Practice Essentials
Meconium is the material found in the intestine of a newborn. It consists of succus entericus, which is made up of bile salts, bile acids, and debris shed from the intestinal mucosa during intrauterine life. It is normally evacuated within 6 hours after birth or sooner in utero as the result of a vagal response to perinatal stress. Meconium ileus (MI) is often the first manifestation of cystic fibrosis (CF) and occurs in approximately 20% of patients with diagnosed CF. [1] The inspissated meconium obstructs the small intestine at the level of the terminal ileum. The prognosis for infants presenting with both simple and complicated meconium ileus has improved with the advancement of both nonoperative and operative treatments, along with good nutritional support and better treatment of bacterial infections. If left untreated, the prognosis is poor. [2]
Once MI is detected prenatally, the clinician should formulate treatment strategies that can prevent the progression of simple MI to complex MI. [2]
Radiography is the preferred examination for evaluating cases of meconium ileus, meconium peritonitis, meconium ileus–equivalent syndrome, and meconium plug syndrome. [3] Normally, meconium is invisible on a radiograph. Occasionally, it has a mottled appearance on abdominal radiographs during the first 2 days of life.
Fetal magnetic resonance imaging (MRI) should be included in the diagnostic algorithm of any pregnancy where fetal bowel obstruction is suspected, to better risk-stratify patients. [4]
By convention, 4 gastrointestinal conditions include the term meconium in their names: meconium ileus, meconium peritonitis, meconium ileus–equivalent syndrome, and meconium plug syndrome. [5, 6, 7, 8, 9, 10, 11, 12]
Meconium ileus
Meconium ileus (MI) is defined as an intestinal obstruction caused by impaction of inspissated meconium in the terminal ileum. [13]
In MI, low or distal intestinal obstruction results from impaction of thick, tenacious meconium in the distal small bowel. Complications such as ileal atresia or stenosis, ileal perforation, meconium peritonitis, and volvulus with or without pseudocyst formation can occur in association with MI. [5, 6, 10, 14, 15, 16, 17]
Proper evaluation of the patient, careful application of principles of conservative management, and timely surgical intervention may yield satisfactory results. [13]
Meconium peritonitis
Meconium peritonitis (MP) is a rare fetal disease that needs to be urgently identified for surgical intervention. Fetuses with bowel dilatation and micro-colorectum on MRI may need postpartum surgical intervention. Infants with only a small amount of ascites and slight bowel distention are likely to receive conservative treatment. [18]
Meconium peritonitis may be incidentally detected on abdominal radiographs. Clinically, patients may present with bowel obstruction caused by fibroadhesive bands, which are produced by the inflammatory peritoneal reaction. The bowel itself may be intact with healed perforation, but bowel atresias are often associated. If the processus vaginalis is patent at the time that perforation occurs, calcification or hernias may involve the scrotum. Ascites may also be present. [9, 11, 12, 17]
Imaging findings that predict the need for surgery include intestinal obstruction, ascites, volvulus, and pneumoperitoneum. Neonates with meconium pseudocysts do not require surgery if these cysts are not associated with the findings described here. Those with diffuse peritoneal calcification as an isolated finding can be successfully treated nonoperatively. [19]
When the extruded meconium becomes walled off, it can form a meconium pseudocyst—a cystic, rim-calcified mass. [12]
Meconium ileus–equivalent syndrome
“Meconium ileus–equivalent syndrome” is the term applied to a partial small-bowel obstruction in an older patient with known CF. Although the bowel gas pattern may resemble that of MI, these findings are not due to meconium, which is present only in the newborn. [20]
This condition is important, as it can be the presenting feature of CF during childhood and even in early adult life. Moreover, operative mortality and morbidity rates are high. Recurrent bowel obstruction (which is often correlated with poor compliance with medication for CF) may manifest as recurrent colicky abdominal pain, often in the right upper quadrant. In the older infant or child, chronic constipation can be a problem and intestinal obstruction can occur secondary to fecal impaction. Patients may also present with intussusceptions. [21, 22]
Meconium plug syndrome
“Meconium plug syndrome” refers to a functional colonic obstruction in a newborn due to an obstructing meconium plug. It is usually transient and affects the left colon, with meconium plugging of the bowel distal to this segment. In this situation, it is also termed the “small left-colon syndrome.” [23]
Meconium plug syndrome may have higher prevalence with maternal diabetes and may be associated with CF. [23]
"Functional colonic obstruction in the full-term neonate" is another name for meconium plug syndrome. Although this abnormality is most often found in term infants, Mees et al reported that 3 of their 4 patients were premature. Most infants with this form of colonic obstruction present within the first 24 to 36 hours of life. Findings include abdominal distention, bilious vomiting, and failure to initiate normal passage of meconium. [24, 25]
Radiography
Radiography is the preferred examination for evaluating cases of meconium ileus, meconium peritonitis, meconium ileus–equivalent syndrome, and meconium plug syndrome. [3, 10, 25]
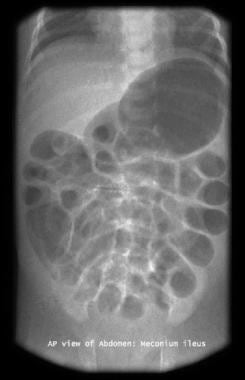
(See the images below.)
