Practice Essentials
Undifferentiated pleomorphic sarcoma (UPS), previously called malignant fibrous histiocytoma (MFH), is a soft tissue sarcoma (STS) that can occur anywhere in the body, but it usually occurs in the extremities (especially the thighs) or back of the abdomen (see the image below). Approximately 15% of undifferentiated pleomorphic sarcomas arise in the abdomen and pelvis. [1] UPS often grows quickly and spreads to other parts of the body, including the lungs.
Undifferentiated pleomorphic sarcoma usually occurs in older adults, and men account for two thirds of cases. UPS is the most common sarcoma to develop at sites of prior irradiation. Investigators have shown that most patients have received a radiation dose of 50 Gy or more, and the median time interval between radiation exposure and the development of a radiation-associated sarcoma is approximately 10 years. Undifferentiated pleomorphic sarcoma may also arise at sites of chronic ulceration. [1]
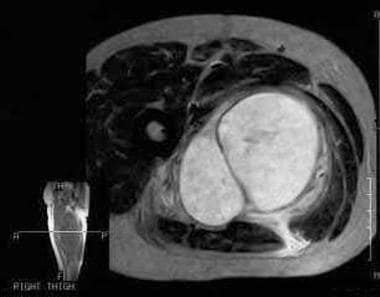
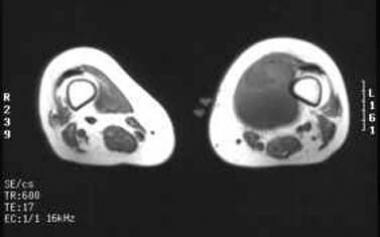
 CT reveals a mass within the anterior compartment musculature of the left thigh. The malignant fibrous histiocytoma is only slightly hypodense to muscle and conceivably could be overlooked.
CT reveals a mass within the anterior compartment musculature of the left thigh. The malignant fibrous histiocytoma is only slightly hypodense to muscle and conceivably could be overlooked.
The World Health Organization (WHO) has published a classification system for tumors of the soft tissue and bone, which includes detailed cytogenetic and molecular data. Undifferentiated/unclassified sarcomas include the following subtypes [2] :
-
Undifferentiated spindle cell sarcoma
-
Undifferentiated pleomorphic sarcoma (previously classified as malignant fibrous histiocytoma)
-
Undifferentiated round cell sarcoma
-
Undifferentiated epithelioid sarcoma
-
Undifferentiated sarcoma not otherwise specified
Historically, the term malignant fibrous histiocytoma (MFH) was applied to pleomorphic spindle cell neoplasms with fibroblastic and histiocytic differentiation. However, the majority of tumors within this classification did not show any evidence of histiocytotic differentiation, and many were found to be other types of poorly differentiated tumors. The small minority of tumors for which the term MFH was most representative are now classified as undifferentiated high-grade pleomorphic sarcoma.
Tumors are further classified by WHO as benign, intermediate, or malignant, and intermediate tumors are designated as either locally aggressive or rarely metastasizing. [2]
UPS has been reported to occur in the lungs, liver, kidneys, bladder, scrotum, vas deferens, heart, aorta, stomach, small intestine, orbit, CNS, paraspinal area, dura mater, facial sinuses, nasal cavity, oral cavity, nasopharynx, and soft tissues of the neck. [3]
The most common clinical presentation is an enlarging painless soft-tissue mass in the thigh, typically 5-10 cm in diameter. The majority of tumors are intramuscular. At gross pathologic examination, the lesion is multilobulated, with necrosis, degeneration, or hemorrhage on the cut surface. In some tumors, extensive hemorrhage can be present. Although the border of the tumor may appear well defined at gross pathologic examination, microscopic spread along muscle fibers and fascial planes is often present. Microscopically, tumor cells with variably pleomorphic nuclei are characteristic. There is no characteristic immunohistochemical profile. Immunohistochemical analysis is used to help exclude other tumors that may have a pleomorphic appearance. [1]
Rare signs and symptoms include episodic hypoglycemia and rapid tumor enlargement during pregnancy. Additionally, UPS has been associated with hematopoietic diseases such as non-Hodgkin lymphoma, Hodgkin lymphoma, multiple myeloma, and malignant histiocytosis.
