma on CTA had an NPV of 100% for aortic or intrathoracic great vessel injury.
In a study of patients with acute traumatic aortic injury (TAI), Steenburg and Ravenel found that catheter angiograms after contrast-enhanced 64-channel multidetector CT (64-MDCT) scans were of limited value. Of the 10 such cases in their study, direct signs on 64-MDCT scans were confirmed in 3 cases; indirect signs were found to be normal findings in 5 cases; and equivocal findings remained equivocal in 2 cases. No patient with equivocal or indirect findings on 64-MDCT needed surgical repair. These researchers concluded that when 64-MDCT scans show direct signs of TAI, standard angiography is unnecessary. [39]
A number of investigators recommend CT scanning as the screening examination of choice for TAI as well as for other injuries (eg, pulmonary laceration, pneumothorax, tracheobronchial injury, spinal injury). Unless the CT scan results are diagnostic, confirmatory angiography is generally required.
Pate et al reported that CT scanning led to a 50% reduction in the use of angiography; this is a benefit in institutions with limited access to angiography. [40]
Because of the nearly 100% sensitivity and specificity of helical CT scanning, this modality has largely replaced aortography in the diagnosis of TAI in adults and children.
Atelectasis, the thymus, or the pericardial recess can mimic mediastinal hematoma. Ductus diverticulum or other variants may be confused with traumatic aortic injury (TAI). Mediastinal hematoma may be due to venous or arterial injury. Subtle ruptures, particularly intimal injuries, may not be clearly delineated. Nevertheless, authors of published reports speak highly of CT evaluation.
Ultrasonography
Transesophageal echocardiography (TEE) for the diagnosis of traumatic aortic injury has its proponents, who support the modality mostly because of its portability and rapid availability in a trauma center setting. TEE has significant proponents in the pediatric trauma literature.
Intravascular ultrasonography is very helpful in identifying traumatic intimal flaps when CTA and aortographic findings are inconclusive in the diagnosis of aortic injuries.
Limitations of the modality include blind spots where the aorta is suboptimally imaged with ultrasonography. Like angiography, TEE is operator and reader dependent and must be performed by well-trained personnel.
Angiography
Thoracic aortography may be performed with a standard 100-cm-long 5F pigtail catheter, although a 110-cm-long 6F pigtail is preferred. The longer length is helpful for reaching the aortic root in tall patients.
With the 6F catheter, the 27-mL/s contrast-agent injection rate typical of 100-cm-long 5F catheters can be exceeded. The 6F pigtail may be more rigid than 5F catheters. Predilation of the tract with a 5F or 6F dilator or a 6F sheath is recommended.
The imaging rate of thoracic aortography is 4-6 frames/sec on deep inspiration. [41]
(Angiograms of aortic trauma in the region of the isthmus are shown below.)
 Aorta, trauma. Left anterior oblique (45°) angiogram shows aortic disruption at the aortic isthmus. An irregular outpouching is present with an intimal flap and an angular transition that represents a contained disruption at the isthmus. This appearance is in contrast to the otherwise normal-appearing vessels.
Aorta, trauma. Left anterior oblique (45°) angiogram shows aortic disruption at the aortic isthmus. An irregular outpouching is present with an intimal flap and an angular transition that represents a contained disruption at the isthmus. This appearance is in contrast to the otherwise normal-appearing vessels.
 Aorta, trauma. Image shows a chronic isthmus pseudoaneurysm, which is indistinguishable from the acute variety. The calcium seen on plain radiographs is not readily seen on digital subtraction angiograms (DSAs).
Aorta, trauma. Image shows a chronic isthmus pseudoaneurysm, which is indistinguishable from the acute variety. The calcium seen on plain radiographs is not readily seen on digital subtraction angiograms (DSAs).
 Aorta, trauma. Posteroanterior angiogram shows a focal isthmus pseudoaneurysm. A fairly sharply demarcated, rounded, doubly dense region is seen superimposed on the isthmus area. Its differentiation from a normal ductus may be difficult.
