Practice Essentials
Meningiomas are the most commonly reported intracranial tumor. They represent approximately 38% of all intracranial neoplasms in females and 20% in males. Meningiomas are also the most common extra-axial tumors in the brain and the most frequently occurring tumors of mesodermal or meningeal origin. They are more common in women than men and are usually diagnosed in individuals older than 30 years. [1, 2, 3, 4]
Advances in radiologic imaging techniques, such as computed tomography (CT) scanning and magnetic resonance imaging (MRI), have improved the ability to predict the success for complete removal of the mass. Imaging information about the dural attachment site, the location and severity of edema, [5] and the displacement of critical neurovascular structures is useful for planning the operative approach and has an effect on the outcome. [6, 7]
(See the images below.)
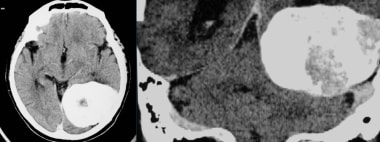
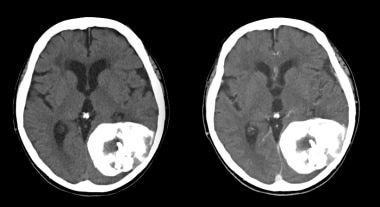
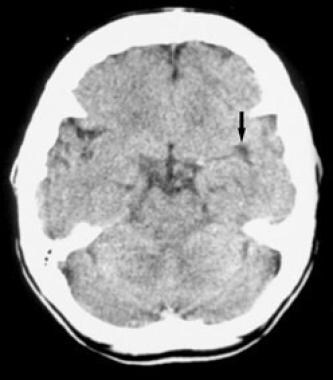
 Transverse axial CT without and with contrast shows a spoke-wheel pattern within this avidly enhancing meningioma. Although this pattern is typically seen angiographically, it can also be noted on cross-sectional imaging.
Transverse axial CT without and with contrast shows a spoke-wheel pattern within this avidly enhancing meningioma. Although this pattern is typically seen angiographically, it can also be noted on cross-sectional imaging.
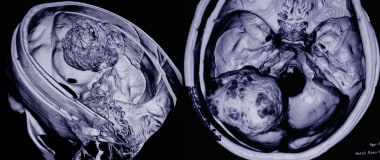
 Subsequent MRI of the previous CT with the following sequences: axial T1 post gadolinium adminsitration and axial T2 sequences. This again shows a large midline frontal meningioma with a spoke-wheel pattern.
Subsequent MRI of the previous CT with the following sequences: axial T1 post gadolinium adminsitration and axial T2 sequences. This again shows a large midline frontal meningioma with a spoke-wheel pattern.
Neuroradiologists and neurosurgeons must be aware of both the typical and the atypical imaging appearances of meningiomas, as there is some correlation with different histologic types of tumor.
The World Health Organization (WHO) classifies meningiomas into 15 subtypes under 3 major categories based on histologic characteristics and recurrence risk, as follows [1, 8, 9, 10] :
-
Grade I (typical or benign), representing ∼80% of cases; includes 9 histologic variants and lacks the anaplastic features that can be seen in grades II and III.
-
Grade II (atypical), representing ∼18% of cases; characterized by 3 or more of the following: necrosis, sheetlike growth, prominent nuclei, increased cellularity, and high nucleus/cytoplasm ratio.
-
Grade III, representing ∼2% of cases; anaplastic or malignant lesions that can be similar to high-grade sarcomas, carcinoma, or melanomas with a high rate of distant metastases; histologic variants include papillary and rhabdoid subtypes.
Significant factors contributing to recurrence include atypical and malignant histologic types and heterogeneous tumor contrast enhancement on CT scans.
Meningiomas arise from the arachnoid membranes, specifically from meningothelial cells. Most grade I typical meningiomas grow inward toward the brain as discrete well-defined, dural-based masses and are spherical or lobulated in contour. Flat tumors, termed en plaque, infiltrate the dura and grow as a thin carpet or sheet of tumor along the convexity dura, falx, or tentorium. Dural attachment of meningiomas can be pedunculated or broad-based (sessile). Because the pia and arachnoid form a membranous barrier between brain and tumor, some meningiomas grow into the subarachnoid space, but invasion of the brain is infrequent.
Grade II atypical meningiomas are often located in the calvarium and can invade overlying bone and scalp. While calcification is found in up to 25% of grade I tumors, it is a rare finding in grade II tumors. Grade III anaplastic tumors are distinguished by their agressiveness, with invasion into surrounding areas and lack of demarcation between the tumor and parenchyma. [11, 12]
Imaging modalities
MRI is preferred for the diagnosis and evaluation of brain meningiomas. [5, 13, 14, 15] Brain MRI with contrast can help distinguish extra-axial from intra-axial lesions. On brain MRI without contrast, meningiomas usually appear as hypointense on T1-weighted imaging and as hyperintense on T2-weighted imaging. MRI spectroscopy can be used to detect malignant meningiomas by comparing the metabolic and chemical contents of the healthy tissue with malignant tumor. Brain MRI also helps identify cystic lesions in meningiomas; a mushroom-like appearance reflects tumor invagination in the brain parenchyma. [1] MRI more accurately evaluates en plaque and posterior fossa meningiomas, which may be missed on CT scanning. CT scanning, however, clearly depicts bony hyperostosis, which may be difficult to appreciate on MRI.
CT scanning historically had limitations in performing direct imaging in any plane other than axial. However, with modern spiral CT scanning and multisection or multidetector-row CT (MDCT) scanning, the quality of sagittal and coronal images that can be reconstructed from axial data has increased significantly. CT scanning is less helpful than MRI in differentiating different types of soft tissue. The differential diagnosis for brain meningioma includes dural metastasis (with breast and prostate cancer being the most common primary malignancies), lymphoma and leukemia (ie, granulocytic sarcoma), [16] hemangiopericytoma, granulomatous disease (including sarcoidosis and tuberculosis), idiopathic hypertrophic pachymeningitis, extramedullary hematopoiesis, hemangioma, and dura/venous sinuses.
With certain anatomic locations, other differential diagnoses should be considered, including vestibular schwannoma for cerebellopontine angle tumors, pituitary macroadenoma and craniopharyngioma for parasellar tumors, and chordoma/chondrosarcoma for masses around the clivus.
The location of intratumoral hemorrhage, cystic changes inside or outside of the tumor mass, calcifications, invasion of the parenchyma by malignant meningiomas, and lobulated or multilobulated masses is demonstrable only with intraoperative ultrasonography.
Meningiomas can be identified incidentally on bone scans, which is thought to be secondary to factors that affect calcium deposition, as well as the presence/absence of a vascular pool. [17]
Angiography is still indispensable if embolization of the tumor is deemed necessary. [18, 19, 20]
Radiologic intervention
The development of catheters and the continued refinement of embolic materials and radiographically controlled interventional procedures have contributed to improved treatment of patients with brain meningiomas. The clinician must be aware of the active participation of the neurosurgeon and neuroradiologist in the therapy for neurosurgical patients. [21, 22, 23]
The best available treatment for benign meningiomas is complete surgical resection of the tumor. Nevertheless, interventional neuroradiologists commonly contribute in performing preoperative embolization to reduce the blood supply to the tumor. Treatment of meningiomas is benefited by embolization, but especially those with a complex presentation, giant meningiomas, meningiomas exhibiting malignant or angioblastic characteristics, or meningiomas involving the skull base, scalp, or critical vascular structures. The preoperative embolization of meningiomas is commonly used to facilitate surgery.
In a study of the effects of preoperative embolization on overall surgical outcomes after meningioma resection, preembolization and postembolization tumor enhancement patterns on MRI defined as embolization fraction correlated with decreased intraoperative blood loss and better postoperative functional outcomes. Tumor location significantly correlated with the decision to embolize preoperatively. [14]
Embolization can be carried out at the same time as the diagnostic angiography session or may occur later if detailed procedural planning is required. Distal, homogeneous, and permanent occlusion of the vascular bed by injecting small particles (150-300 microns of polyvinyl alcohol [PVA]) through microcatheters is the goal. Bilateral dural devascularization shortens the surgical resection time and permits total removal of the tumor. The procedure causes tumor necrosis, expanding the spectrum of meningiomas that can be safely resectioned during surgery.
PVA particles ranging in size from 100 to 2000 microns have been used, but the newer class of deformable particles and Bead Block have been shown to be more effective in distal embolotherapy to reach the capillary bed of the meningioma. Embospheres can be tagged with chemotherapeutic agents. Several meningiomas of the convexity have been embolized with Embospheres in our experience.
A cautious approach should be taken regarding pathologic evaluation of preoperatively embolized meningiomas; one study has suggested that preoperatively embolizing meningiomas may risk overgrading the pathologic specimen if the interpreting pathologist is not aware of the recent procedure. Features such as neoangiogenesis (microvessel density), necrosis, and prominent nucleoli should be interpreted with caution in such specimens. [24]
Approximately 2% of patients have complications associated with embolization that result in neurologic deficits. At the theoretical level, embolization may reduce the likelihood of recurrence. Embolization also may be the only treatment required in older or high-risk patients.
(See the images below.)