Retroperitoneal tumors may present with constitutional symptoms, including fever, malaise, and weight loss. The tumor is often large at presentation and may cause displacement of the bowel, kidney, ureter, and/or bladder.
UPS may also occur secondary to radiation exposure and shrapnel injury and may be seen adjacent to metallic fixation devices, including total joint prostheses. Early and complete surgical removal using wide or radical resection is indicated because of the aggressive nature of the tumor.
Imaging Guidelines
The National Comprehensive Cancer Network (NCCN) clinical practice guidelines for STS of the extremities, superficial trunk, or head and neck include the following imaging recommendations [4] :
-
Provide adequate imaging of primary tumor for all lesions with a reasonable chance of being malignant.
-
Imaging studies should include cross-sectional imaging magnetic resonance imaging (MRI) with and without contrast to provide details about the size and contiguity to nearby visceral structures and neurovascular landmarks. The addition of computed tomography (CT) scanning with contrast may be needed.
-
Other studies such as angiography and plain radiography may be warranted in individual situations.
-
For chest imaging, CT without contrast is preferred,
-
PET/CT scan may be useful in staging, prognostication, and grading.
-
For retroperitoneal/intra-abdominal STS, a chest/abdominal/pelvic CT scan is recommended, with or without an abdominal/pelvic MRI.
In concurrence with NCCN, the ESMO–EURACAN (European Society for Medical Oncology–European Reference Network for rare adult solid cancers) clinical practice guidelines on STSs recommend MRI as the main imaging modality in the extremities, pelvis, and trunk. Standard radiographs may be useful to rule out a bone tumor, to detect bone erosion with a risk of fracture, and to show calcifications. CT is used in calcified lesions to rule out a myositis ossificans and in retroperitoneal tumors, where the performance is identical to MRI. Ultrasound may be the first exam, but it should be followed by CT or MRI. [5]
Sarcoma specialists from the United Kingdom, including members of the British Sarcoma Group and NHS England Sarcoma Clinical Reference Group, also issued guidelines on management of STS. Imaging recommendations include [6] :
-
Any patient with a soft tissue mass that is increasing in size or is >5 cm, whether or not painful, should be referred either for an urgent ultrasound scan or directly to a sarcoma diagnostic center.
-
If the ultrasound scan does not definitively confirm benign pathology, the patient should be referred for further investigation on an urgent suspected cancer referral pathway.
-
Ultrasound scan by a musculoskeletal radiologist should be considered as the first-line investigation and may be supplemented by ultrasound-guided core biopsy.
-
MRI and core needle biopsy are recommended prior to definitive surgery.
-
Imaging of the thorax by CT scan for lung metastases should be done before radical treatment; further staging may be considered depending on subtype and location of the sarcoma.
The Trans-Atlantic Retroperitoneal Sarcoma Working Group was established to address challenging management issues encountered when caring for patients with retroperitoneal soft tissue sarcomas (RPS). Their imaging recommendations include the following [7] :
-
Review of cross-sectional imaging by a dedicated tumor board is required.
-
CT of the chest, abdomen, and pelvis with intravenous contrast is the preferred imaging modality. MRI may be a useful ancillary modality in selected cases to define extent of adjacent organ/structure involvement that is not clear on CT but is not required in most cases.
-
MRI is an option for patients with contrast allergy, for pelvic tumors, or for cases in which detailed anatomic information (eg, sciatic foramen) is required.
-
PET scan is rarely indicated; it may be indicated if the extent of active abdominal disease is difficult to evaluate and/or if there is uncertainty about different growth characteristics in multifocal lesions that would alter management
The American College of Radiology (ACR) Appropriateness Criteria for soft-tissue masses include the following recommendations [8] :
-
The initial imaging study for a superficial or palpable soft-tissue mass should be radiographs.