Aorta, trauma. Posteroanterior angiogram shows a focal isthmus pseudoaneurysm. A fairly sharply demarcated, rounded, doubly dense region is seen superimposed on the isthmus area. Its differentiation from a normal ductus may be difficult.
 Aorta, trauma. Left anterior oblique (45°) angiogram shows a focal isthmus pseudoaneurysm. Image shows delayed washout from the slightly irregular isthmus bulge that supports the diagnosis of pseudoaneurysm. The remainder of the aorta is smooth in this 19-year-old male patient.
Aorta, trauma. Left anterior oblique (45°) angiogram shows a focal isthmus pseudoaneurysm. Image shows delayed washout from the slightly irregular isthmus bulge that supports the diagnosis of pseudoaneurysm. The remainder of the aorta is smooth in this 19-year-old male patient.
 Aorta, trauma. Posteroanterior (PA) angiogram shows a subtle intimal flap. Only a hint of the intimal flap at the anteromedial isthmus is depicted in this 31-year-old man. The angiographic findings are otherwise normal.
Aorta, trauma. Posteroanterior (PA) angiogram shows a subtle intimal flap. Only a hint of the intimal flap at the anteromedial isthmus is depicted in this 31-year-old man. The angiographic findings are otherwise normal.
 Aorta, trauma. Left anterior oblique (30°) angiogram shows a subtle intimal flap. Image demonstrates a focal anteromedial isthmus bulge with the intimal flap shown to better advantage.
Aorta, trauma. Left anterior oblique (30°) angiogram shows a subtle intimal flap. Image demonstrates a focal anteromedial isthmus bulge with the intimal flap shown to better advantage.
 Aorta, trauma. Posteroanterior angiogram shows a subtle isthmus tear in a 21-year-old man. On this view, the anteromedial isthmus abnormality is subtly demonstrated as a round, superimposed density in this otherwise unremarkable study.
Aorta, trauma. Posteroanterior angiogram shows a subtle isthmus tear in a 21-year-old man. On this view, the anteromedial isthmus abnormality is subtly demonstrated as a round, superimposed density in this otherwise unremarkable study.
 Aorta, trauma. Posteroanterior (PA) angiogram shows a subtle circumferential isthmus tear in a 72-year-old man. Image demonstrates the mildly irregular lateral surface of the aortic isthmus. This abnormality could easily be confused with atherosclerosis.
Aorta, trauma. Posteroanterior (PA) angiogram shows a subtle circumferential isthmus tear in a 72-year-old man. Image demonstrates the mildly irregular lateral surface of the aortic isthmus. This abnormality could easily be confused with atherosclerosis.
 Aorta, trauma. Posteroanterior (PA) angiogram shows an anteromedial isthmus rupture in a 19-year-old man. Image shows an anteromedial bulge with a slightly irregular contour and a suggestion of an acute-angle transition with the aortic wall. This appearance might be confused with that of a ductus diverticulum.
Aorta, trauma. Posteroanterior (PA) angiogram shows an anteromedial isthmus rupture in a 19-year-old man. Image shows an anteromedial bulge with a slightly irregular contour and a suggestion of an acute-angle transition with the aortic wall. This appearance might be confused with that of a ductus diverticulum.
 Aorta, trauma. Angiogram shows a circumferential isthmus rupture. The surface irregularity, contour abnormality, and acute angulation of the transition make this diagnosis easy.
Aorta, trauma. Angiogram shows a circumferential isthmus rupture. The surface irregularity, contour abnormality, and acute angulation of the transition make this diagnosis easy.
 Aorta, trauma. Left anterior oblique angiogram shows an isthmus tear and atherosclerosis. Although the appearance of the surrounding and underlying atherosclerosis confuses the diagnosis, a definite focal bulge at the anteromedial isthmus is noted. This was proven to be a traumatic aortic injury (TAI).
Aorta, trauma. Left anterior oblique angiogram shows an isthmus tear and atherosclerosis. Although the appearance of the surrounding and underlying atherosclerosis confuses the diagnosis, a definite focal bulge at the anteromedial isthmus is noted. This was proven to be a traumatic aortic injury (TAI).
