Practice Essentials
The lungs are one of the most common targets for metastatic disease. [1] Pulmonary lymphangitic carcinomatosis (PLC) is the spread of tumor to the lymphatic system of the lungs, and primary lesions commonly associated with pulmonary lymphangitic carcinomatosis include breast, stomach, lung, pancreas, colon, stomach, and prostate. [2] Most pulmonary metastases are nodular, but a significant minority is interstitial. In PLC, there is diffuse infiltration and obstruction of pulmonary parenchymal lymphatic channels by tumor. Various neoplasms can cause lymphangitic carcinomatosis, but 80% are adenocarcinomas. [3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15] LC can also arise from choriocarcinoma, melanoma, or metastatic adenocarcinoma from an unknown primary cancer. [16, 17]
The differential diagnosis can generally be narrowed by determining whether the interstitial thickening is smooth or nodular, along with septal thickening, lymphadenopathy, alveolar opacities, and pericardial effusions. [17]
In a patient with a known malignancy, the usual presenting complaint is breathlessness. Occasionally, patients have a dry cough or hemoptysis. Symptoms often precede the development of any radiographic abnormality. [18, 19, 20]
(Radiographic characteristics of lymphangitic carcinomatosis are presented in the images below.)
 Typical radiographic appearance of lymphangitic carcinomatosis in a patient with breathlessness. Diffuse, bilateral reticulonodular opacification with Kerley B lines is noted.
Typical radiographic appearance of lymphangitic carcinomatosis in a patient with breathlessness. Diffuse, bilateral reticulonodular opacification with Kerley B lines is noted.
 Fine reticular opacification with Kerley B lines and a tiny left pleural effusion are demonstrated in a patient with a lymphangitic spread of cervical carcinoma.
Fine reticular opacification with Kerley B lines and a tiny left pleural effusion are demonstrated in a patient with a lymphangitic spread of cervical carcinoma.
Preferred examination
Plain chest radiography is the initial investigation of choice in patients presenting with any respiratory symptoms, and this examination is used in staging most cancers. However, the radiographic features of LC are essentially nonspecific, with a diagnostic accuracy of 23%. Furthermore, chest radiographic findings are normal in as many as 50% of patients with histologic evidence of disease. [21, 22]
In the appropriate clinical circumstances or when the chest radiographic findings are equivocal, the next investigation employs high-resolution computed tomography (HRCT) scanning, which has a higher sensitivity than radiography, although, as with radiography, the findings may not be diagnostic. [23, 24] Although the appearance of LC on HRCT scans is nonspecific, the observation of certain features in a symptomatic patient with an appropriate history of malignancy is highly suggestive of LC; in such instances, further investigation is generally not required. The differential diagnosis includes other malignant conditions, such as lymphoma and Kaposi sarcoma, as well as benign entities, such as sarcoidosis. [23, 17]
Fragmented scintigraphic perfusion defects have been reported in LC, as have ventilation-perfusion (V/Q) mismatches. [25, 26] However, a diagnosis of LC cannot be reliably based on the presence of these features. Perfusion defects on a V/Q scan are also described in various pulmonary pathologies, the most important of which is pulmonary embolism.
Radiography
On radiographs, lymphangitic carcinomatosis (LC) appears as reticular or reticulonodular opacification, often with associated septal lines (Kerley A and B lines), peribronchial cuffing, pleural effusions, and mediastinal and/or hilar lymphadenopathy (20-50% of cases). [22, 27, 28, 29]
(The images below demonstrate the radiographic characteristics of LC.)
 Typical radiographic appearance of lymphangitic carcinomatosis in a patient with breathlessness. Diffuse, bilateral reticulonodular opacification with Kerley B lines is noted.
Typical radiographic appearance of lymphangitic carcinomatosis in a patient with breathlessness. Diffuse, bilateral reticulonodular opacification with Kerley B lines is noted.
 Fine reticular opacification with Kerley B lines and a tiny left pleural effusion are demonstrated in a patient with a lymphangitic spread of cervical carcinoma.