-
US is equally appropriate for small lesions that are superficial to the deep fascia.
-
For deep masses or lesions in areas difficult to evaluate radiographically (ie, groin, paraspinal area, deep soft tissues of the hands and feet, or flank), radiographs are also usually appropriate.
-
If the initial evaluation of soft-tissue masses is nondiagnostic, further evaluation with MRI without and/or with IV contrast is usually appropriate.
-
In patients presenting with spontaneous hemorrhage or suspicion of a vascular mass, if the initial evaluation is nondiagnostic, further evaluation with either MRI without and with IV contrast or CT without and with IV contrast is usually appropriate.
-
If the initial evaluation of a soft-tissue mass is nondiagnostic in patients who are non–MRI compatible or who have metal limiting MRI evaluation, CT with IV contrast or CT without and with IV contrast is usually appropriate as the next imaging study.
For a full summary of guidelines recommendations, see Soft Tissue Sarcoma Guidelines.
Preferred examination
As with other soft-tissue tumors, MRI is the imaging method of choice because of its ability to provide superior contrast between tumor and muscle, excellent definition of surrounding anatomy, and ease of imaging in multiple planes. [9, 10]
(UPSs are displayed in the images below.)
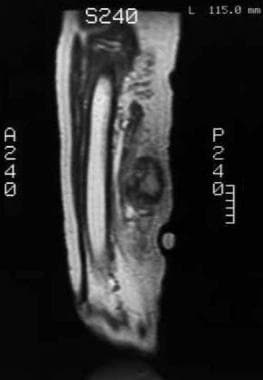
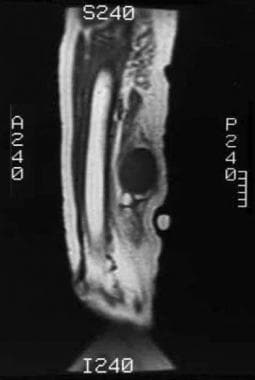 Noninfused T1-weighted MRI reveals a low signal intensity mass posterior to the femoral diaphysis (same patient as in the previous image).
Noninfused T1-weighted MRI reveals a low signal intensity mass posterior to the femoral diaphysis (same patient as in the previous image).
 T1-weighted MRI obtained following intravenous gadolinium administration reveals inhomogeneous enhancement of the soft tissue mass (same patient as in the previous image).
T1-weighted MRI obtained following intravenous gadolinium administration reveals inhomogeneous enhancement of the soft tissue mass (same patient as in the previous image).
Although MRI is typically best suited for defining the anatomy of the tumor and its surrounding structures, the signal characteristics of pleomorphic sarcoma, as well as the true histologic nature of the tumor or other soft-tissue masses, often cannot be ascertained by imaging alone, with few exceptions (eg, lipoma). Furthermore, patients with claustrophobia or cardiac pacemakers and aneurysm clips may not be able to undergo examination with MRI. In these patients, axial CT scanning may be performed. CT scanning can provide adequate information regarding the location and gross extent of the mass, although the contrast between tumor and muscle is often less than that seen with MRI. CT scanning is also useful for evaluation of calcifications. [11, 12]
No single imaging technique can provide a specific histologic diagnosis of pleomorphic sarcoma, and biopsy is usually necessary. If the radiologist is asked to perform a biopsy on a potentially malignant soft-tissue mass, the orthopedic surgeon resecting the mass must be consulted first. With certain tumors, the biopsy tract must be removed with the mass; a presurgical image-guided biopsy performed without appropriate orthopedic consultation may result in more extensive surgery (including amputation) than would have been necessary otherwise.
See Soft-Tissue Sarcomas: What You Need to Know, a Critical Images slideshow, to help identify and treat some of these malignant tumors of mesenchymal origin.
Radiography
Radiographs may reveal a nonspecific soft-tissue mass (see the image below), often greater than 5 cm in diameter. Deep intramuscular tumors often lie adjacent to the diaphysis of a long bone.