 Aorta, trauma. Left anterior oblique (60°) angiogram shows atherosclerosis without an aortic injury. No focal variation in the atherosclerotic pattern is present to suggest injury.
Aorta, trauma. Left anterior oblique (60°) angiogram shows atherosclerosis without an aortic injury. No focal variation in the atherosclerotic pattern is present to suggest injury.
 Aorta, trauma. Angiogram shows a chronic circumferential isthmus rupture. The appearance should not be confused with that of the normal fusiform dilation in the previous image. Note the acute angles of the transition and the irregular margins. This patient was 9 years old and was involved in a motor vehicle accident.
Aorta, trauma. Angiogram shows a chronic circumferential isthmus rupture. The appearance should not be confused with that of the normal fusiform dilation in the previous image. Note the acute angles of the transition and the irregular margins. This patient was 9 years old and was involved in a motor vehicle accident.
 Aorta, trauma. Lateral digital subtraction angiogram shows a subtle isthmus pseudoaneurysm. This image better demonstrates the irregular contour and the right-angle transition of the pseudoaneurysm.
Aorta, trauma. Lateral digital subtraction angiogram shows a subtle isthmus pseudoaneurysm. This image better demonstrates the irregular contour and the right-angle transition of the pseudoaneurysm.
 Aorta, trauma. Lateral screen-film angiogram shows a subtle isthmus pseudoaneurysm. Conventional subtraction image demonstrates the irregular contour of the isthmus rupture. The image also suggests a linear defect of the intimal flap. Surgical exploration confirmed subtle aortic injury. CT scan of the aortic arch (not shown) showed no abnormality in the region of the traumatic pseudoaneurysm that was demonstrated on the angiogram.
Aorta, trauma. Lateral screen-film angiogram shows a subtle isthmus pseudoaneurysm. Conventional subtraction image demonstrates the irregular contour of the isthmus rupture. The image also suggests a linear defect of the intimal flap. Surgical exploration confirmed subtle aortic injury. CT scan of the aortic arch (not shown) showed no abnormality in the region of the traumatic pseudoaneurysm that was demonstrated on the angiogram.
Although most traumatic aortic injuries occur in the region of the isthmus, the entire thoracic aorta should be evaluated. To exclude aortic regurgitation and other aortic root injury, the catheter is first placed above the sinuses of Valsalva. A test injection is used to verify that the catheter tip does not interfere with the aortic root, to avoid spurious aortic regurgitation (see the image below). The contrast-agent injection rate is 20 to 30 mL/s for 50 mL, depending on the patient's cardiac output. Patients with blunt aortic trauma (BAT) are typically young and present in a state of high cardiac output.
 Aorta, trauma. Angiogram shows a spurious aortic regurgitation. The pigtail catheter is placed too close to the aortic valves (sinuses of Valsalva) and interferes with normal valvular function and regurgitation. Repeat angiogram obtained after the catheter was repositioned showed normal findings. The position of the catheter should be verified with a vigorous test injection.
Aorta, trauma. Angiogram shows a spurious aortic regurgitation. The pigtail catheter is placed too close to the aortic valves (sinuses of Valsalva) and interferes with normal valvular function and regurgitation. Repeat angiogram obtained after the catheter was repositioned showed normal findings. The position of the catheter should be verified with a vigorous test injection.
The injection and imaging rate may be adjusted on the basis of the test injection results. For intubated patients, mechanical ventilation may be suspended during each angiographic run. Once the aortic root and the ascending aorta are cleared, the catheter may then be withdrawn to the upper ascending aorta to concentrate on the isthmus and distal aorta. The side holes of the catheter should be positioned just proximal to the area of interest for maximum opacification.
Aortographic signs of aortic rupture may be subtle. A minimum of 2 angiographic projections is required to exclude traumatic aortic injury (TAI). Typical projections are a 45° left anterior oblique (LAO) view followed by a steep LAO or lateral view (see the images below). When an isthmus abnormality is suspected, obtain a lateral or steep LAO view to differentiate between the contour abnormality of a pseudoaneurysm and a normal ductus. Other projections are obtained depending on clinical suspicion and the preliminary angiographic findings. In one case from the author's experience, a rupture was better seen on the PA image than on the shallow oblique image (no steep oblique or lateral image had been obtained).