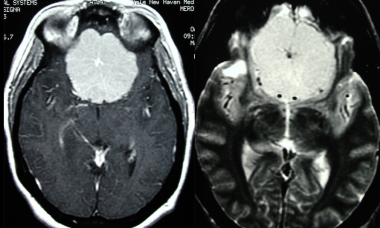
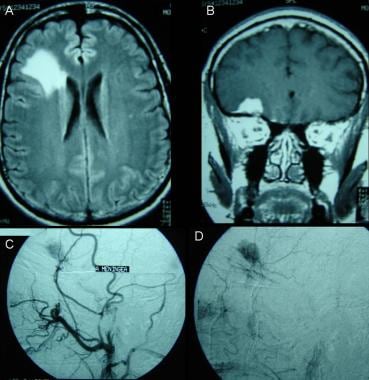
 T2-weighted magnetic resonance image shows a hyperintense mass attached to the petrous bone, within the cerebellopontine angle, in keeping with a cerebellopontine angle meningioma. Differential diagnosis includes vestibular schwannoma. Features on this image include a sharply defined tumor margin, subtle edema, and mass effect on the fourth ventricle and the brainstem. Hyperintensity on the T2-weighted image indicates a soft tumor consistency and microhypervascularity, which is seen more often in aggressive, angioblastic, or meningothelial meningioma.
T2-weighted magnetic resonance image shows a hyperintense mass attached to the petrous bone, within the cerebellopontine angle, in keeping with a cerebellopontine angle meningioma. Differential diagnosis includes vestibular schwannoma. Features on this image include a sharply defined tumor margin, subtle edema, and mass effect on the fourth ventricle and the brainstem. Hyperintensity on the T2-weighted image indicates a soft tumor consistency and microhypervascularity, which is seen more often in aggressive, angioblastic, or meningothelial meningioma.
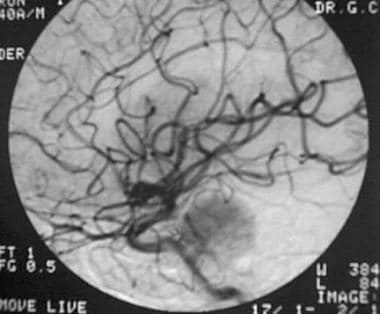
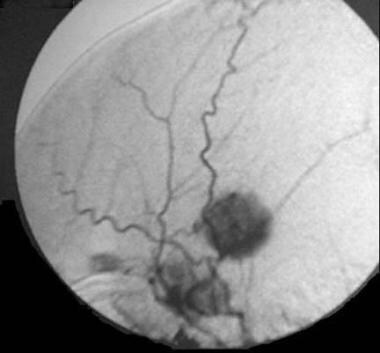
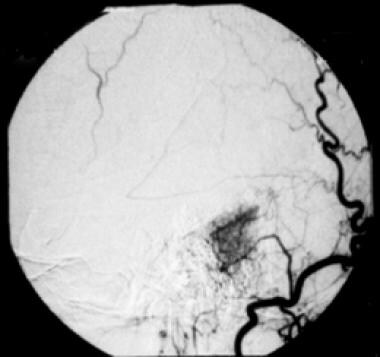 Selective angiogram of right occipital artery shows focal hypervascularity through the auricular artery. Early and delayed staining is seen in this cerebellopontine angle meningioma, characterizing the typical "mother-in-law sign."
Selective angiogram of right occipital artery shows focal hypervascularity through the auricular artery. Early and delayed staining is seen in this cerebellopontine angle meningioma, characterizing the typical "mother-in-law sign."
Radiography
In most patients, plain skull radiographs are nondiagnostic, with no features to suggest the presence of a meningioma. Some cases may demonstrate calcification or reactive hyperostosis. Rarely, osteolysis may be observed.
Meningiomas en plaque have diffuse hyperostosis, more frequently observed over the sphenoid wing and pterion. This finding results in a high degree of confidence.
Calcification within the tumor is a considerably less frequent plain radiographic manifestation; therefore, false-negative results occur. Most patients with brain meningiomas do not undergo radiographic imaging because the diagnosis has been made directly with CT scanning or MRI.
(See the images below.)
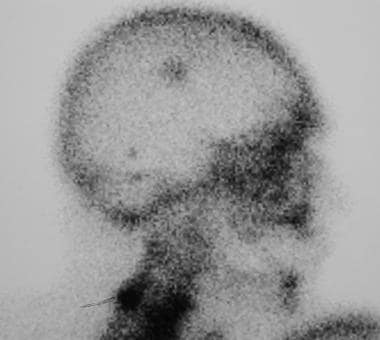
 Lateral scout radiograph shows a large densely calcified intracranial mass. This scout image was for a subsequent CT that demonstrates typical features of a meningioma.
Lateral scout radiograph shows a large densely calcified intracranial mass. This scout image was for a subsequent CT that demonstrates typical features of a meningioma.
 Transverse axial CT without and with contrast demonstrates the large calcified meningioma that was seen radiographically on the scout image.
Transverse axial CT without and with contrast demonstrates the large calcified meningioma that was seen radiographically on the scout image.
 Frontal skull radiograph illustrates a calcified mass overlying the frontal sinuses. Lateral skull radiograph localizes the mass to be arising superior to the cribriform plate. Although a meningioma could be suspected, this finding is not specific and this intracranial mass was correctly further investigated with CT.
Frontal skull radiograph illustrates a calcified mass overlying the frontal sinuses. Lateral skull radiograph localizes the mass to be arising superior to the cribriform plate. Although a meningioma could be suspected, this finding is not specific and this intracranial mass was correctly further investigated with CT.
Computed Tomography
Approximately 90% of meningiomas are demonstrated on CT scans. Typical features on unenhanced images include a well-circumscribed, smoothly marginated extra-axial mass abutting the dura. The main role of CT scanning, as opposed to MRI, is the demonstration of adjacent bone changes and calcification within the lesion. Approximately 70-75% of meningiomas are hyperattenuating to surrounding brain parenchyma, while roughly 25% are isodense. A rare group of meningiomas (the lipoblastic subtype) contain fat and are thus hypoattenuating. [25, 26, 27, 28, 29, 30, 31, 32]
Calcification is seen in approximately 20-25% of cases. The CT nature of the calcification may be nodular, fine and punctate, or dense. Surrounding parenchymal vasogenic edema is common, identified as hypodense brain tissue. Occasionally, the edema is extensive and, as it predominantly affects white matter, can resemble fingers of low attenuation. Edema, however, is absent in approximately 50% of cases because of the neoplasm's slow growth.
An advantage of CT over MRI is the evaluation of bone. [33] Underlying bone demonstrates hyperostosis in 15-20% of patients. Other bony findings include an increase in vascular markings and cortical irregularity. Less common meningioma findings include hemorrhage, cyst formation, and necrosis. Cystic components of meningiomas may be present inside the tumor or between the tumor and the adjacent brain (so-called trapped CSF).
The administration of intravenous contrast in evaluating meningiomas is helpful, as more than 90% of cases will demonstrate intense homogeneous enhancement. Inhomogeneous enhancement can result because of necrosis or rare hemorrhage. Steinhoff et al observed a nodular blush in 97% of cases, a mixed inhomogeneous blush in 0.5%, and a ring blush in 1.5%. [34] In a study by Naidich et al, tumor blush was nodular and nearly homogeneous in 70% of cases, inhomogeneous in 24%, and ringlike in 2%. [35]
Atypical CT scan features, such as irregular areas of nonenhancing mass and well-defined regions of persistent low attenuation, are the primary reason for preoperative misdiagnosis. Posterior fossa meningiomas and some en plaque lesions may be missed by CT. CT scanning can fail to demonstrate cystic changes in intracranial meningiomas. False-negative findings can occur with cystic changes in brain meningiomas. False-positive findings can occur with large dural calcification, which can mimic the disease.
(See the images below.)
 After identification on plain radiograph, this calcified intracranial mass was further investigated with CT. This transverse axial CT at the level of the superior border of the orbits demonstrates a cribriform plate meningioma.
After identification on plain radiograph, this calcified intracranial mass was further investigated with CT. This transverse axial CT at the level of the superior border of the orbits demonstrates a cribriform plate meningioma.
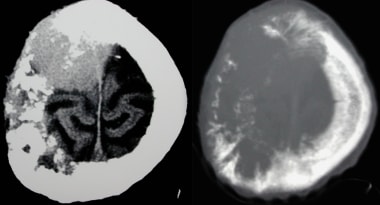 Transverse axial CT on brain and bone windows shows a large intraosseous meningioma. The findings can range from osteolysis to osteosclerosis and are non-specific. Intraosseous meningiomas represent less than 1% of osseous tumors.
Transverse axial CT on brain and bone windows shows a large intraosseous meningioma. The findings can range from osteolysis to osteosclerosis and are non-specific. Intraosseous meningiomas represent less than 1% of osseous tumors.
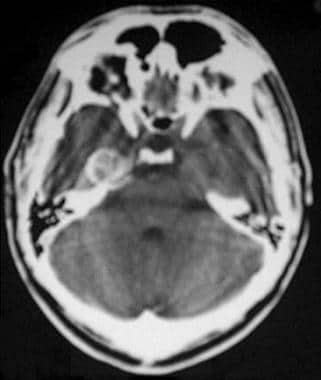 Nonenhanced computed tomography scan demonstrates a middle cranial fossa meningioma. The calcified mass is attached to the anterior ridge of the right petrous bone. Ring and punctate calcification are depicted. Edema is not appreciated.
Nonenhanced computed tomography scan demonstrates a middle cranial fossa meningioma. The calcified mass is attached to the anterior ridge of the right petrous bone. Ring and punctate calcification are depicted. Edema is not appreciated.
