Practice Essentials
Primary tuberculosis has generally been defined as onset of clinical disease within 12 months of initial infection with Mycobacterium tuberculosis. [1] Tuberculosis may involve multiple organs, such as the lung, liver, spleen, kidney, brain, and bone. In endemic regions, the normal host immune response may be sufficient to contain the infection and prevent clinical presentation. Uncontrolled or uncontained infection may result in high morbidity and mortality. A third of the world's population is said to have contracted M tuberculosis, with estimates of 10 million new infections globally each year. The major pathology is necrotizing granulomatous inflammation, with the lungs being the primary organs of involvement in up to 87% of cases. [2, 3, 4]
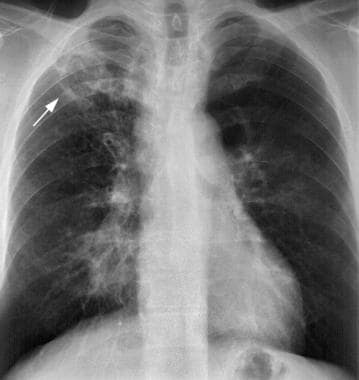
If patients with primary tuberculosis undergo imaging, a conventional chest radiograph may be sufficient for diagnosis in the appropriate clinical setting. [1, 5] (A case of primary pulmonary tuberculosis is depicted in the image below.) In patients with progressive primary or postprimary tuberculosis, computed tomography scanning is often performed, in addition to chest radiography. [5] Magnetic resonance imaging may be used to evaluate complications of thoracic disease, such as the extent of thoracic wall involvement with empyema, but is of limited value in the evaluation of patients with pulmonary tuberculosis. [6, 7, 8, 9, 10]
Early in the disease, chest radiographs are usually normal. Hilar lymphadenopathy is a hallmark radiologic finding of tuberculosis, with other common findings being perihilar and right-sided infiltration and pleural effusion. [2, 3, 4, 11, 12] The gold standard for TB screening is sputum culture, but posterior-anterior chest radiography is considered a safe, effective modality and is recommended by the World Health Organization because of its high sensitivity, wide availability, and relatively low cost. [13, 11, 14, 15]
Concerning characterization of the infection as active or not, CT is more sensitive than radiography, and fluorodeoxyglucose positron emission tomography/CT (FDG PET/CT) has yielded promising results. [8]
 Young male patient with fever and cough has a focal opacity in the left lower lobe that looks like a pneumonia. This is a case of primary tuberculosis in an adult.
Young male patient with fever and cough has a focal opacity in the left lower lobe that looks like a pneumonia. This is a case of primary tuberculosis in an adult.
Conventional radiography is limited in its sensitivity and specificity. As many as 15% of patients with primary tuberculosis have normal chest radiographic findings. Clinical suspicion must remain high for prompt diagnosis in these individuals. Chest radiographic results are not specific for tuberculosis, and other entities must remain in the differential diagnosis. [16, 17, 18]
Typically, ultrasonography is not useful in imaging pulmonary disease. This modality may be used for thoracentesis guidance or to evaluate the pericardium for secondary tuberculous involvement.
Angiography is not used in the diagnosis of pulmonary tuberculosis. Angiographic techniques, such as bronchial arteriography and embolization in patients with hemoptysis, may be used to treat the complications of cavitary pulmonary tuberculosis.
Patients with postprimary tuberculosis may also undergo bronchoscopy to evaluate endobronchial disease and to obtain sputum specimens for microbacteriologic cultures. [19, 20, 21, 6, 22]
Interventional radiologists may be consulted to perform diagnostic and therapeutic bronchial artery studies, and interventional radiologic techniques may be used to confirm the diagnosis with percutaneous lymph node aspiration or biopsy to obtain material for culture, cytologic, or histologic studies. Radiologists may perform stent placement with fluoroscopic and/or CT guidance in collaboration with the bronchoscopist, and they often obtain fluid for evaluation by performing ultrasonography- or CT-guided thoracentesis.
Radiography
Pulmonary imaging findings in individuals with primary tuberculosis are nonspecific. Common findings include segmental or lobar airspace consolidation, ipsilateral hilar and mediastinal lymphadenopathy, and/or pleural effusion. Atelectasis may occur in primary pulmonary tuberculosis, often as a consequence of tuberculous airway involvement. The imaging features of primary tuberculosis may mimic those of other infectious processes. A finding that differentiates primary tuberculosis from other infectious processes is lymphadenopathy, which is typically absent in bacterial pneumonia. [12, 14]
Postprimary tuberculosis may be recognized more readily with the presence of fibrocavitary disease and a history of prior tuberculosis exposure or infection. Radiologic findings of postprimary tuberculosis are highly suggestive of, but not pathognomonic for, the disease. Inactive disease cannot be established without prior radiographs, regardless of the pattern.