Contrast enema examination can help in differentiating meconium plug syndrome from meconium ileus or ileal atresia. In these latter conditions, microcolon is seen, and only occasionally does an infant with MI have a picture similar to that seen in an infant with meconium plug syndrome. [26]
(See the images below.)
 Gastrografin enema study shows filling defects in the terminal ileum and cecum. Also note the microcolon (transverse and descending colon).
Gastrografin enema study shows filling defects in the terminal ileum and cecum. Also note the microcolon (transverse and descending colon).
 Enema study shows microcolon and contrast material outlining a terminal ileum packed with (meconium) filling defects.
Enema study shows microcolon and contrast material outlining a terminal ileum packed with (meconium) filling defects.
Meconium ileus
Plain abdominal radiographs frequently reveal a low small-bowel obstruction with numerous air-filled loops of bowel. Although plain imaging findings may suggest the diagnosis, with or without a family history of CF, contrast enema examination of the colon is required to confirm the diagnosis of MI. [7, 21, 27]
Water-soluble contrast material is typically used, as are a variety of water-soluble contrast agents. Shin and Jeon reported that ultrasound-guided Gastrografin enema at bedside was effective and safe for very low birth weight infants as first-line treatment to relieve meconium-related ileus. They concluded that with this treatment, unnecessary emergent operation can be avoided in preterm infants, who have high postoperative morbidity and mortality, as can transport of small preterm infants to the fluoroscopy suite. [28]
The Cystic Fibrosis Foundation Consensus Conference on GI disorders concluded that no scientific evidence suggests that a hyperosmolar Gastrografin enema is any better than an iso-osmolar or hypo-osmolar enema. However, opinion remains divided on this topic, and Gastrografin when diluted appropriately is used safely by very experienced pediatric radiologists.
Other nonionic contrast agents (eg, Hypaque, Omnipaque) are preferred by many radiologists and involve less risk of dehydration or colitis. Because of potential fluid shifts, hypovolemia may occur; therefore, assurance of adequate hydration and electrolyte balance before, during, and after the procedure is essential. This monitoring should prevent significant fluid shifts. If perforation of bowel and leak of contrast or Gastrografin into the peritoneum occurs, more rapid fluid shifts may result. Close monitoring by a neonatologist is recommended.
Acetylcysteine (a mucolytic) can be mixed with the enema to aid the passage of very sticky meconium, but the efficacy of this is not known.
Because of tenacious meconium and abnormal mucous gland secretion, air-fluid levels often are not apparent. However, images in some infants may reveal air-fluid levels, especially in those with complications such as volvulus and stenosis or atresia.
Although absence of air-fluid levels strongly suggests meconium ileus, the presence of air-fluid levels does not exclude it. In some cases of MI, distention of the obstructed small bowel can be enormous and findings can be easily misinterpreted as distal colonic distention. In other cases, a so-called soap-bubble effect of gas mixed with meconium may be seen.
Although this soap-bubble effect is not pathognomonic of the condition, it is commonly seen with MI. However, it can also be seen with ileal atresia, colonic atresia, Hirschsprung disease, and meconium plug syndrome.
A contrast enema study typically demonstrates microcolon, which reflects underused bowel. A microcolon can be due to other etiologies besides CF such as ileal atresia or another complete intrauterine obstruction of the distal small bowel. However, when contrast agent refluxes into the small bowel, meconium pellets distending the distal ileum are usually identified and the diagnosis of MI is confirmed.
Meconium peritonitis
Meconium peritonitis may be incidentally detected on abdominal radiographs. The extruded meconium may or may not become calcified, and when no calcification is present, the radiograph may only suggest fluid in the abdomen. Contrast enema examination can help in differentiating meconium plug syndrome from MI or ileal atresia.
In some cases, fluid and meconium can pass into the chest, presumably through congenital communications, resulting in meconium thorax. When calcification is seen, the diagnosis can usually be confirmed. This calcification can be amorphous and irregular or curvilinear, with the latter suggesting cystic loculation or coating of the peritoneum. The term "cystic" or "pseudocystic" meconium peritonitis has been applied to this finding.
It is uncommon to encounter an older child with residual calcifications.
Only occasionally does an infant with MI have a picture similar to that seen in an infant with meconium plug syndrome.
Meconium ileus–equivalent syndrome
Plain abdominal images show a mottled appearance (which may simulate meconium) in dilated loops of small bowel. Other plain imaging findings include a bubbly, granular appearance, predominantly on the right side of the abdomen, with dilated small bowel and fluid levels due to small-bowel obstruction.