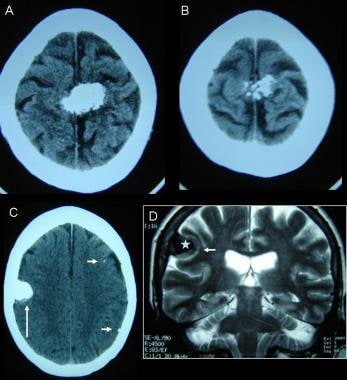 Two different cases. A, B: Computed tomography (CT) scans depict calcified meningiomas from the parietal convexity. C: Nonenhanced axial CT image shows homogeneous calcified mass attached to the right parietal bone. Soft-tissue tumor is seen at the posterior aspect of the calcification (large arrow). Other minor calcifications on the left cerebral hemisphere are caused by a parasitic disease. D: Coronal T2-weighted magnetic resonance image demonstrates calcium deposit (star) surrounded by solid tissue (small arrow); edema is not seen in this case.
Two different cases. A, B: Computed tomography (CT) scans depict calcified meningiomas from the parietal convexity. C: Nonenhanced axial CT image shows homogeneous calcified mass attached to the right parietal bone. Soft-tissue tumor is seen at the posterior aspect of the calcification (large arrow). Other minor calcifications on the left cerebral hemisphere are caused by a parasitic disease. D: Coronal T2-weighted magnetic resonance image demonstrates calcium deposit (star) surrounded by solid tissue (small arrow); edema is not seen in this case.
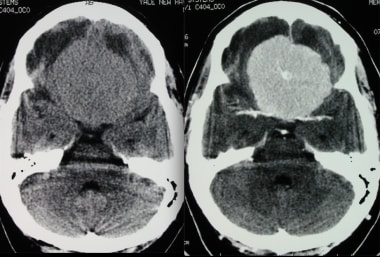
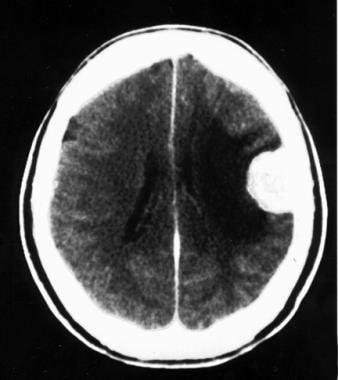
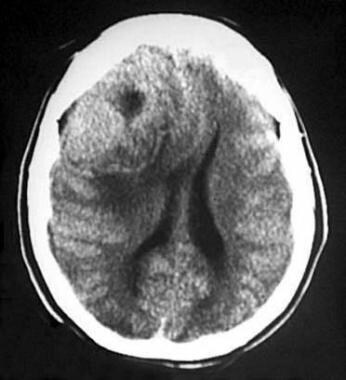 Nonenhanced computed tomography scan shows a malignant meningioma in the frontal convexity that appears as a spontaneously hyperattenuating mass. The cystic cavity may be tumor necrosis, old hemorrhage, cystic degeneration, or trapped cerebrospinal fluid. Edema and midline shift to the left anterior aspect are also present.
Nonenhanced computed tomography scan shows a malignant meningioma in the frontal convexity that appears as a spontaneously hyperattenuating mass. The cystic cavity may be tumor necrosis, old hemorrhage, cystic degeneration, or trapped cerebrospinal fluid. Edema and midline shift to the left anterior aspect are also present.
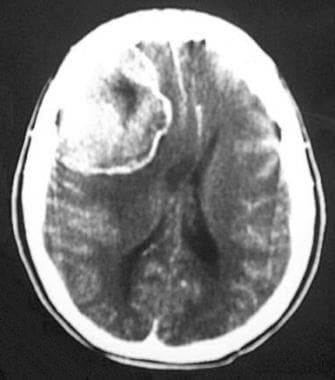 Computed tomography scan shows a malignant meningioma in the frontal convexity. A hyperattenuating and inhomogeneous enhancing mass with ring-shaped enhancement is shown.
Computed tomography scan shows a malignant meningioma in the frontal convexity. A hyperattenuating and inhomogeneous enhancing mass with ring-shaped enhancement is shown.
 Malignant frontal-convexity meningioma is demonstrated. Computed tomography scan of the frontal internal table and diploe shows erosion and bone infiltration.
Malignant frontal-convexity meningioma is demonstrated. Computed tomography scan of the frontal internal table and diploe shows erosion and bone infiltration.
 Nonenhanced computed tomography scan shows an isoattenuating sphenoid-wing meningioma. The left sylvian fissure is partially collapsed.
Nonenhanced computed tomography scan shows an isoattenuating sphenoid-wing meningioma. The left sylvian fissure is partially collapsed.
 Computed tomography scan shows an isoattenuating sphenoid-wing meningioma. The contrast-enhancing mass is attached to the major sphenoid wing and was demonstrated only after the intravenous injection of contrast material.
Computed tomography scan shows an isoattenuating sphenoid-wing meningioma. The contrast-enhancing mass is attached to the major sphenoid wing and was demonstrated only after the intravenous injection of contrast material.
 Contrast-enhanced computed tomography scan shows a parietal convexity meningioma, characterized by a round, hyperattenuating, and unilobulated mass. Broad-based attachment to the dura is demonstrated, as is intense edema in the subjacent brain.
Contrast-enhanced computed tomography scan shows a parietal convexity meningioma, characterized by a round, hyperattenuating, and unilobulated mass. Broad-based attachment to the dura is demonstrated, as is intense edema in the subjacent brain.
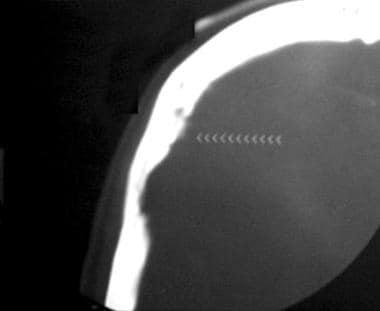
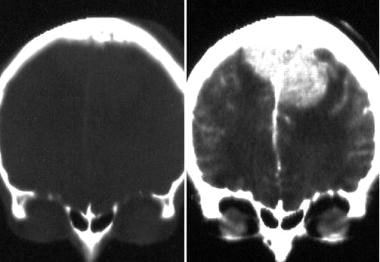 Computed tomography (CT) scanning is the imaging technique most commonly used to evaluate bone changes and calcium in meningiomas. Plain radiography can show calcium in 20% of patients. This image demonstrates bone changes on a coronal CT scan with bone window settings.
Computed tomography (CT) scanning is the imaging technique most commonly used to evaluate bone changes and calcium in meningiomas. Plain radiography can show calcium in 20% of patients. This image demonstrates bone changes on a coronal CT scan with bone window settings.
 Posterior tentorial meningioma on a coronal contrast-enhanced computed tomography scan. A hyperattenuating and well-marginated mass is adjacent to the tentorium. Pooling of cerebrospinal fluid, subtle edema, homogeneous enhancement, and ventricular dilatation are demonstrated.
Posterior tentorial meningioma on a coronal contrast-enhanced computed tomography scan. A hyperattenuating and well-marginated mass is adjacent to the tentorium. Pooling of cerebrospinal fluid, subtle edema, homogeneous enhancement, and ventricular dilatation are demonstrated.
Magnetic Resonance Imaging
MRI with gadolinium is the best imaging modality for evaluating meningiomas. Important advantages of MRI in the imaging of meningiomas are the superior resolution of different types of soft tissue, multiplanar capability, and 3-dimensional (3-D) reconstruction ability. [1, 36, 37] MRI can demonstrate tumor vascularity, arterial encasement, venous sinus invasion, and the relationship between the tumor and surrounding structures. This modality is particularly advantageous in depicting the juxtasellar area and the posterior fossa and in demonstrating the rare presence of disseminated disease via the CSF. The multiplanar capability is often the best means to visualize the broad contact of tumors to the meninges, tumor capsules, and meningeal contrast enhancement adjacent to the tumor. [38, 39, 40, 41]
On nonenhanced T1-weighted images, most meningiomas have no signal intensity difference compared with cortical gray matter. Fibromatous meningiomas may be more hypointense than the cerebral cortex. T1-weighted images may be used to asses for necrosis, hemorrhagic products, and cysts. On T2-weighted images, signal is variable. T2-weighted images are useful in assessing for hemorrhagic products and cysts, as well. Additionally, this sequence is used to assess for a CSF cleft between the neoplasm and brain parenchyma, confirming an extra-axial location.
Hyperintensity on T2-weighted images indicates soft-tumor consistency and microhypervascularity. This is seen more often in aggressive, angioblastic, or meningothelial tumors. T2-weighted signal intensity is best correlated with both the histology and the consistency of the meningioma. Generally, low-intensity portions of the tumor indicate a more fibrous and harder character (eg, fibroblastic meningiomas), whereas higher-intensity portions indicate a softer character (eg, angioblastic tumor). [42, 43, 44]
Fluid-attenuated inversion recovery (FLAIR) sequences are useful to assess for associated edema, as well as for the characteristic feature of a dural tail. The dural tail represents a collar of thickened, enhancing dura that surrounds the tumor's dural attachment. A dural tail occurs in approximately 65% of meningiomas, as well as 15% of other tumors. Although this finding is not specific for meningiomas, it is highly suggestive of the diagnosis.
On MRI and CT, meningiomas exhibit the same enhancement appearance after the injection of contrast medium. Intense enhancement following gadolinium is seen in more than 85% of tumors. A ring appearance may represent a capsule. Gadolinium also enables better visualization of en plaque meningiomas that may be more subtle on unenhanced sequences.
(See the images below.)