 Radiograph demonstrates a soft tissue mass posterior to the femoral diaphysis. Although not appreciated on the radiograph, a component of the mass extends inferiorly and contains a small cluster of calcifications (within circle).
Radiograph demonstrates a soft tissue mass posterior to the femoral diaphysis. Although not appreciated on the radiograph, a component of the mass extends inferiorly and contains a small cluster of calcifications (within circle).
Secondary osseous involvement, including periosteal reaction, cortical erosion, and pathologic fracture, is uncommon but suggestive of a malignant soft-tissue sarcoma.
Calcification or ossification can be detected in 5-20% of patients. Calcifications within the tumor may be punctate, curvilinear, and/or poorly defined.
Heterotopic bone formation may be present in the periphery of the mass.
Computed Tomography
On CT images, UPS lesions are well-circumscribed, multinodular, or infiltrating masses of soft-tissue attenuation. Undifferentiated pleomorphic sarcomas are often large at the time of diagnosis and invade adjacent anatomic structures. Centrally within the tumor, areas of low-attenuation necrosis, hemorrhage, or myxoid change can be seen. The tumor may appear cystic with a rim of peripheral enhancement when marked intralesional hemorrhage is present. [1]
Calcification from osseous or chondroid metaplasia occurs in approximately 16% of cases. Calcifications may be small and punctate in a speckled pattern or coarse and chunky. After administration of intravenous contrast material, the enhancement pattern is variable, although regions of marked contrast enhancement and large intratumoral vessels may be seen. Hemoperitoneum from tumoral hemorrhage has been reported. [1]
Fat attenuation is not observed in the tumors; this fact can be useful in distinguishing undifferentiated pleomorphic sarcoma from some well-differentiated liposarcomas. [13]
Retroperitoneal tumors manifest as heterogeneous masses with areas of hemorrhage and/or necrosis and occasionally focal or diffuse coarse calcifications (approximately 10%); the tumors may invade the abdominal musculature but do not invade the renal veins or inferior vena cava. [12, 14, 15]
(See the images below.)
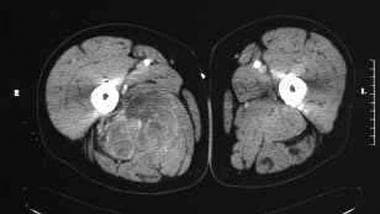 Transverse CT image following enhancement with intravenous contrast shows a heterogeneous and mildly enhancing soft tissue mass in the posteromedial right thigh.
Transverse CT image following enhancement with intravenous contrast shows a heterogeneous and mildly enhancing soft tissue mass in the posteromedial right thigh.
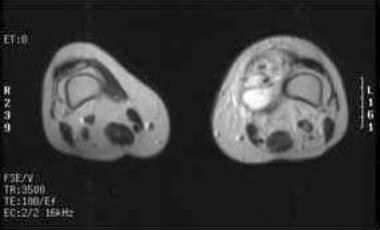
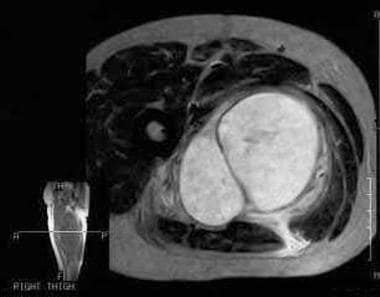 T2-weighted MRI reveals a hyperintense mass within the posteromedial right thigh (same patient as in the previous image). The mass proved to be a malignant fibrous histiocytoma.
T2-weighted MRI reveals a hyperintense mass within the posteromedial right thigh (same patient as in the previous image). The mass proved to be a malignant fibrous histiocytoma.