 Aorta, trauma. Left anterior oblique (45°) angiogram shows a subtle isthmus tear. This digital subtraction angiogram clearly demonstrates the focal bulge of a pseudoaneurysm, with a linear defect of the intimal flap shown superiorly.
Aorta, trauma. Left anterior oblique (45°) angiogram shows a subtle isthmus tear. This digital subtraction angiogram clearly demonstrates the focal bulge of a pseudoaneurysm, with a linear defect of the intimal flap shown superiorly.
 Aorta, trauma. Left anterior oblique (45°) digital subtraction angiogram shows a subtle circumferential isthmus tear. The findings confirm the irregularity, and the image shows a focal bulge with a sharply angled superior transition.
Aorta, trauma. Left anterior oblique (45°) digital subtraction angiogram shows a subtle circumferential isthmus tear. The findings confirm the irregularity, and the image shows a focal bulge with a sharply angled superior transition.
 Aorta, trauma. Left anterior oblique (45°) digital subtraction angiogram shows an anteromedial isthmus rupture. Image clearly demonstrates the linear defect of an intimal flap, which confirms the diagnosis of an aortic rupture.
Aorta, trauma. Left anterior oblique (45°) digital subtraction angiogram shows an anteromedial isthmus rupture. Image clearly demonstrates the linear defect of an intimal flap, which confirms the diagnosis of an aortic rupture.
 Aorta, trauma. Left anterior oblique (45°) angiogram shows a circumferential isthmus rupture. Irregularity and acute angulation are noted in this acute traumatic aortic injury (TAI).
Aorta, trauma. Left anterior oblique (45°) angiogram shows a circumferential isthmus rupture. Irregularity and acute angulation are noted in this acute traumatic aortic injury (TAI).
 Aorta, trauma. Left anterior oblique (45°) angiogram shows a circumferential isthmus rupture. The contour of the proximal margin of the pseudoaneurysm is shown in relief against the adjacent aorta.
Aorta, trauma. Left anterior oblique (45°) angiogram shows a circumferential isthmus rupture. The contour of the proximal margin of the pseudoaneurysm is shown in relief against the adjacent aorta.
 Aorta, trauma. Left anterior oblique (45°) angiogram shows a normal aorta with a fusiform isthmus and atherosclerosis. No abnormality is superimposed over the normal variant fusiform appearance of the isthmus and the typical appearance of atherosclerosis.
Aorta, trauma. Left anterior oblique (45°) angiogram shows a normal aorta with a fusiform isthmus and atherosclerosis. No abnormality is superimposed over the normal variant fusiform appearance of the isthmus and the typical appearance of atherosclerosis.
 Aorta, trauma. Left anterior oblique (45°) digital subtraction angiogram shows a subtle isthmus pseudoaneurysm. The image shows a slightly asymmetrical anteromedial bulge that might represent a small ductus diverticulum.
Aorta, trauma. Left anterior oblique (45°) digital subtraction angiogram shows a subtle isthmus pseudoaneurysm. The image shows a slightly asymmetrical anteromedial bulge that might represent a small ductus diverticulum.
Biplane imaging or rotational angiography can reduce the examination time and the contrast agent load. A biplane combination of 45° right anterior oblique (RAO) and/or LAO views may be used. The imaging frame rate, the source-to–image intensifier distance (SID), and the projection may be altered to accommodate tube loading, kilovolt-peak issues, or cardiac output. A typical frame rate is 4-6 per second. DSA magnification may be helpful in equivocal cases.
Tube-loading limits may become significant for steep oblique or lateral magnified studies. Rotational angiography typically increases tube loading. Whenever tube loading becomes an issue, the traditional steps may be taken—that is, a reduction in the frame rate and the duration of the examination, in the SID, in the magnification, or in the dose (increased DSA quantum mottle).