As many as 15% of conventional chest radiographs may be normal in primary tuberculosis. In the immunocompromised population, lymphadenopathy occasionally may occur in isolation, and it may not be detected on conventional radiographs. Additional imaging with CT is often required, because CT is more sensitive in depicting lymphadenopathy.
Note that chest radiographic findings may be normal in as many as 15% of patients with primary pulmonary tuberculosis.
(The radiographic characteristics of primary and postprimary pulmonary tuberculosis are displayed in the images below.)
 Young male patient with fever and cough has a focal opacity in the left lower lobe that looks like a pneumonia. This is a case of primary tuberculosis in an adult.
Young male patient with fever and cough has a focal opacity in the left lower lobe that looks like a pneumonia. This is a case of primary tuberculosis in an adult.
 Posteroanterior chest radiograph in a young patient shows a right upper lobe and right lower lobe consolidation and a small pleural effusion on the right side.
Posteroanterior chest radiograph in a young patient shows a right upper lobe and right lower lobe consolidation and a small pleural effusion on the right side.
 A middle-aged man presents with a cough and fever lasting several weeks. Posteroanterior chest radiograph shows a prominent paratracheal area on the right, lymphadenopathy, a cavitary opacity in the right upper lobe, and a focal consolidation in the middle lung zone on the right. The patient was ultimately found to have primary progressive tuberculosis.
A middle-aged man presents with a cough and fever lasting several weeks. Posteroanterior chest radiograph shows a prominent paratracheal area on the right, lymphadenopathy, a cavitary opacity in the right upper lobe, and a focal consolidation in the middle lung zone on the right. The patient was ultimately found to have primary progressive tuberculosis.
Parenchymal consolidation in primary pulmonary tuberculosis
Parenchymal consolidation may be observed. Although consolidation may occur in any segment or lobe or in multiple segments or lobes, the disease has a predilection for the lower lobes, for the middle lobe and lingula, and for the anterior segments of the upper lobes.
Airspace consolidation tends to be homogeneous, with ill-defined margins. If the consolidation abuts a fissure, a well-defined margin may be identified. Cavitation within parenchymal opacity is distinctly uncommon in primary infection. As the host immune response continues, healing begins. Caseous necrosis occurs centrally within the lung parenchymal opacity, decreasing its size.
The lung opacity tends to become rounded with healing, and it continues to shrink until only a small nodule remains. Subsequently, the nodule may become calcified or ossified, resulting in a calcified granuloma. Note that although a granuloma may calcify, this does not necessarily reflect an absence of bacilli. The organisms may remain quiescent within this nodule, serving as a possible source for reactivation of disease.
Lymphadenopathy in primary pulmonary tuberculosis
Lymphadenopathy is a common manifestation of primary pulmonary tuberculosis. The presence of hilar and mediastinal lymphadenopathy may distinguish primary from postprimary tuberculosis, because lymphadenopathy is conspicuously absent in postprimary tuberculosis. Lymphadenopathy may be symptomatic if it secondarily involves the airways.
Lymphadenopathy without a parenchymal opacity may occur as the only manifestation of primary pulmonary tuberculosis. This is seen most often in the population with human immunodeficiency virus (HIV) infection. (In adults with HIV infection, adenopathy is common.)
As expected, adenopathy is most common in the ipsilateral hilar region. Hilar lymphadenopathy is seen in approximately 60% of children with primary tuberculosis, paratracheal adenopathy is seen in 40%, and subcarinal lymphadenopathy is seen in 80%.
In adults, lymphadenopathy is unusual in an immunocompetent host, but it does occur. The pattern of lymphadenopathy is indistinguishable from that of sarcoid or lymphoma.
With an appropriate immune response or with adequate chemotherapy, enlarged necrotic lymph nodes may diminish in size and commonly calcify. The presence of calcified lymph node and a granuloma represents the Ranke complex.
Airway involvement in primary pulmonary tuberculosis
Airway involvement is frequently present in primary tuberculosis and may take any of the following forms:
-
Airway compression by adjacent lymphadenopathy with resultant atelectasis
-
Mucosal infection with resultant ulceration and long-term stricture formation
-
Broncholithiasis (ie, extrinsic erosion of a bronchus by adjacent lymphadenopathy, with extrusion of calcified material into the bronchus)
-
Endobronchial spread of infection
-
Bronchiectasis
Atelectasis is most notable within the anterior segments of the upper lobes and the medial segment of the middle lobe. Atelectasis may resolve as lymphadenopathy regresses with host response. A sudden resolution of atelectasis may represent perforation of an infected lymph node into the airway, which relieves the bronchial obstruction.