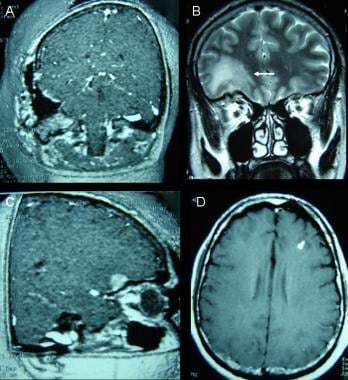
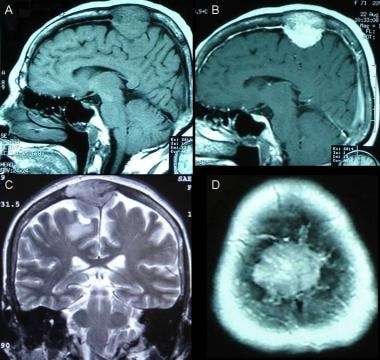 Parasagittal meningioma. A: Nonenhanced sagittal T1-weighted magnetic resonance image (MRI) shows a solid dural isointense mass with bone invasion and compression against the parietal cortex. B: Contrast-enhanced sagittal T1-weighted MRI demonstrates partially intense enhancement of the tumor. C: Coronal T2-weighted image shows isointense mass meaning hard tissue. This finding is observed on fibroblastic meningiomas. D: Contrast-enhanced T1-weighted axial MRI shows hyperintense image located within the bony marrow.
Parasagittal meningioma. A: Nonenhanced sagittal T1-weighted magnetic resonance image (MRI) shows a solid dural isointense mass with bone invasion and compression against the parietal cortex. B: Contrast-enhanced sagittal T1-weighted MRI demonstrates partially intense enhancement of the tumor. C: Coronal T2-weighted image shows isointense mass meaning hard tissue. This finding is observed on fibroblastic meningiomas. D: Contrast-enhanced T1-weighted axial MRI shows hyperintense image located within the bony marrow.
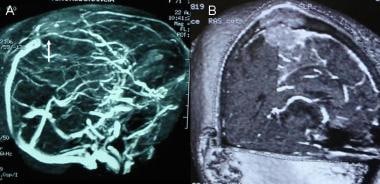 A: Noncontrast angio-magnetic resonance image (MRI) on lateral view demonstrates occluded superior sagittal sinus due to meningioma invasion. B: MRI reconstruction shows sagittal venous obstruction and 3-dimensional (3-D) appearance of the tumor.
A: Noncontrast angio-magnetic resonance image (MRI) on lateral view demonstrates occluded superior sagittal sinus due to meningioma invasion. B: MRI reconstruction shows sagittal venous obstruction and 3-dimensional (3-D) appearance of the tumor.
 Nonenhanced T1-weighted sagittal magnetic resonance image demonstrates a typical parasagittal meningioma. A homogeneous, long-T1, round mass with thin capsule is present. The tumor is attached to the left sagittal dura. Mass effect is noted against the ventricular trigone.
Nonenhanced T1-weighted sagittal magnetic resonance image demonstrates a typical parasagittal meningioma. A homogeneous, long-T1, round mass with thin capsule is present. The tumor is attached to the left sagittal dura. Mass effect is noted against the ventricular trigone.
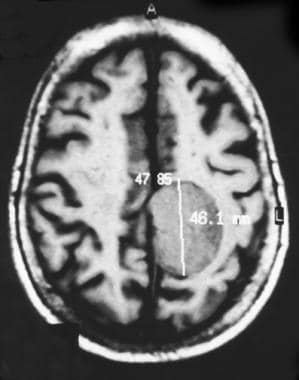 Nonenhanced axial magnetic resonance image demonstrates a typical parasagittal meningioma. T1-weighted image shows a homogeneous, long-T1, round mass with thin capsule. The tumor is attached to the left side of the falx. Mass effect is noted on the adjacent gyri.
Nonenhanced axial magnetic resonance image demonstrates a typical parasagittal meningioma. T1-weighted image shows a homogeneous, long-T1, round mass with thin capsule. The tumor is attached to the left side of the falx. Mass effect is noted on the adjacent gyri.
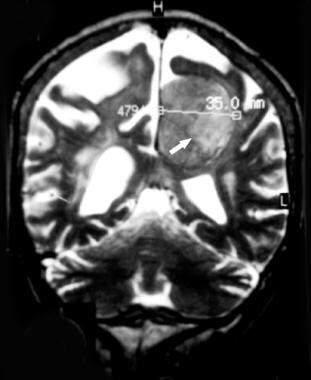 Coronal T2-weighted magnetic resonance image demonstrates a typical parasagittal meningioma. Isointense and inhomogeneous tumor without peripheral edema indicates a more fibrous and harder character (ie, a fibroblastic meningioma).
Coronal T2-weighted magnetic resonance image demonstrates a typical parasagittal meningioma. Isointense and inhomogeneous tumor without peripheral edema indicates a more fibrous and harder character (ie, a fibroblastic meningioma).
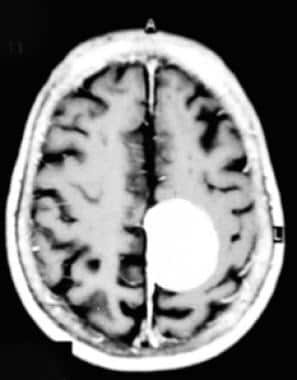 Contrast-enhanced T1-weighted axial magnetic resonance image demonstrates a typical parasagittal meningioma. A homogeneous, enhancing, globose mass is depicted.
Contrast-enhanced T1-weighted axial magnetic resonance image demonstrates a typical parasagittal meningioma. A homogeneous, enhancing, globose mass is depicted.
 Contrast-enhanced T1-weighted coronal magnetic resonance image shows a typical parasagittal meningioma. A homogeneous, enhancing, globose mass is depicted.
Contrast-enhanced T1-weighted coronal magnetic resonance image shows a typical parasagittal meningioma. A homogeneous, enhancing, globose mass is depicted.
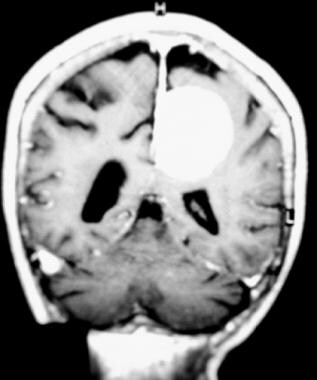
 Axial T2 weighted MRI image shows a midline frontal meningioma. High T2 signal rim surrounding the mass is consistent with CSF fluid, confirming the extra-axial location. This is a classic "CSF cleft sign" of extra-axial tumors, such as meningiomas.
Axial T2 weighted MRI image shows a midline frontal meningioma. High T2 signal rim surrounding the mass is consistent with CSF fluid, confirming the extra-axial location. This is a classic "CSF cleft sign" of extra-axial tumors, such as meningiomas.
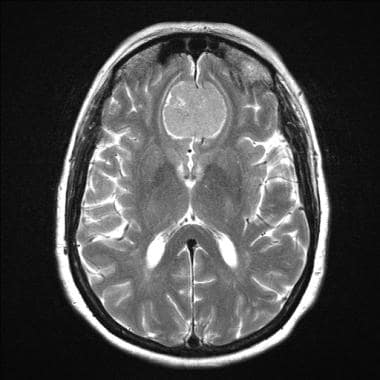
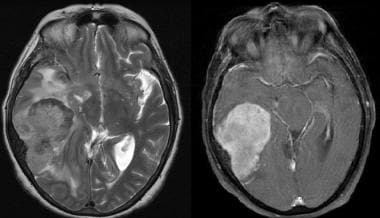 Multisequence MR images, including axial T2 and axial T1 post-gadolinium, demonstrate a large right temporal meningioma with a spoke-wheel pattern, local mass effect, surrounding edema, and underlying hyperostosis.
Multisequence MR images, including axial T2 and axial T1 post-gadolinium, demonstrate a large right temporal meningioma with a spoke-wheel pattern, local mass effect, surrounding edema, and underlying hyperostosis.
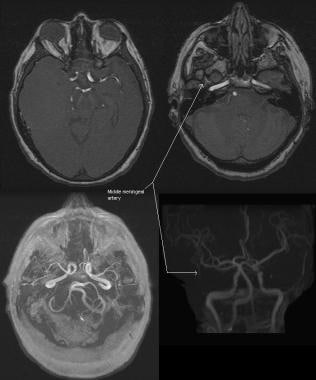 An MR angiogram was performed on the previous case, with the following sequences: MRA through the level of the middle cerebral arteries, MRA through the level of the petrous segment of the internal carotid arteries, collapsed MRA, and MRA projection. These images demonstrate an additional finding of the large right temporal meningioma supplied by the middle meningeal artery (a branch off the external carotid arterial system). Identification of this finding is important for presurgical consideration of embolization.
An MR angiogram was performed on the previous case, with the following sequences: MRA through the level of the middle cerebral arteries, MRA through the level of the petrous segment of the internal carotid arteries, collapsed MRA, and MRA projection. These images demonstrate an additional finding of the large right temporal meningioma supplied by the middle meningeal artery (a branch off the external carotid arterial system). Identification of this finding is important for presurgical consideration of embolization.
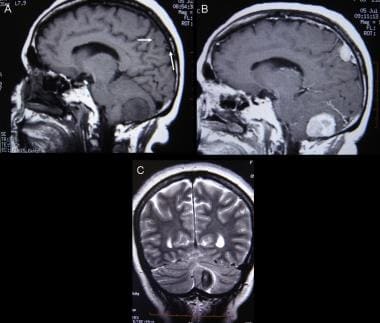 Multiple meningiomas. A: Sagittal T1-weighted magnetic resonance image (MRI) demonstrates posterior fossa and parietal meningiomas. B: Gadolinium enhancement on sagittal T1-weighted MRI shows intense enhancing of the masses. C: T2-weighted coronal MRI shows stable hypointense appearance of the posterior mass after endovascular embolization.