Degree of confidence
Angiography is the traditional modality for evaluating patients with suspected acute TAI. Approximately 10-20% of patients with blunt trauma who are referred for angiography have positive angiographic findings. In BAT, angiography is best used as a confirmatory tool for patients with positive CT scan findings or as a primary diagnostic tool in hemodynamically stable patients in whom the clinical suspicion for TAI is high.
Gavant reported that angiography is 94% sensitive and 96% specific, with an NPV of 99% and a PPV of 81%. [42] Fabian et al reported that angiography had a sensitivity of 100%, a specificity of 97%, an NPV of 97%, and a PPV of 97%. [43]
False positives/negatives
A high index of suspicion is required when a patient is evaluated for TAI. Mortality associated with a missed diagnosis (false-negative angiographic finding) is high. Equivocal cases should undergo close clinical and imaging follow-up or exploratory surgery. Surgery is a relatively benign procedure when the risk of morbidity and mortality associated with a missed TAI is considered. As the quality of CT and other noninvasive imaging modalities improve, the surgical exploration rate can be expected to decrease.
False diagnoses can be minimized by paying meticulous attention to the imaging technique and by following up any equivocal findings. False-negative angiographic results may occur when the injury is subtle, when it is not seen in profile (out of plane), or when the injured area is not delineated by the contrast agent column or when it is out of the field of view.
False-positive angiographic results (examples of which appear below) may occur as a result of inadequate angiographic technique (catheter position, injection rate, exposure and position), motion or inflow artifacts, comorbidities (eg, atherosclerosis), the presence of nontraumatic entities (eg, infection), and normal variants in the anatomy.
Common variants at the isthmus are a smooth, fusiform, circumferential widening at the isthmus; a ductus diverticulum; and an asymmetrical ductus with bronchointercostal artery. No other signs of TAI should be present if a normal variant is to be safely diagnosed.
 Aorta, trauma. Left anterior oblique angiogram shows a normal fusiform aortic isthmus. Angiogram shows smooth, fusiform widening of the isthmus with a smooth transition at an obtuse angle with the descending aorta. No persistence of contrast opacification is shown. This 31-year-old patient was referred for surgery, and a normal aorta was found. The angiographic findings were false-positive. In the author's experience, subsequent patients with similar findings have not been referred for thoracotomy, and they have not developed signs or symptoms of aortic rupture.
Aorta, trauma. Left anterior oblique angiogram shows a normal fusiform aortic isthmus. Angiogram shows smooth, fusiform widening of the isthmus with a smooth transition at an obtuse angle with the descending aorta. No persistence of contrast opacification is shown. This 31-year-old patient was referred for surgery, and a normal aorta was found. The angiographic findings were false-positive. In the author's experience, subsequent patients with similar findings have not been referred for thoracotomy, and they have not developed signs or symptoms of aortic rupture.
 Aorta, trauma. Left anterior oblique (20°) angiogram shows an acute widening in the anteromedial isthmus region, with linear enhancement projecting superomedially. This 40-year-old man underwent surgical exploration, with negative results. The finding was retrospectively identified as a normal bronchointercostal artery.
Aorta, trauma. Left anterior oblique (20°) angiogram shows an acute widening in the anteromedial isthmus region, with linear enhancement projecting superomedially. This 40-year-old man underwent surgical exploration, with negative results. The finding was retrospectively identified as a normal bronchointercostal artery.
-
Aorta, trauma. CT scan shows aortic disruption at the aortic isthmus. Increased attenuation is present in the mediastinum; this indicates hematoma and a left pleural effusion. The linear lucency across the aortic lumen may be an artifact. The pseudoaneurysm is not seen on this image.
-
Aorta, trauma. Left anterior oblique (45°) angiogram shows aortic disruption at the aortic isthmus. An irregular outpouching is present with an intimal flap and an angular transition that represents a contained disruption at the isthmus. This appearance is in contrast to the otherwise normal-appearing vessels.
-
Aorta, trauma. Left anterior oblique (45°) angiogram shows disruption of the innominate artery. A fairly well-contained pseudoaneurysm originates near the innominate artery.
-
Aorta, trauma. Chest radiograph shows widening of the mediastinal contour and deformity and blurred margins of the superior mediastinum.