Magnetic Resonance Imaging
MRI typically reveals an intramuscular mass with heterogeneous signal intensity on all pulse sequences (see the images below). As with other soft-tissue neoplasms, the signal intensity pattern is nonspecific, usually low to intermediate on T1-weighted images and intermediate to high on T2-weighted images; low signal intensity of T1-weighted images and prominent high signal intensity on T2-weighted images may be a feature of myxofibrosarcoma/myxoid MFH, reflecting the high water content of these lesions. Other findings include the following:
-
Regions of prominent fibrous tissue (high collagen content) may demonstrate low signal intensity on both T1-weighted and T2-weighted images.
-
Calcification may present as foci of low signal on both T1-weighted and T2-weighted sequences.
-
Subacute hemorrhage should be considered when regions of high signal are noted on both T1-weighted and T2-weighted images.
-
Areas of necrosis demonstrate a signal pattern similar to that of fluid.
-
As with CT, solid components of MFH typically reveal nodular and peripheral enhancement.
-
Tumor margins appear relatively well defined on MRI; a low signal intensity margin may be observed, representing a pseudocapsule.
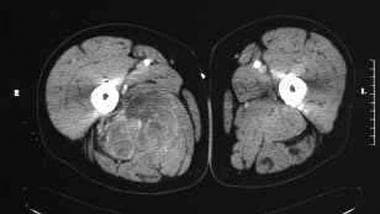 Transverse CT image following enhancement with intravenous contrast shows a heterogeneous and mildly enhancing soft tissue mass in the posteromedial right thigh.
Transverse CT image following enhancement with intravenous contrast shows a heterogeneous and mildly enhancing soft tissue mass in the posteromedial right thigh.
 T2-weighted MRI reveals a hyperintense mass within the posteromedial right thigh (same patient as in the previous image). The mass proved to be a malignant fibrous histiocytoma.
T2-weighted MRI reveals a hyperintense mass within the posteromedial right thigh (same patient as in the previous image). The mass proved to be a malignant fibrous histiocytoma.
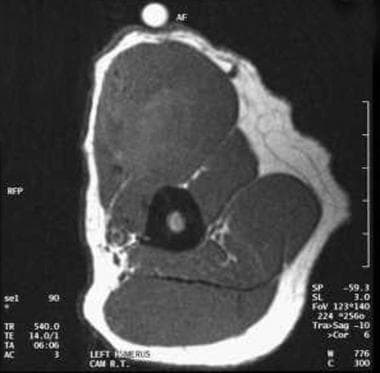 Preinfusion T1-weighted MRI reveals a large mass. Although slightly heterogeneous, the tumor is predominantly isointense to muscle.
Preinfusion T1-weighted MRI reveals a large mass. Although slightly heterogeneous, the tumor is predominantly isointense to muscle.
 T1-weighted MRI obtained following intravenous administration of gadolinium reveals circumferential enhancement of the tumor (same patient as in the previous image).
T1-weighted MRI obtained following intravenous administration of gadolinium reveals circumferential enhancement of the tumor (same patient as in the previous image).
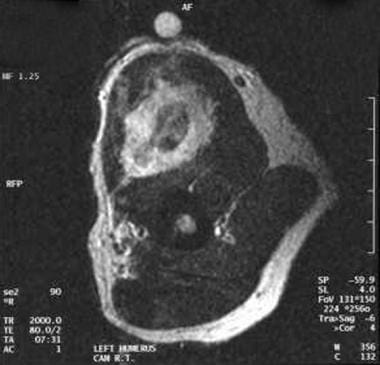 T2-weighted MRI reveals heterogeneous signal of the malignant fibrous histiocytoma (same patient as in the previous image). Central low signal intensity may be the result of old blood products.
T2-weighted MRI reveals heterogeneous signal of the malignant fibrous histiocytoma (same patient as in the previous image). Central low signal intensity may be the result of old blood products.
 T2-weighted MRI obtained following gadolinium administration reveals heterogeneous enhancement of the malignant fibrous histiocytoma.
T2-weighted MRI obtained following gadolinium administration reveals heterogeneous enhancement of the malignant fibrous histiocytoma.