Fine reticular opacification with Kerley B lines and a tiny left pleural effusion are demonstrated in a patient with a lymphangitic spread of cervical carcinoma.
Chest radiographic findings are normal in most patients with LC, with the accurancy of chest radiography in this disease being only 23%. In addition, a false-positive diagnosis may occur with other interstitial lung diseases. On chest radiographs, the linear pattern of Kerley A and B lines has a variety of causes, the most common of which is hydrostatic interstitial edema. Besides LC, other causes include sarcoidosis and interstitial pneumonias. All of these conditions have a similar appearance to congestive heart failure; thus, the differentiation is largely clinically based. LC and interstitial pneumonias are often asymmetrically distributed, a characteristic that may be useful in distinguishing these from pulmonary edema. (See the image below.) [30]
Computed Tomography
The mainstay of lymphangitic carcinomatosis (LC) detection is high-resolution computed tomography (HRCT) scanning. Although HRCT scanning is a sensitive technique, the findings may not be diagnostic. HRCT scan findings include the following [23, 24, 31, 32, 33, 34, 35, 36, 17] :
-
Irregular, nodular, and/or smooth, interlobular septal thickening
-
Thickening of the fissures as a result of the involvement of the lymphatics concentrated in the subpleural interstitium
-
Preservation of normal parenchymal architecture at the level of the secondary pulmonary lobule
-
Peribronchovascular thickening
-
Centrilobular peribronchovascular thickening, which predominates over interlobular septal thickening in a minority of patients
-
Polygonal arcades or polygons with prominence of the centrilobular bronchovascular bundle in association with interlobular septal thickening (50%)
-
Mediastinal and/or hilar lymphadenopathy (30-50%)
-
Pleural effusions (30-50%)
Findings may be unilateral or bilateral, focal or diffuse, and symmetrical or asymmetrical. [37] Focal, unilateral disease accounts for 50% of cases. This pattern is associated in particular with underlying bronchogenic carcinoma. All of the changes described above are often associated with nodular opacities.
(The HRCT scan characteristics of lymphangitic carcinomatosis are demonstrated below.)
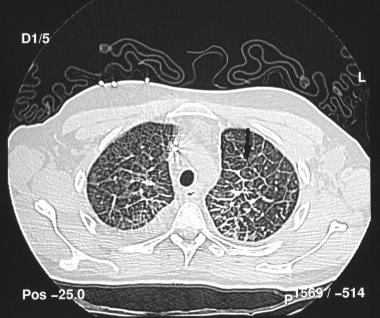
 High-resolution computed tomography scan demonstrates smooth and nodular interlobular septal thickening (arrow).
High-resolution computed tomography scan demonstrates smooth and nodular interlobular septal thickening (arrow).
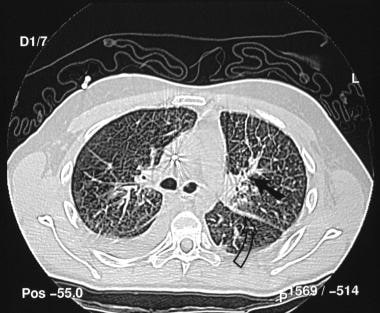
 High-resolution computed tomography scan demonstrates irregularly thickened septa that have created polygonal arcades (arrow).
High-resolution computed tomography scan demonstrates irregularly thickened septa that have created polygonal arcades (arrow).
 Prominent axial interstitium with thickened bronchovascular bundles (solid arrow). Also note the thickening of the fissure secondary to the involvement of subpleural lymphatics (open arrow).
Prominent axial interstitium with thickened bronchovascular bundles (solid arrow). Also note the thickening of the fissure secondary to the involvement of subpleural lymphatics (open arrow).
Although the appearance of LC on HRCT scans is nonspecific, the development of HRCT scan features in a symptomatic patient with an appropriate history of malignancy is highly suggestive of LC, and further investigation is usually not required. LC may not be recognized in the presence of normal radiographic chest findings.