-
Aorta, trauma. Posteroanterior angiogram shows disruption of the innominate artery. This early image shows a poorly circumscribed pseudoaneurysm or extravasation.
-
Aorta, trauma. Posteroanterior angiogram shows disruption of the innominate artery. This delayed image shows continuing expansion of the extravasation of contrast material. The outer margins of the pseudoaneurysm are better delineated on this image than on others.
-
Aorta, trauma. Left anterior oblique (45°) angiogram shows disruption of the innominate artery. A well-circumscribed narrow-neck pseudoaneurysm is noted along the superior margin of the aortic isthmus. The findings suggest a daughter injury immediately distal to the main outpouching.
-
Aorta, trauma. Posteroanterior angiogram shows multiple great-vessel injuries. The image shows a cut-off of the left vertebral artery and a pseudoaneurysm of the left subclavian artery. The right common carotid artery is also occluded. The occlusions are probably due to intimal flap ballooning into the vessel lumen that occludes it.
-
Aorta, trauma. Left anterior oblique angiogram (LAO) shows the typical appearance of the normal ductus diverticulum. The smooth walls and transition would be better delineated on a steep LAO or lateral view (not shown).
-
Aorta, trauma. Chest radiograph shows a chronic isthmus pseudoaneurysm, which is demonstrated as a smooth outpouching near the aortic knob. The calcified rim indicates that this injury is several years old.
-
Aorta, trauma. Image shows a chronic isthmus pseudoaneurysm, which is indistinguishable from the acute variety. The calcium seen on plain radiographs is not readily seen on digital subtraction angiograms (DSAs).
-
Aorta, trauma. Chest radiograph shows a focal isthmus pseudoaneurysm. The superior mediastinum is distorted, with a loss of the normal aortic knob contour. The right mediastinal edge is blurred as well. Although not measured, the mediastinum is also wide.
-
Aorta, trauma. CT scan shows a focal isthmus pseudoaneurysm. The image shows increased attenuation of the mediastinum, which is consistent with mediastinal hematoma. The descending aortic contour is bilobed, consistent with pseudoaneurysm formation.
-
Aorta, trauma. Posteroanterior angiogram shows a focal isthmus pseudoaneurysm. A fairly sharply demarcated, rounded, doubly dense region is seen superimposed on the isthmus area. Its differentiation from a normal ductus may be difficult.
-
Aorta, trauma. Left anterior oblique (45°) angiogram shows a focal isthmus pseudoaneurysm. Image shows delayed washout from the slightly irregular isthmus bulge that supports the diagnosis of pseudoaneurysm. The remainder of the aorta is smooth in this 19-year-old male patient.
-
Aorta, trauma. Chest radiograph shows spontaneous rupture of the isthmus, a mycotic aneurysm secondary to Salmonella pneumonitis infection. The widening and distortion of the superior mediastinum is indistinguishable from a traumatic pseudoaneurysm. This patient had no history of significant trauma and presented with chest pain. At surgery, a necrotic node was found, and Salmonella organisms were cultured. A faint bronchogram was noted retrospectively.
-
Aorta, trauma. CT scan shows spontaneous rupture of the isthmus, a mycotic aneurysm secondary to Salmonella pneumonitis infection. Increased attenuation in the mediastinum is indistinguishable from a hematoma. The calcified outpouching of the aorta suggests a more chronic condition.
-
Aorta, trauma. Left anterior oblique (40°) angiogram shows spontaneous rupture of the isthmus, a mycotic aneurysm secondary to Salmonella pneumonitis infection. An isthmus outpouching has reduced contrast enhancement and a slightly irregular contour and margins in comparison with the surrounding aorta. This appearance is indistinguishable from that of a traumatic pseudoaneurysm.
-
Aorta, trauma. Angiogram shows a spurious aortic regurgitation. The pigtail catheter is placed too close to the aortic valves (sinuses of Valsalva) and interferes with normal valvular function and regurgitation. Repeat angiogram obtained after the catheter was repositioned showed normal findings. The position of the catheter should be verified with a vigorous test injection.