Multiple meningiomas. A: Sagittal T1-weighted magnetic resonance image (MRI) demonstrates posterior fossa and parietal meningiomas. B: Gadolinium enhancement on sagittal T1-weighted MRI shows intense enhancing of the masses. C: T2-weighted coronal MRI shows stable hypointense appearance of the posterior mass after endovascular embolization.
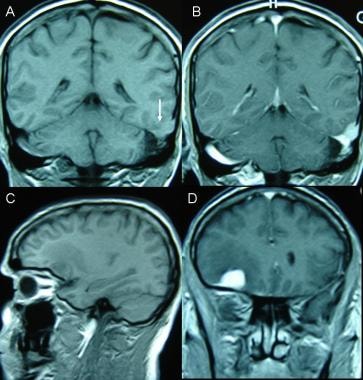 Malignant and multiple meningiomas. A 47-year-old white male underwent gamma knife surgery due to left convexity meningioma, followed by microsurgical removal of the tumor. A, B: Four years later, MRI showed a stable residual parietal/occipital mass. The left sigmoid sinus is occluded. C, D: One small right frontal meningioma also underwent radiosurgery at the same time. Edema and intense enhancing after gadolinium injection is demonstrated.
Malignant and multiple meningiomas. A 47-year-old white male underwent gamma knife surgery due to left convexity meningioma, followed by microsurgical removal of the tumor. A, B: Four years later, MRI showed a stable residual parietal/occipital mass. The left sigmoid sinus is occluded. C, D: One small right frontal meningioma also underwent radiosurgery at the same time. Edema and intense enhancing after gadolinium injection is demonstrated.
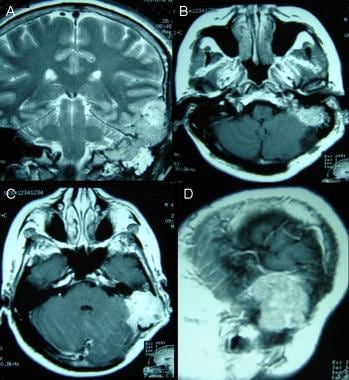 A-D: Coronal T2-weighted and enhanced T1-weighted magnetic resonance images demonstrate quick growth of a convexity mass toward the tentorium and the petrous bone. This bone structure is filled with liquid in its inferior aspect. Surgical biopsy reported "atypical meningioma."
A-D: Coronal T2-weighted and enhanced T1-weighted magnetic resonance images demonstrate quick growth of a convexity mass toward the tentorium and the petrous bone. This bone structure is filled with liquid in its inferior aspect. Surgical biopsy reported "atypical meningioma."
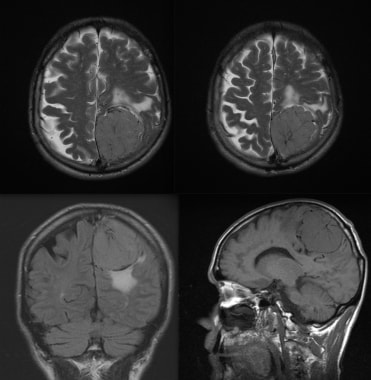 MRI images with the following sequences: axial T2, axial T2, coronal FLAIR, and sagittal T1. A large left-sided meningioma shows a spoke-wheel pattern within an extra-axial mass with surrounding edema.
MRI images with the following sequences: axial T2, axial T2, coronal FLAIR, and sagittal T1. A large left-sided meningioma shows a spoke-wheel pattern within an extra-axial mass with surrounding edema.
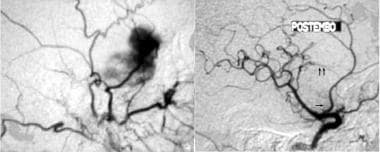
 Frontal meningioma. A, B: Slow growth and surrounding edema is seen on magnetic resonance imaging (MRI) control of this tumor. Coronal, enhanced-T1 weighted and fluid attenuation inversion recovery (FLAIR) sequences are shown. C, D: Digital angiography. Right middle meningeal branch demonstrates feeding of the tumor. It was not embolized.
Frontal meningioma. A, B: Slow growth and surrounding edema is seen on magnetic resonance imaging (MRI) control of this tumor. Coronal, enhanced-T1 weighted and fluid attenuation inversion recovery (FLAIR) sequences are shown. C, D: Digital angiography. Right middle meningeal branch demonstrates feeding of the tumor. It was not embolized.
 A: 3-dimensional (3-D)-enhanced T1-weighted magnetic resonance image (MRI) image shows residual meningioma at the cranial base after second surgical removal. B: Coronal T2-weighted MRI shows intense edema surrounding the frontal mass. C: 3-D image on enhanced T1-weighted MRI demonstrates frontal meningioma underlying the orbital right sulcus. D: Gadolinium-enhanced, axial T1-weighted image shows 1 of the 3 focal hyperintense masses discovered only on this sequence. Brain metastases from meningioma have not been proved.
A: 3-dimensional (3-D)-enhanced T1-weighted magnetic resonance image (MRI) image shows residual meningioma at the cranial base after second surgical removal. B: Coronal T2-weighted MRI shows intense edema surrounding the frontal mass. C: 3-D image on enhanced T1-weighted MRI demonstrates frontal meningioma underlying the orbital right sulcus. D: Gadolinium-enhanced, axial T1-weighted image shows 1 of the 3 focal hyperintense masses discovered only on this sequence. Brain metastases from meningioma have not been proved.
Histologic subtypes may have different MRI appearances, but this does not suffice for a histologic diagnosis by using MRI.
Most meningiomas can be diagnosed by conventional MRI. [27, 28, 45, 46, 47, 48, 49, 50, 51, 18, 52, 53] However, atypical features can lead to uncertainty in diagnosis.
MR spectroscopy (MRS) has been studied to aid in differentiating meningiomas from other mimics. Studies have consistently demonstrated increased levels of alanine, choline, and glutamate-glutamine complex and decreased levels of N-acetylaspartate and creatine. [54] Specifically, elevated signal intensities for glutamine at 3.8 ppm and alanine at 1.48 ppm have been reported. [55] Lactate and lipid levels, although correlated well with malignancy of gliomas and metastases, remain controversial in their value in evaluating meningiomas. Low myoinositol and creatine have been shown to be characteristic in meningiomas. [56]
Phosphorus-31 MRS has shown a characteristic alkaline environment and low levels of phosphocreatine and phosphodiesterases. [57]
(See the images below.)
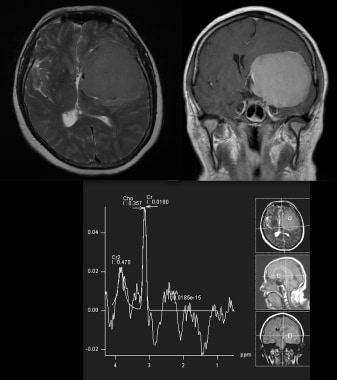
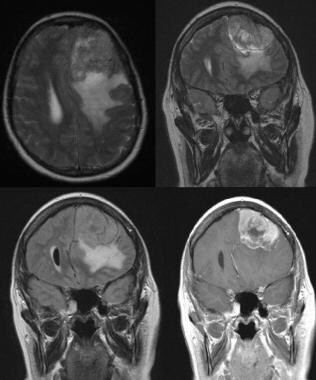 MRI of the brain with the following sequences: axial T2, coronal T2, coronal FLAIR, and coronal T1 post gadolinium administration. Shown is a left frontal meningioma with a spoke-wheel pattern, underlying hyperostosis of the calvarium, and surrounding parenchymal edema.
MRI of the brain with the following sequences: axial T2, coronal T2, coronal FLAIR, and coronal T1 post gadolinium administration. Shown is a left frontal meningioma with a spoke-wheel pattern, underlying hyperostosis of the calvarium, and surrounding parenchymal edema.
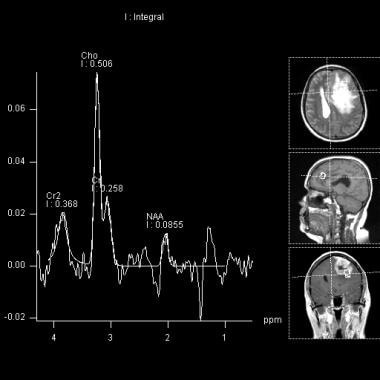 This MR spectroscopy of the previous MRI demonstrates elevated choline and low NAA levels, typical of meningiomas. Additional characteristic meningioma MRS features include increased alanine and glutamate-glutamine complex and decreased creatine. Elevated signal intensities, specifically at 3.8 ppm (glutamine) and 1.48 ppm (alanine), have been reported. Lipid and lactate levels remain controversial in meningioma evaluation.
This MR spectroscopy of the previous MRI demonstrates elevated choline and low NAA levels, typical of meningiomas. Additional characteristic meningioma MRS features include increased alanine and glutamate-glutamine complex and decreased creatine. Elevated signal intensities, specifically at 3.8 ppm (glutamine) and 1.48 ppm (alanine), have been reported. Lipid and lactate levels remain controversial in meningioma evaluation.