Water-soluble contrast enemas are often helpful in excluding other possible causes of symptoms and can be used to treat patients with this condition. If the diagnosis can be made radiologically, conservative medical treatment should be pursued vigorously, and surgery should be undertaken only if it is unavoidable. [22]
Meconium plug syndrome
Meconium plug and small left-colon syndromes are diagnosed radiologically, and contrast enema examination is required. Plain images are nonspecific and usually show findings of a low small-bowel obstruction. Erect abdominal radiographs, albeit seldom necessary in the newborn, show a paucity of air-fluid levels, and, in most cases, no gas is seen in the colon.
Water-soluble contrast enemas can be curative with the passage of meconium.
If air is introduced into the rectum from below (eg, on rectal examination), rectal gas may be visualized. In this setting, meconium in the rectum can erroneously suggest a small presacral mass. However, if air entirely surrounds the meconium mass, it will outline the contour of the mass, suggesting the correct diagnosis.
If peristalsis forces gas from the small bowel into the colon, and if the gas mixes with meconium, a granular or bubbly appearance mimicking the findings of pneumatosis cystoides intestinalis and necrotizing enterocolitis (NEC) results. If a bubbly pattern is seen within the first 12 hours of life, meconium plug syndrome should be considered, but if it is visible after 12 to 18 hours, NEC is more likely. NEC typically occurs in preterm infants.
Contrast enema examination shows a characteristic appearance of the colon, with contrast material outlining the solid column of inspissated meconium and the wall of the colon for a double-contrast effect.
After meconium is passed, the portion of the colon from which it was evacuated may appear narrowed, and a transition zone mimicking that seen in Hirschsprung disease may be noted.
In any of these cases, meconium proximal to the apparent transition zone may take the form of a solid, cylindrical mass extending to the cecum, or lumps of solid meconium may be scattered throughout the colon.
For patients with intermediate findings, individual assessment is most important.
The small, contracted portion of the descending colon in these infants has led to the term "neonatal small left-colon syndrome."
False positives/negatives
Differentiating Hirschsprung disease from meconium plug or small left-colon syndrome can be a problem, and one must completely exclude Hirschsprung disease before either of these diagnoses is confirmed. [8]
Initial clinical and radiologic findings may be similar, but infants with Hirschsprung disease invariably return with either constipation or diarrhea. Once treated, those with meconium plug or small left-colon syndrome remain healthy. Plain images in infants with Hirschsprung disease are more likely to show numerous air-fluid levels on the erect view. During an enema, abnormal contractions with bowel wall irregularity may be seen in the narrowed, aganglionic bowel of Hirschsprung disease, but the bowel wall typically has a smooth contour in the meconium plug setting.
Ultrasonography
Fetal MRI is used to assess abnormalities in fetal meconium patterns after ultrasonography. Bowel anomalies are a significant cause of neonatal morbidity. With care, these results can be used in clinical practice to aid diagnosis of bowel pathology. [29]
Meconium ileus
Ultrasonographic signs of meconium ileus include enlarged bowel loops at 17 to 18 weeks' gestational age, or a mass with proximal bowel distention, which is suggestive of cystic meconium peritonitis on prenatal sonography. [6, 17]
Meconium peritonitis
Ultrasound is seldom necessary for evaluation of meconium peritonitis, as findings on plain radiographs are usually diagnostic.
Calcified meconium can be seen during in utero sonography. Ultrasonography may be useful after birth, when cystic masses are present and often appear circumscribed and heterogeneous.
Fluid (sonolucent areas) may be seen in the cyst, but usually, increased echogenicity resulting from debris and calcifications is seen. The wall of the cyst may be thin or thick, and one may note loops of fluid-filled bowel bound to the matrix of associated adhesions.
With free-floating meconium in the abdomen, multiple speckled echoes are seen. These produce a snowstorm configuration.
Calcifications in the scrotum produce echogenic masses.
Prenatal ultrasound manifestations of fetal meconium peritonitis are diverse, and the different grades of prenatal ultrasound manifestations can provide important information for treatment of perinatal infants. [30]
Zangheri et al created the following classification system related to perinatal outcomes [12, 31] :
-
Grade 0: isolated intra-abdominal calcifications (IAC)
-
Grade I: IAC and 1 of the following: ascites, pseudocyst, or bowel dilatation
-
Grade II: IAC and 2 of the following: ascites, pseudocyst, or bowel dilatation
-
Grade III: all of the above (IAC, ascites, pseudocyst, and bowel dilatation)
Meconium ileus–equivalent syndrome
Rare cases of intussusception occurring as a complication of cystic fibrosis may be easily diagnosed with ultrasonography.
-
Abdominal radiograph shows low intestinal obstruction.
-
Abdominal radiograph shows low intestinal obstruction.
-
Gastrografin enema study shows filling defects in the terminal ileum and cecum. Also note the microcolon (transverse and descending colon).
-
Enema study shows microcolon and contrast material outlining a terminal ileum packed with (meconium) filling defects.
-
Long, cylindrical filling defect in the descending and sigmoid colon.