-
Aorta, trauma. Left anterior oblique (LAO) (30°) angiogram shows a tear on the undersurface of the aortic arch. This case is unusual in that the oblique view fails to demonstrate all of the patient's injuries. This moderate LAO view demonstrates only the atherosclerotic and hypertensive changes.
-
Aorta, trauma. Left anterior oblique (4°) angiogram shows a tear on the undersurface of the aortic arch. This nearly posteroanterior (PA) view demonstrates a small but definite irregular and hypodense pseudoaneurysm extending from the undersurface of the aortic arch. This case illustrates the need for multiple angiographic projections before the findings can be declared normal.
-
Aorta, trauma. Angiogram shows a focal isthmus traumatic pseudoaneurysm. This example demonstrates an anteromedial bulge, intimal flap, acute-angle transition, irregular contour, and contrast-material hang up in this 45-year-old female patient.
-
Aorta, trauma. Posteroanterior (PA) angiogram shows a subtle intimal flap. Only a hint of the intimal flap at the anteromedial isthmus is depicted in this 31-year-old man. The angiographic findings are otherwise normal.
-
Aorta, trauma. Left anterior oblique (30°) angiogram shows a subtle intimal flap. Image demonstrates a focal anteromedial isthmus bulge with the intimal flap shown to better advantage.
-
Aorta, trauma. Posteroanterior angiogram shows a subtle isthmus tear in a 21-year-old man. On this view, the anteromedial isthmus abnormality is subtly demonstrated as a round, superimposed density in this otherwise unremarkable study.
-
Aorta, trauma. Left anterior oblique (45°) angiogram shows a subtle isthmus tear. This digital subtraction angiogram clearly demonstrates the focal bulge of a pseudoaneurysm, with a linear defect of the intimal flap shown superiorly.
-
Aorta, trauma. Posteroanterior (PA) angiogram shows a subtle circumferential isthmus tear in a 72-year-old man. Image demonstrates the mildly irregular lateral surface of the aortic isthmus. This abnormality could easily be confused with atherosclerosis.
-
Aorta, trauma. Left anterior oblique (45°) digital subtraction angiogram shows a subtle circumferential isthmus tear. The findings confirm the irregularity, and the image shows a focal bulge with a sharply angled superior transition.
-
Aorta, trauma. Posteroanterior (PA) angiogram shows an anteromedial isthmus rupture in a 19-year-old man. Image shows an anteromedial bulge with a slightly irregular contour and a suggestion of an acute-angle transition with the aortic wall. This appearance might be confused with that of a ductus diverticulum.
-
Aorta, trauma. Left anterior oblique (45°) digital subtraction angiogram shows an anteromedial isthmus rupture. Image clearly demonstrates the linear defect of an intimal flap, which confirms the diagnosis of an aortic rupture.
-
Aorta, trauma. Left anterior oblique (45°) angiogram shows a circumferential isthmus rupture. Irregularity and acute angulation are noted in this acute traumatic aortic injury (TAI).
-
Aorta, trauma. Chest radiograph shows a circumferential isthmus rupture. The aortic knob is not depicted, and the mediastinum is wide and deformed.
-
Aorta, trauma. Left anterior oblique (45°) angiogram shows a circumferential isthmus rupture. The contour of the proximal margin of the pseudoaneurysm is shown in relief against the adjacent aorta.
-
Aorta, trauma. Angiogram shows a circumferential isthmus rupture. The surface irregularity, contour abnormality, and acute angulation of the transition make this diagnosis easy.
-
Aorta, trauma. Chest radiograph shows an isthmus tear and atherosclerosis in a 79-year-old man. Image shows blurring of the aortic knob with a double shadow. The extensive subcutaneous emphysema probably related to another injury.
-
Aorta, trauma. Left anterior oblique angiogram shows an isthmus tear and atherosclerosis. Although the appearance of the surrounding and underlying atherosclerosis confuses the diagnosis, a definite focal bulge at the anteromedial isthmus is noted. This was proven to be a traumatic aortic injury (TAI).
-
Aorta, trauma. Left anterior oblique (30°) angiogram shows atherosclerosis without an aortic injury. No focal variation in the atherosclerotic pattern is present to suggest injury.