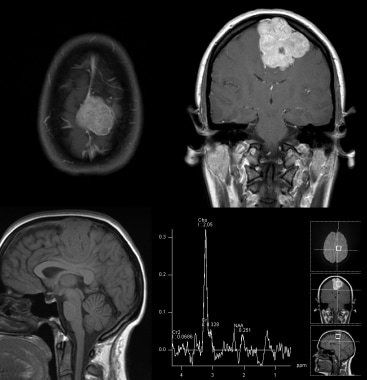
 MRI with the following sequences: axial T2, coronal T1 post gadolinium administration, and MR spectroscopy. Findings of this large meningioma include CSF encompassing the mass, a classic "CSF cleft sign," confirming an extra-axial location. Additional features include significant mass effect with effacement of the left lateral ventricle. Note the avid homogeneous enhancement after gadolinium is administered. MRS shows elevated choline and low NAA as classic features.
MRI with the following sequences: axial T2, coronal T1 post gadolinium administration, and MR spectroscopy. Findings of this large meningioma include CSF encompassing the mass, a classic "CSF cleft sign," confirming an extra-axial location. Additional features include significant mass effect with effacement of the left lateral ventricle. Note the avid homogeneous enhancement after gadolinium is administered. MRS shows elevated choline and low NAA as classic features.
 MRI with the following sequences: axial T1 post gadolinium administration, coronal T1 post gadolinium, sagittal T1, and MR spectroscopy. This meningioma shows avid enhancement and invasion into the superior sagittal sinus. MRS shows elevated choline and low NAA as typical meningioma features.
MRI with the following sequences: axial T1 post gadolinium administration, coronal T1 post gadolinium, sagittal T1, and MR spectroscopy. This meningioma shows avid enhancement and invasion into the superior sagittal sinus. MRS shows elevated choline and low NAA as typical meningioma features.
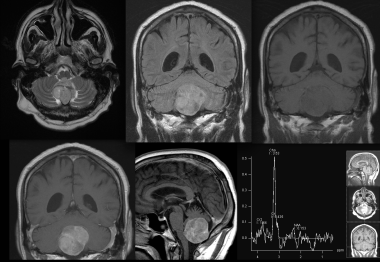 MRI images with the following sequences: axial T2, coronal FLAIR, coronal T1, coronal T1 post gadolinium administration, sagittal T1 post gadolinium, and MR spectroscopy. This MRI characterizes the posterior fossa meningioma to be within the cisterna magna, exerting mass effect with superior displacement of the cerebellum. Avid enhancement is seen after gadolinium is administered. MRS features include elevated choline and relatively absent NAA.
MRI images with the following sequences: axial T2, coronal FLAIR, coronal T1, coronal T1 post gadolinium administration, sagittal T1 post gadolinium, and MR spectroscopy. This MRI characterizes the posterior fossa meningioma to be within the cisterna magna, exerting mass effect with superior displacement of the cerebellum. Avid enhancement is seen after gadolinium is administered. MRS features include elevated choline and relatively absent NAA.
Diffusion-weighted MRI has been evaluated with varying conclusions. Apparent diffusion coefficients (ADC) have been shown to typically be lower than surrounding brain for high-grade neoplasms. Some studies have shown a similar trend for meningiomas, while other studies have found ADC values for grade I and grade II meningiomas to not be statistically different. [2]
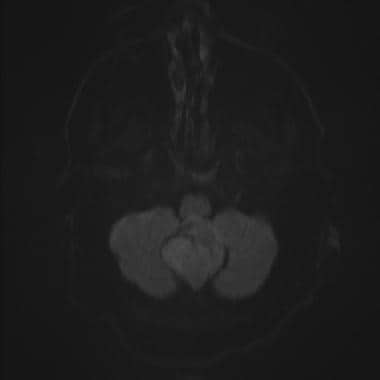 Diffusion weighted MRI of the posterior fossa meningioma demonstrates mildly increased signal, in keeping with mild diffusion restriction.
Diffusion weighted MRI of the posterior fossa meningioma demonstrates mildly increased signal, in keeping with mild diffusion restriction.
Perfusion-weighted MRI has been studied, with several conclusions. Hypervascular meningiomas will typically demonstrate increased perfusion. Perfusion-weighted MRI has also been evaluated to assess meningioma tumor subtype, as well as to follow postintervention success. [2]
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans.
An apparent diffusion coefficient (ADC) of 0.85 using diffusion-weighted MRI was found to differentiate grade I meningioma from grade II and III tumors. In the study of 389 patients, World Health Organization grade I was diagnosed in 271 cases (69.7%), grade II in 103 (26.5%), and grade III in 15 (3.9%). [13]
MR elastography (MRe) has been studied for its ability to assess tumor consistency and evaluate invasiveness of adjacent structures. [58]
In general, the sensitivity and specificity of MRI are high in the diagnosis of meningiomas. MRI has proved to be superior in delineation of the tumor and its relation with surrounding structures. However, MRI is unreliable for recognition of tumor calcification, and acute hemorrhage is often difficult to image with this modality.
False-negative findings of tumor calcium must be considered. Delineation of acute hemorrhage into tumor with conventional sequences is a disadvantage of MRI and may generate false findings.
Nuclear Imaging
Meningiomas can be identified incidentally on bone scans. This is thought to be secondary to factors that affect calcium deposition, as well as the presence/absence of a vascular pool. [17] Numerous single photon emission computed tomography (SPECT) and positron emission tomography (PET) radiolabeled tracers have been evaluated with respect to meningiomas and may assist in further differentiating between biological features and specific subtypes of meningiomas. Nuclear medicine, specifically SPECT and PET, may have a role in several areas of meningioma management, including establishing a diagnosis and differential diagnosis, planning radiation treatment, predicting tumor grade, predicting likelihood of recurrence, assessing treatment response, and differentiating residual tumor from posttreatment fibrosis. [59, 60, 61]
(See the images below.)
 Lateral skull projection of a bone scan shows a small focus of increased uptake that overlying the mid skull. Subsequent CT demonstrated a small right posterior frontal meningioma. The uptake on bone scan is thought to be secondary to calcium deposition factors as well as the presence/absence of a vascular pool.
Lateral skull projection of a bone scan shows a small focus of increased uptake that overlying the mid skull. Subsequent CT demonstrated a small right posterior frontal meningioma. The uptake on bone scan is thought to be secondary to calcium deposition factors as well as the presence/absence of a vascular pool.
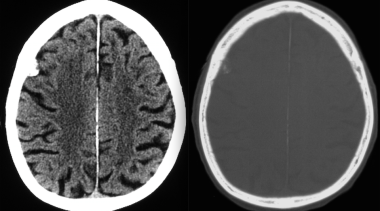 Transverse axial CT at the level of the centrum semiovale on brain and bone windows illustrates a small right posterior frontal meningioma that was detected on bone scan. Bone windows illustrate typical meningioma features of hyperostosis and cortical irregularity underlying the mass. Partial calcification of the meningioma is also noted.
Transverse axial CT at the level of the centrum semiovale on brain and bone windows illustrates a small right posterior frontal meningioma that was detected on bone scan. Bone windows illustrate typical meningioma features of hyperostosis and cortical irregularity underlying the mass. Partial calcification of the meningioma is also noted.
SPECT evaluation of meningiomas has demonstrated several characteristic features. Thallium-201 has shown accumulation in several brain tumors, including meningiomas. Studies have suggested that long-lasting uptake in meningiomas could be utilized to predict malignant likelihood and tumor aggressiveness, and it has been associated with vascular endothelial growth factor positivity. [59]
Numerous studies have identified characteristic features of meningiomas using technetium-labeled compounds, such as 99mTc-methoxyisobutylisonitrile (MIBI) and 99mTc-tetrofosmin (TF), as well as somatostatin receptor scintigraphy (111In-octreotide and 99mTc-depreotide). [59]
PET has been studied using 18F-FDG (18F-fluorodeoxyglucose), with mixed results: some papers have suggested an FDG avidity to differentiate benign from malignant meningiomas, while other papers contradict this finding. One of the major complicating factors of FDG evaluation is the normal high uptake in cerebral cortex. Multiple other PET tracers have been studied, with mixed results. [59]
Angiography
Although magnetic resonance angiography (MRA and magnetic resonance venography [MRV]) have decreased the role of classical angiography, the latter remains a powerful tool for embolization and planning surgery. Angiography is still indispensable if embolization of the tumor is deemed necessary. [18, 19, 20]
Meningiomas are supplied by meningeal branches of the internal and external carotid artery (see the following images). Basal meningiomas of the anterior and middle cranial fossa and meningiomas of the wings of the sphenoid bone are commonly supplied by the internal carotid artery. Other supratentorial meningiomas are supplied by the internal and external carotid arteries.
 This angiogram of the internal carotid artery demonstrates considerable supply of a middle cranial fossa meningioma from a petrous branch. The external carotid artery, however, provided the main blood supply to the tumor.
This angiogram of the internal carotid artery demonstrates considerable supply of a middle cranial fossa meningioma from a petrous branch. The external carotid artery, however, provided the main blood supply to the tumor.
 Lateral projection from internal carotid angiography shows multiple opacified tumoral vessels in a radial distribution, characterizing this parasellar meningioma. Circumferential narrowing of the supraclinoid carotid portion is depicted.
Lateral projection from internal carotid angiography shows multiple opacified tumoral vessels in a radial distribution, characterizing this parasellar meningioma. Circumferential narrowing of the supraclinoid carotid portion is depicted.
Tumors that arise along the falx, the sphenoidal ridge, and the convexity are supplied by the middle meningeal artery. Falcine meningiomas can be supplied additionally by the anterior meningeal artery. Parasellar and tentorium tumors are supplied by the hypophyseal meningeal artery. Direct meningeal arteries from the cavernous sinus can supply meningiomas of the middle cranial fossa. Intraventricular tumors are supplied by anterior and posterior choroidal arteries.