The differential diagnosis of LC includes sarcoidosis and other chronic interstitial lung diseases such as silicosis, coal worker's pneumoconiosis, extrinsic allergic alveolitis (hypersensitivity pneumonitis), and cryptogenic fibrosing alveolitis, as well as other neoplasms, such as lymphoma and Kaposi sarcoma. Most of these diagnoses can be excluded on the basis of the clinical findings alone. The relative absence of polygons and the presence of architectural distortion at the level of the secondary pulmonary lobule strongly suggest fibrosis rather than LC. Furthermore, parenchymal involvement in sarcoidosis is typically more central and/or perihilar, as well as more bilaterally symmetrical, than it is in LC. LC never appears as honeycombing, and sarcoid granulomas are often subpleural.
Nuclear Imaging
Fragmented scintigraphic perfusion defects have been reported in lymphangitic carcinomatosis (LC), as have V/Q mismatches. However, these features are not reliable in the diagnosis of LC. [4, 38] FDG-PET scanning is used in the diagnosis and characterization of primary or secondary lung neoplasms, but its value in the characterization of LC is not well documented. [39, 40, 41, 42, 43]
In a study comparing findings from FDG-PET scans with those from HRCT scans in 5 patients with pulmonary LC, [41] the FDG-PET scan activity distribution appeared to be identical to abnormal lung areas (which could be segmental, lobar, or diffuse) observed on HRCT scans. In segmental LC, a linear or a hazy area of FDG uptake extending from the tumor could be seen. An earlier study in 7 patients showed similar results, with the intensity of FDG uptake in the diseased lung being significantly greater than in the normal, contralateral lung. [44]
One study, by Prakash et al, reported that F-18 FDG PET/CT was 100% specific and 86% sensitive in diagnosing PLC by subjective analysis. The mean standard uptake value (SUV) in the region of pulmonary lymphangitic carcinomatosis was 1.37 ± 0.64, versus 0.51 ± 0.29 in normal lung. The standard uptake ratio (SUR) of mediastinal blood pool to lymphangitic lung was 1.26 ± 0.45, versus 3.78 ± 1.37 for that of blood pool to normal lung. [43, 45]
Lung perfusion defects on VQ lung scans have been described as secondary to lymphangitic carcinomatosis or due to tumor microemboli. Charest et al designed a retrospective study to determine the prognostic value of a lymphangitic carcinomatosis pattern on perfusion lung scan. They identified 32 patients from 21 published papers internationally. The perfusion pattern defect was more commonly identified in women (81%) and associated with a progressive dyspnea (69%) and normal or minimal findings on a chest radiograph (58%). Of the 29 patients with available outcome data, 23 (79%) had a progressive course after the lung scan interpretation. The study revealed that lymphangitic carcinomatosis perfusion pattern on scintigraphic imaging is associated with an extremely poor prognosis. Physicians caring for oncology patients need to be aware of this finding, as it may make a difference to the treatment plan. [6]
A study by Ooi et al showed that increased diffuse FDG uptake in the lungs correlated with the CT pattern of pulmonary lymphangitic carcinomatosis in patients with non-small cell lung cancer. [46]
A report has been published on lymphangitic carcinomatosis visualized with gallium-68 prostate-specific membrane antigen PET in a patient with prostate cancer. [47]
-
Typical radiographic appearance of lymphangitic carcinomatosis in a patient with breathlessness. Diffuse, bilateral reticulonodular opacification with Kerley B lines is noted.
-
Endoscopic image of the stomach shows a primary, ulcerating gastric carcinoma.
-
Fine reticular opacification with Kerley B lines and a tiny left pleural effusion are demonstrated in a patient with a lymphangitic spread of cervical carcinoma.
-
High-resolution computed tomography scan demonstrates smooth and nodular interlobular septal thickening (arrow).
-
High-grade non–Hodgkin lymphoma mimics lymphangitic carcinomatosis. Note the diffuse interstitial pattern and a tiny left pleural effusion.
-
High-resolution computed tomography scan demonstrates irregularly thickened septa that have created polygonal arcades (arrow).
-
Prominent axial interstitium with thickened bronchovascular bundles (solid arrow). Also note the thickening of the fissure secondary to the involvement of subpleural lymphatics (open arrow).