A possible long-term sequela of infection is tracheobronchial stenosis. The airways may be involved by tuberculosis in a variety of ways, including direct mucosal involvement from infected sputum, direct extension from perforating lymphadenopathy or adjacent parenchymal infection, and hematogenous or lymphatic drainage.
The endobronchial spread of infection may be seen with tuberculous tracheobronchial disease. Bacilli from the infected airways disseminate into more distal bronchi and bronchioles and subsequently enter the alveoli, where they become deposited. The resultant radiographic appearance is one of small ill-defined acinar shadows and small nodules.
Endobronchial tuberculosis may lead to bronchiectasis, either from bronchial stenosis or secondary to traction from fibrosis. Bronchiectasis is more frequently seen in postprimary tuberculosis.
Pleural involvement in primary pulmonary tuberculosis
Pleural involvement is uncommon in children with primary tuberculosis, occurring in approximately 10% of these patients. Pleural involvement is seen more frequently in adults with primary pulmonary tuberculosis, and it is even more frequently identified in postprimary tuberculosis.
Postprimary pulmonary tuberculosis
The findings of reactivation tuberculosis typically become radiographically apparent within 2 years of the initial infection. [26] Pleural effusions develop if the infection remains untreated. Tuberculous empyema is a much less common finding.
In postprimary tuberculosis, the earliest radiologic sign is small nodules and branching centrilobular lesions that increase in size and coalesce to form ill-defined patchy consolidations; cavitations are very characteristic of active disease. [9]
Parenchymal manifestations of postprimary pulmonary tuberculosis
Postprimary tuberculosis may have any of a number of parenchymal manifestations. Patchy or confluent airspace opacities are opacities that involve the apical and posterior segments of the upper lobes and the superior segments of the lower lobes.
In postprimary tuberculosis, cavitary disease is secondary to caseous necrosis within the opacity. [27] The debris from the lesion is expelled via the tracheobronchial tree with which the cavity is in communication. The cavities, similar to airspace opacities in reactivation tuberculosis, are commonly within the upper lung zones. The cavities demonstrate a thick outer wall with a smooth inner contour. Air-fluid levels may be present. Superinfection by Aspergillus organisms may occur, leading to a mycetoma.
Tuberculomas are rounded discrete nodules that are known to harbor bacilli. They may be present in primary or postprimary tuberculosis and radiographically appear as discrete nodules, typically within the upper lobes. Tuberculomas may calcify. Satellite lesions (ie, small discrete nodules in the vicinity of the tuberculoma) are present in as many as 90% of patients.
Endobronchial spread of infection with acinar opacities occurs as a consequence of infected material passing into the tracheobronchial tree from an infected portion of the lung. The organisms pass via the airways into previously uninvolved portions of the lung. The radiographic appearance is one of widespread ill-defined acinar shadows. Foci may become confluent and mimic bacterial pneumonia. Spread from the upper lobes to the lower lobes is common and called the upstairs-downstairs pattern.
Pulmonary miliary tuberculosis is a consequence of hematogenous spread of organisms to the pulmonary parenchyma. Radiographically, miliary spread can be recognized by circumscribed nodules less than 1-2 mm in diameter located diffusely throughout both lungs.
Lymphadenopathy in postprimary pulmonary tuberculosis
In contrast to primary tuberculosis, lymphadenopathy is notably absent in patients with postprimary tuberculosis, with the exception of patients with HIV or AIDS.
Airway involvement in postprimary pulmonary tuberculosis
Tracheobronchial stenosis may not be directly visualized on conventional chest radiographs. Airway stenosis may result in atelectasis in the segments of the lung supplied by that bronchus.
Bronchiectasis may be visualized on radiographs as dilated air-containing structures, with a tram-track appearance representing the parallel walls of the dilated airway. Dilated bronchi may be irregular in caliber and varicoid in appearance or may be cystic. Traction bronchiectasis may occur as well, as a consequence of fibrosis.
Pleural involvement in postprimary pulmonary tuberculosis
Pleural involvement is seen more commonly in postprimary tuberculosis than in primary infection. Pleural effusions may occur and may progress to empyema. An empyema may require emergent surgical intervention because the infection is maintained within a closed space and because it may result in rapid destruction of surrounding structures (eg, lung parenchyma, osseous structures of the thorax).
If infection extends from the pleural space to involve the chest wall, it is called empyema necessitans. Osseous destruction and, possibly, air within subcutaneous tissues may be identified radiographically, or the empyema may present as a palpable soft-tissue mass.
Computed Tomography
In primary pulmonary tuberculosis, CT scanning helps confirm the presence of an ill-defined parenchymal infiltrate, as well as lymphadenopathy. [28, 7, 29, 30, 31, 32, 33] CT is the examination of choice for evaluating lymphadenopathy and involvement of the tracheobronchial tree. Lymphadenopathy causing bronchial compression can be identified, and airway compromise can be monitored during chemotherapy. CT scans may demonstrate enlarged lymph nodes typically measuring more than 2 cm.