 Preinfusion T1-weighted MRI of a patient with a medial left thigh mass proven at biopsy to represent a malignant fibrous histiocytoma. Although slightly heterogeneous, the mass is predominantly isointense to muscle.
Preinfusion T1-weighted MRI of a patient with a medial left thigh mass proven at biopsy to represent a malignant fibrous histiocytoma. Although slightly heterogeneous, the mass is predominantly isointense to muscle.
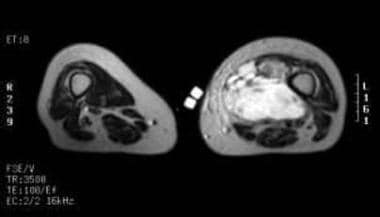 Malignant fibrous histiocytoma. T2-weighted MRI reveals predominantly increased signal intensity in the tumor mass (same patient as in the previous image).
Malignant fibrous histiocytoma. T2-weighted MRI reveals predominantly increased signal intensity in the tumor mass (same patient as in the previous image).
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
The radiologist should keep in mind that the diagnosis of UPS is made using histopathology, not imaging; however, MRI remains invaluable for delineating tumor extent.
Ultrasonography
Sonography typically reveals a well-defined heterogeneous mass that contains hyperechoic areas of cellularity and hypoechoic regions of necrosis. The appearance of tumors on ultrasound is nonspecific; however, sonography may be used to evaluate tumor volume. Retroperitoneal tumors tend to appear as hypoechoic solid masses with scattered regions of heterogeneity. [16]
(See the images below.)
 Ultrasound image demonstrates a predominantly hypoechoic mass in the thigh representing a malignant fibrous histiocytoma. Regions of hyperechogenicity likely correspond to cellular components of the tumor.
Ultrasound image demonstrates a predominantly hypoechoic mass in the thigh representing a malignant fibrous histiocytoma. Regions of hyperechogenicity likely correspond to cellular components of the tumor.
Nuclear Imaging
Technetium-99m bone scintigraphy often shows increased uptake by tumor, regardless of the presence of calcium within the tumor or invasion of adjacent bone. Hypervascular lesions show increased radionuclide uptake on both dynamic and blood pool images. The mildly increased uptake observed on static images is also probably related to hypervascularity and may be more prominent with internal calcification. Bone scans usually are not ordered to evaluate the primary tumor but may be obtained if osseous metastases are suggested. Gallium-67 scans may also demonstrate increased activity.
(See the images below.)
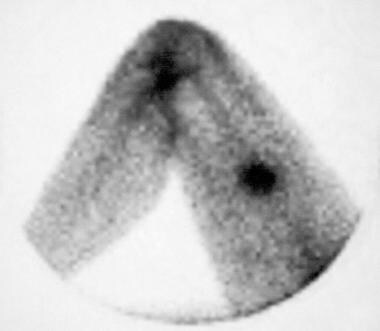
 Spot image of a technetium-99m bone scintigram (delayed phase) reveals increased radiotracer uptake in the soft tissue tumor.
Spot image of a technetium-99m bone scintigram (delayed phase) reveals increased radiotracer uptake in the soft tissue tumor.
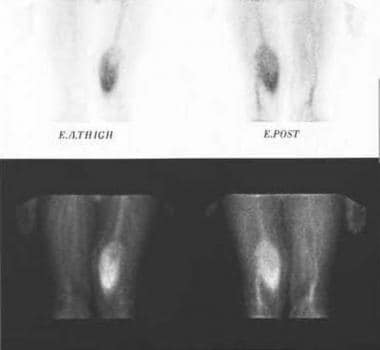
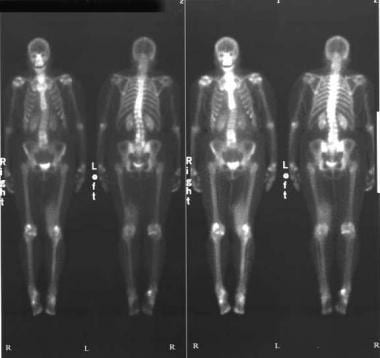 Technetium-99m bone scintigram (delayed phase) reveals increased radiotracer uptake in the left thigh.