 Selective injection of the left middle meningeal artery shows inhomogeneous enhancing tumor, consistent with a parietal-convexity meningioma. Intense vascularity is appreciated on the posterior aspect of the mass. Drainage veins are not seen.
Selective injection of the left middle meningeal artery shows inhomogeneous enhancing tumor, consistent with a parietal-convexity meningioma. Intense vascularity is appreciated on the posterior aspect of the mass. Drainage veins are not seen.
External carotid and vertebral branches supply tumors of the posterior fossa. Large meningiomas can be supplied by pia vessels around the tumor.
Meningeal arteries penetrate to a meningioma through its dural attachment with inside branches radially distributed like sunrays, creating the typical "sunburst" appearance. Homogeneous sharp tumor staining is seen early and remains late and, as such, has been called "the mother-in-law sign." Usually, meningiomas do not exhibit drainage veins, although angioblastic types may.
In summary, angiography is useful in delineating the blood supply of the external versus internal carotid arteries and can show encasement of intracranial vessels. Angiography demonstrates an arterial map for preoperative embolization.
 Selective angiogram of right occipital artery shows focal hypervascularity through the auricular artery. Early and delayed staining is seen in this cerebellopontine angle meningioma, characterizing the typical "mother-in-law sign."
Selective angiogram of right occipital artery shows focal hypervascularity through the auricular artery. Early and delayed staining is seen in this cerebellopontine angle meningioma, characterizing the typical "mother-in-law sign."
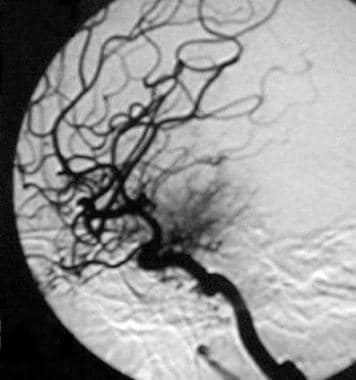
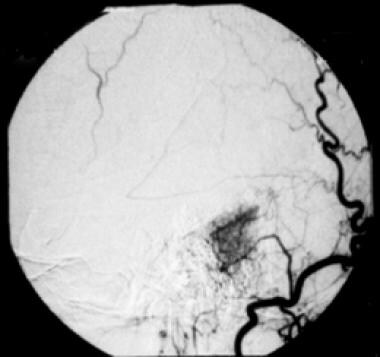
 This angiogram demonstrates successful embolization of this cerebellopontine angle meningioma prior to surgery, via embolization of the right occipital artery with polyvinyl alcohol particles.
This angiogram demonstrates successful embolization of this cerebellopontine angle meningioma prior to surgery, via embolization of the right occipital artery with polyvinyl alcohol particles.
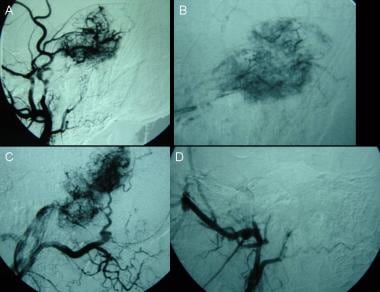 Digital subtraction angiography. A, B: Left external carotid artery shows early and delayed stain of the mass through middle meningeal and superficial temporal arteries. C: Occipital artery. D: The branches were embolized before the surgical procedure. The tumor was partially removed due to cranial base involvement.
Digital subtraction angiography. A, B: Left external carotid artery shows early and delayed stain of the mass through middle meningeal and superficial temporal arteries. C: Occipital artery. D: The branches were embolized before the surgical procedure. The tumor was partially removed due to cranial base involvement.
 Embolization may be the only treatment required in older or high-risk patients. Meningeal vessels from the internal carotid artery should supply the tumor. Mass effect should persist after embolization of the middle meningeal artery.
Embolization may be the only treatment required in older or high-risk patients. Meningeal vessels from the internal carotid artery should supply the tumor. Mass effect should persist after embolization of the middle meningeal artery.
As an alternative to traditional catheter angiography, 3-D CT angiography may depict the relationship between skull base meningiomas and neighboring bony and vascular structures clearly, quickly, and with minimal risk to the patient.
Angiography has a high degree of confidence in recognizing the arterial source of the meningioma. Tumor feeding can be identified with a low rate of false-positive and/or false-negative findings.
Arterial findings have a high sensitivity and specificity in the diagnosis of meningiomas. Angiography shows an arterial map for preoperative embolization with a low false-finding rate.
-
Posterior tentorial meningioma on a coronal contrast-enhanced computed tomography scan. A hyperattenuating and well-marginated mass is adjacent to the tentorium. Pooling of cerebrospinal fluid, subtle edema, homogeneous enhancement, and ventricular dilatation are demonstrated.
-
Nonenhanced computed tomography scan shows a malignant meningioma in the frontal convexity that appears as a spontaneously hyperattenuating mass. The cystic cavity may be tumor necrosis, old hemorrhage, cystic degeneration, or trapped cerebrospinal fluid. Edema and midline shift to the left anterior aspect are also present.
-
Computed tomography scan shows a malignant meningioma in the frontal convexity. A hyperattenuating and inhomogeneous enhancing mass with ring-shaped enhancement is shown.
-
Malignant frontal-convexity meningioma is demonstrated. Computed tomography scan of the frontal internal table and diploe shows erosion and bone infiltration.
-
Nonenhanced computed tomography scan shows an isoattenuating sphenoid-wing meningioma. The left sylvian fissure is partially collapsed.
-
Computed tomography scan shows an isoattenuating sphenoid-wing meningioma. The contrast-enhancing mass is attached to the major sphenoid wing and was demonstrated only after the intravenous injection of contrast material.
-
Contrast-enhanced computed tomography scan shows a parietal convexity meningioma, characterized by a round, hyperattenuating, and unilobulated mass. Broad-based attachment to the dura is demonstrated, as is intense edema in the subjacent brain.
-
Selective injection of the left middle meningeal artery shows inhomogeneous enhancing tumor, consistent with a parietal-convexity meningioma. Intense vascularity is appreciated on the posterior aspect of the mass. Drainage veins are not seen.
-
Nonenhanced T1-weighted sagittal magnetic resonance image demonstrates a typical parasagittal meningioma. A homogeneous, long-T1, round mass with thin capsule is present. The tumor is attached to the left sagittal dura. Mass effect is noted against the ventricular trigone.
-
Nonenhanced axial magnetic resonance image demonstrates a typical parasagittal meningioma. T1-weighted image shows a homogeneous, long-T1, round mass with thin capsule. The tumor is attached to the left side of the falx. Mass effect is noted on the adjacent gyri.
-
Coronal T2-weighted magnetic resonance image demonstrates a typical parasagittal meningioma. Isointense and inhomogeneous tumor without peripheral edema indicates a more fibrous and harder character (ie, a fibroblastic meningioma).
-
Contrast-enhanced T1-weighted axial magnetic resonance image demonstrates a typical parasagittal meningioma. A homogeneous, enhancing, globose mass is depicted.
-
Contrast-enhanced T1-weighted coronal magnetic resonance image shows a typical parasagittal meningioma. A homogeneous, enhancing, globose mass is depicted.
-
Lateral projection from internal carotid angiography shows multiple opacified tumoral vessels in a radial distribution, characterizing this parasellar meningioma. Circumferential narrowing of the supraclinoid carotid portion is depicted.
-
Nonenhanced computed tomography scan demonstrates a middle cranial fossa meningioma. The calcified mass is attached to the anterior ridge of the right petrous bone. Ring and punctate calcification are depicted. Edema is not appreciated.
-
A middle cranial fossa meningioma is demonstrated by this contrast-enhanced computed tomography scan, characterized by a round enhancing extra-axial mass.
-
A middle cranial fossa meningioma is depicted in this contrast-enhanced computed tomography scan showing a dense, enhancing mass.
-
This angiogram of the internal carotid artery demonstrates considerable supply of a middle cranial fossa meningioma from a petrous branch. The external carotid artery, however, provided the main blood supply to the tumor.
-
Off-midline sagittal nonenhanced T1-weighted magnetic resonance image displays a hypointense and inhomogeneous round mass in the cerebellopontine angle. This is a cerebellopontine angle meningioma.
-
T2-weighted magnetic resonance image shows a hyperintense mass attached to the petrous bone, within the cerebellopontine angle, in keeping with a cerebellopontine angle meningioma. Differential diagnosis includes vestibular schwannoma. Features on this image include a sharply defined tumor margin, subtle edema, and mass effect on the fourth ventricle and the brainstem. Hyperintensity on the T2-weighted image indicates a soft tumor consistency and microhypervascularity, which is seen more often in aggressive, angioblastic, or meningothelial meningioma.
-
Selective angiogram of right occipital artery shows focal hypervascularity through the auricular artery. Early and delayed staining is seen in this cerebellopontine angle meningioma, characterizing the typical "mother-in-law sign."
-
This angiogram demonstrates successful embolization of this cerebellopontine angle meningioma prior to surgery, via embolization of the right occipital artery with polyvinyl alcohol particles.
-
Two different cases. A, B: Computed tomography (CT) scans depict calcified meningiomas from the parietal convexity. C: Nonenhanced axial CT image shows homogeneous calcified mass attached to the right parietal bone. Soft-tissue tumor is seen at the posterior aspect of the calcification (large arrow). Other minor calcifications on the left cerebral hemisphere are caused by a parasitic disease. D: Coronal T2-weighted magnetic resonance image demonstrates calcium deposit (star) surrounded by solid tissue (small arrow); edema is not seen in this case.