-
Aorta, trauma. Left anterior oblique (60°) angiogram shows atherosclerosis without an aortic injury. No focal variation in the atherosclerotic pattern is present to suggest injury.
-
Aorta, trauma. Left anterior oblique angiogram shows a normal fusiform aortic isthmus. Angiogram shows smooth, fusiform widening of the isthmus with a smooth transition at an obtuse angle with the descending aorta. No persistence of contrast opacification is shown. This 31-year-old patient was referred for surgery, and a normal aorta was found. The angiographic findings were false-positive. In the author's experience, subsequent patients with similar findings have not been referred for thoracotomy, and they have not developed signs or symptoms of aortic rupture.
-
Aorta, trauma. Left anterior oblique (45°) angiogram shows a normal aorta with a fusiform isthmus and atherosclerosis. No abnormality is superimposed over the normal variant fusiform appearance of the isthmus and the typical appearance of atherosclerosis.
-
Aorta, trauma. Angiogram shows a chronic circumferential isthmus rupture. The appearance should not be confused with that of the normal fusiform dilation in the previous image. Note the acute angles of the transition and the irregular margins. This patient was 9 years old and was involved in a motor vehicle accident.
-
Aorta, trauma. Left anterior oblique (20°) angiogram shows an acute widening in the anteromedial isthmus region, with linear enhancement projecting superomedially. This 40-year-old man underwent surgical exploration, with negative results. The finding was retrospectively identified as a normal bronchointercostal artery.
-
Aorta, trauma. Left anterior oblique (45°) angiogram shows a normal bronchointercostal artery with a ductus diverticulum. The initial image in this young female patient who was injured in a motor vehicle accident shows a possible contour abnormality in the region of the isthmus.
-
Aorta, trauma. Left anterior oblique (70°) angiogram shows a normal bronchointercostal artery with a ductus diverticulum. The anteromedial isthmus outpouching is asymmetrical, with a questionable distal irregularity. The differential diagnosis includes ductus diverticulum and traumatic aortic injury (TAI).
-
Aorta, trauma. Lateral digital subtraction angiogram shows a normal bronchointercostal artery with a ductus diverticulum. The anteromedial isthmus outpouching is asymmetrical, and a right-angle transition is depicted proximally. The margins are smooth, and no hang up is shown. Because of the severity of the patient's other injuries, surgical exploration was recommended. During surgery, a normal isthmus region was found.
-
Aorta, trauma. Anteroposterior digital subtraction angiogram shows a subtle isthmus pseudoaneurysm. The image demonstrates no abnormality.
-
Aorta, trauma. Left anterior oblique (45°) digital subtraction angiogram shows a subtle isthmus pseudoaneurysm. The image shows a slightly asymmetrical anteromedial bulge that might represent a small ductus diverticulum.
-
Aorta, trauma. Lateral digital subtraction angiogram shows a subtle isthmus pseudoaneurysm. This image better demonstrates the irregular contour and the right-angle transition of the pseudoaneurysm.
-
Aorta, trauma. Lateral screen-film angiogram shows a subtle isthmus pseudoaneurysm. Conventional subtraction image demonstrates the irregular contour of the isthmus rupture. The image also suggests a linear defect of the intimal flap. Surgical exploration confirmed subtle aortic injury. CT scan of the aortic arch (not shown) showed no abnormality in the region of the traumatic pseudoaneurysm that was demonstrated on the angiogram.
-
Aorta, trauma. Left anterior oblique (45°) angiogram shows a replaced origin of the left vertebral artery. Familiarity with normal variants such as this aortic origin of left vertebral artery is essential.
-
Aorta, trauma. Image shows the contour deformity and the calcified rim of a chronic posttraumatic aortic pseudoaneurysm.
-
Aorta, trauma. The image shows the intimal irregularity and intraluminal thrombus of the distal abdominal aorta and the proximal common iliac arteries. This obese patient had a seat-belt injury to the abdominal aorta. Physical examination showed significant ecchymosis of the abdomen. Radiographs showed blurring of the psoas margin with displacement of the ureters.