Technetium-99m bone scintigram (delayed phase) reveals increased radiotracer uptake in the left thigh.
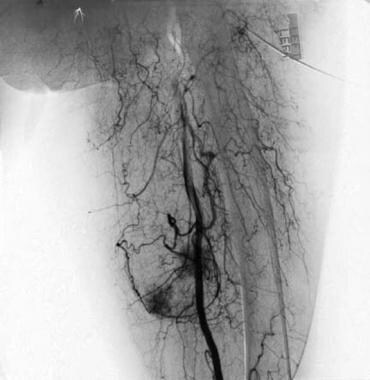
Angiography
Angiographic findings are nonspecific. The tumor may be hypovascular or, more commonly, hypervascular with early venous return (see the image below). Similarly, retroperitoneal tumors may be either hypovascular or hypervascular, with blood supply from the lumbar, celiac, iliac, renal, renal capsular, and/or inferior adrenal arteries.
-
Radiograph demonstrates a soft tissue mass posterior to the femoral diaphysis. Although not appreciated on the radiograph, a component of the mass extends inferiorly and contains a small cluster of calcifications (within circle).
-
Noninfused T1-weighted MRI reveals a low signal intensity mass posterior to the femoral diaphysis (same patient as in the previous image).
-
T1-weighted MRI obtained following intravenous gadolinium administration reveals inhomogeneous enhancement of the soft tissue mass (same patient as in the previous image).
-
Spot image of a technetium-99m bone scintigram (delayed phase) reveals increased radiotracer uptake in the soft tissue tumor.
-
Angiogram reveals tumor hypervascularity (same patient as in the previous image).
-
Transverse CT image following enhancement with intravenous contrast shows a heterogeneous and mildly enhancing soft tissue mass in the posteromedial right thigh.
-
T2-weighted MRI reveals a hyperintense mass within the posteromedial right thigh (same patient as in the previous image). The mass proved to be a malignant fibrous histiocytoma.
-
CT reveals a mass within the anterior compartment musculature of the left thigh. The malignant fibrous histiocytoma is only slightly hypodense to muscle and conceivably could be overlooked.
-
T2-weighted MRI demonstrates the tumor much more conspicuously.
-
Gallium-67 scintigram reveals increased radiotracer activity in the left thigh.
-
Ultrasound image demonstrates a predominantly hypoechoic mass in the thigh representing a malignant fibrous histiocytoma. Regions of hyperechogenicity likely correspond to cellular components of the tumor.
-
Ultrasound image demonstrates another example of a predominantly hypoechoic mass within the patient's thigh, proven to be a malignant fibrous histiocytoma.
-
Preinfusion T1-weighted MRI reveals a large mass. Although slightly heterogeneous, the tumor is predominantly isointense to muscle.
-
T1-weighted MRI obtained following intravenous administration of gadolinium reveals circumferential enhancement of the tumor (same patient as in the previous image).
-
T2-weighted MRI reveals heterogeneous signal of the malignant fibrous histiocytoma (same patient as in the previous image). Central low signal intensity may be the result of old blood products.
-
Preinfusion T1-weighted MRI of a patient with a medial left thigh mass proven at biopsy to represent a malignant fibrous histiocytoma. Although slightly heterogeneous, the mass is predominantly isointense to muscle.
-
T2-weighted MRI obtained following gadolinium administration reveals heterogeneous enhancement of the malignant fibrous histiocytoma.
-
Malignant fibrous histiocytoma. T2-weighted MRI reveals predominantly increased signal intensity in the tumor mass (same patient as in the previous image).
-
Technetium-99m bone scintigram (delayed phase) reveals increased radiotracer uptake in the left thigh.
-
Spot images from technetium-99m scintigram (blood pool phase) reveal increased radiotracer uptake in the left thigh.