-
Parasagittal meningioma. A: Nonenhanced sagittal T1-weighted magnetic resonance image (MRI) shows a solid dural isointense mass with bone invasion and compression against the parietal cortex. B: Contrast-enhanced sagittal T1-weighted MRI demonstrates partially intense enhancement of the tumor. C: Coronal T2-weighted image shows isointense mass meaning hard tissue. This finding is observed on fibroblastic meningiomas. D: Contrast-enhanced T1-weighted axial MRI shows hyperintense image located within the bony marrow.
-
A: Noncontrast angio-magnetic resonance image (MRI) on lateral view demonstrates occluded superior sagittal sinus due to meningioma invasion. B: MRI reconstruction shows sagittal venous obstruction and 3-dimensional (3-D) appearance of the tumor.
-
Multiple meningiomas. A: Sagittal T1-weighted magnetic resonance image (MRI) demonstrates posterior fossa and parietal meningiomas. B: Gadolinium enhancement on sagittal T1-weighted MRI shows intense enhancing of the masses. C: T2-weighted coronal MRI shows stable hypointense appearance of the posterior mass after endovascular embolization.
-
Malignant and multiple meningiomas. A 47-year-old white male underwent gamma knife surgery due to left convexity meningioma, followed by microsurgical removal of the tumor. A, B: Four years later, MRI showed a stable residual parietal/occipital mass. The left sigmoid sinus is occluded. C, D: One small right frontal meningioma also underwent radiosurgery at the same time. Edema and intense enhancing after gadolinium injection is demonstrated.
-
A-D: Coronal T2-weighted and enhanced T1-weighted magnetic resonance images demonstrate quick growth of a convexity mass toward the tentorium and the petrous bone. This bone structure is filled with liquid in its inferior aspect. Surgical biopsy reported "atypical meningioma."
-
Coronal computed tomography scan. This bone window shows petrous bone destruction and partial lack of bone plane after surgical removal of the tumor.
-
Digital subtraction angiography. A, B: Left external carotid artery shows early and delayed stain of the mass through middle meningeal and superficial temporal arteries. C: Occipital artery. D: The branches were embolized before the surgical procedure. The tumor was partially removed due to cranial base involvement.
-
Frontal meningioma. A, B: Slow growth and surrounding edema is seen on magnetic resonance imaging (MRI) control of this tumor. Coronal, enhanced-T1 weighted and fluid attenuation inversion recovery (FLAIR) sequences are shown. C, D: Digital angiography. Right middle meningeal branch demonstrates feeding of the tumor. It was not embolized.
-
A: 3-dimensional (3-D)-enhanced T1-weighted magnetic resonance image (MRI) image shows residual meningioma at the cranial base after second surgical removal. B: Coronal T2-weighted MRI shows intense edema surrounding the frontal mass. C: 3-D image on enhanced T1-weighted MRI demonstrates frontal meningioma underlying the orbital right sulcus. D: Gadolinium-enhanced, axial T1-weighted image shows 1 of the 3 focal hyperintense masses discovered only on this sequence. Brain metastases from meningioma have not been proved.
-
Histopathologic report described a meningothelial-like neoplasm proliferation that shows hypercellularity, a prominent nucleolus, regions of necrosis, occluded veins and arteries, and dense chromatin. The neoformation reaches adjacent bone structures. Histopathologic diagnosis: left temporal mass compatible with an atypical meningioma meningothelial neoplasm.
-
Computed tomography (CT) scanning is the imaging technique most commonly used to evaluate bone changes and calcium in meningiomas. Plain radiography can show calcium in 20% of patients. This image demonstrates bone changes on a coronal CT scan with bone window settings.
-
Embolization may be the only treatment required in older or high-risk patients. Meningeal vessels from the internal carotid artery should supply the tumor. Mass effect should persist after embolization of the middle meningeal artery.
-
Meningiomas have the same enhancement appearance on computed tomography (CT) scans and magnetic resonance images (MRIs) after the injection of contrast material. Meningiomas of the left parietal convexity are shown on axial CT scans, and meningiomas of the left parietal midline are shown on MRIs. Intense enhancement is seen.
-
Magnetic resonance imaging (MRI) is the best cross-sectional imaging modality for assessing soft tissues and thus brain tumors, including specifically meningiomas. On coronal T2-weighted MRIs, parasagittal meningiomas are isointense and inhomogeneous tumors and have a harder character (fibroblastic meningioma).
-
Lateral skull projection of a bone scan shows a small focus of increased uptake that overlying the mid skull. Subsequent CT demonstrated a small right posterior frontal meningioma. The uptake on bone scan is thought to be secondary to calcium deposition factors as well as the presence/absence of a vascular pool.
-
After identification on plain radiograph, this calcified intracranial mass was further investigated with CT. This transverse axial CT at the level of the superior border of the orbits demonstrates a cribriform plate meningioma.
-
Transverse axial and coronal CT images show a large left parieto-occipital calcified meningioma.
-
3-D reconstructions are shown, characterizing a left parieto-occipital meningioma.
-
Lateral scout radiograph shows a large densely calcified intracranial mass. This scout image was for a subsequent CT that demonstrates typical features of a meningioma.
-
Transverse axial CT without and with contrast demonstrates the large calcified meningioma that was seen radiographically on the scout image.
-
Transverse axial CT at the level of the centrum semiovale on brain and bone windows illustrates a small right posterior frontal meningioma that was detected on bone scan. Bone windows illustrate typical meningioma features of hyperostosis and cortical irregularity underlying the mass. Partial calcification of the meningioma is also noted.
-
Frontal skull radiograph illustrates a calcified mass overlying the frontal sinuses. Lateral skull radiograph localizes the mass to be arising superior to the cribriform plate. Although a meningioma could be suspected, this finding is not specific and this intracranial mass was correctly further investigated with CT.
-
MRI images with the following sequences: axial T2, axial T2, coronal FLAIR, and sagittal T1. A large left-sided meningioma shows a spoke-wheel pattern within an extra-axial mass with surrounding edema.
-
Transverse axial CT on brain and bone windows shows a large intraosseous meningioma. The findings can range from osteolysis to osteosclerosis and are non-specific. Intraosseous meningiomas represent less than 1% of osseous tumors.
-
MRI with the following sequences: axial T2, coronal T1 post gadolinium administration, and MR spectroscopy. Findings of this large meningioma include CSF encompassing the mass, a classic "CSF cleft sign," confirming an extra-axial location. Additional features include significant mass effect with effacement of the left lateral ventricle. Note the avid homogeneous enhancement after gadolinium is administered. MRS shows elevated choline and low NAA as classic features.
-
MRI with the following sequences: axial T1 post gadolinium administration, coronal T1 post gadolinium, sagittal T1, and MR spectroscopy. This meningioma shows avid enhancement and invasion into the superior sagittal sinus. MRS shows elevated choline and low NAA as typical meningioma features.
-
Transverse axial CT through the level of the posterior fossa without and with contrast, demonstrates a midline enhancing meningioma compressing the fourth ventricle. This is an atypical location for meningioma, and the mass was worked up further with MRI.
-
MRI images with the following sequences: axial T2, coronal FLAIR, coronal T1, coronal T1 post gadolinium administration, sagittal T1 post gadolinium, and MR spectroscopy. This MRI characterizes the posterior fossa meningioma to be within the cisterna magna, exerting mass effect with superior displacement of the cerebellum. Avid enhancement is seen after gadolinium is administered. MRS features include elevated choline and relatively absent NAA.
-
Diffusion weighted MRI of the posterior fossa meningioma demonstrates mildly increased signal, in keeping with mild diffusion restriction.
-
Axial T2 weighted MRI image shows a midline frontal meningioma. High T2 signal rim surrounding the mass is consistent with CSF fluid, confirming the extra-axial location. This is a classic "CSF cleft sign" of extra-axial tumors, such as meningiomas.
-
Subsequent MRI of the previous CT with the following sequences: axial T1 post gadolinium adminsitration and axial T2 sequences. This again shows a large midline frontal meningioma with a spoke-wheel pattern.
-
Transverse axial CT without and with contrast shows a spoke-wheel pattern within this avidly enhancing meningioma. Although this pattern is typically seen angiographically, it can also be noted on cross-sectional imaging.
-
Multisequence MR images, including axial T2 and axial T1 post-gadolinium, demonstrate a large right temporal meningioma with a spoke-wheel pattern, local mass effect, surrounding edema, and underlying hyperostosis.
-
MRI of the brain with the following sequences: axial T2, coronal T2, coronal FLAIR, and coronal T1 post gadolinium administration. Shown is a left frontal meningioma with a spoke-wheel pattern, underlying hyperostosis of the calvarium, and surrounding parenchymal edema.
-
This MR spectroscopy of the previous MRI demonstrates elevated choline and low NAA levels, typical of meningiomas. Additional characteristic meningioma MRS features include increased alanine and glutamate-glutamine complex and decreased creatine. Elevated signal intensities, specifically at 3.8 ppm (glutamine) and 1.48 ppm (alanine), have been reported. Lipid and lactate levels remain controversial in meningioma evaluation.
-
An MR angiogram was performed on the previous case, with the following sequences: MRA through the level of the middle cerebral arteries, MRA through the level of the petrous segment of the internal carotid arteries, collapsed MRA, and MRA projection. These images demonstrate an additional finding of the large right temporal meningioma supplied by the middle meningeal artery (a branch off the external carotid arterial system). Identification of this finding is important for presurgical consideration of embolization.