Lymph nodes demonstrate central hypoattenuation with peripheral rim enhancement with the administration of contrast material. This appearance reflects central necrosis within the node. Broncholiths may be identified in rare cases.
Morphologically, the stenoses in active disease are areas of irregular luminal narrowing with circumferential wall thickening. Associated mediastinitis and even mediastinal abscesses may be present. Small pleural effusions are detected more readily on CT scans than on other images. Contrast enhancement may be useful in identifying evolution into an empyema.
Pericardial disease can be imaged with CT scanning or MRI, although calcification related to prior tuberculous pericarditis is more readily apparent on CT images. Osseous involvement is well delineated on CT scans; however, MRI is often necessary to evaluate the disk and the spinal canal.
(The CT scan characteristics of primary and postprimary tuberculosis are displayed in the images below.)
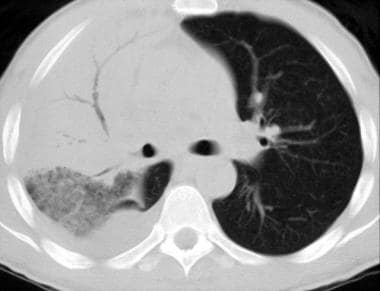 CT scan in a young patient, obtained with the pulmonary window setting, demonstrates consolidation in the right upper lobe, ground-glass opacities in the right lower lobe, and a pleural effusion on the right side. This patient has extensive tuberculous pneumonia and is immunocompromised.
CT scan in a young patient, obtained with the pulmonary window setting, demonstrates consolidation in the right upper lobe, ground-glass opacities in the right lower lobe, and a pleural effusion on the right side. This patient has extensive tuberculous pneumonia and is immunocompromised.
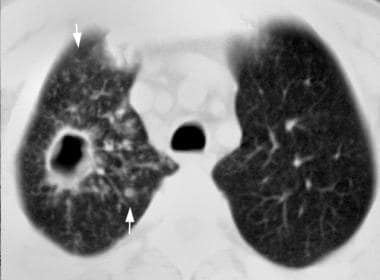 A middle-aged man presents with a cough and fever lasting several weeks. CT scan obtained with the pulmonary window setting in the right upper lobe shows an irregular, thick-walled cavity with some increased markings around it. A nearby nodule is also shown.
A middle-aged man presents with a cough and fever lasting several weeks. CT scan obtained with the pulmonary window setting in the right upper lobe shows an irregular, thick-walled cavity with some increased markings around it. A nearby nodule is also shown.
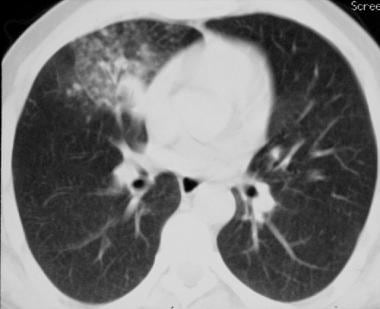 CT scan obtained with pulmonary window setting in the right middle lobe (same patient as in the previous image) shows a focal area of consolidation with what may be tiny nodules. This patient has primary progressive tuberculosis with radiographic manifestations of mediastinal adenopathy, cavitary process, and endobronchial spread that occurs over a short period. He had a history of alcohol abuse.
CT scan obtained with pulmonary window setting in the right middle lobe (same patient as in the previous image) shows a focal area of consolidation with what may be tiny nodules. This patient has primary progressive tuberculosis with radiographic manifestations of mediastinal adenopathy, cavitary process, and endobronchial spread that occurs over a short period. He had a history of alcohol abuse.
Postprimary pulmonary tuberculosis
CT scans may be helpful in evaluating parenchymal involvement, satellite lesions, bronchogenic spread of infection, and miliary disease.
Cavitation is best demonstrated on CT scans. The outer wall of the cavity tends to be thick walled and irregular, whereas the inner wall tends to be smooth. An air-fluid level may be identified. The connection of the cavity to the airway may be visualized. Complications of cavitary disease may become apparent with mycetoma formation, which appears as an intraluminal collection of material with a crescent of surrounding air. Changes in patient positioning demonstrate a change in the position of the mycetoma relative to the cavity.
Tuberculomas can be identified on CT scans as rounded nodules that usually have surrounding associated satellite lesions. The bronchogenic spread of tuberculosis is recognized on CT scans by the presence of acinar shadows and nodules of varying sizes in a peribronchial distribution. The lesions are seen throughout both lungs.
Miliary tuberculosis is characterized by randomly distributed tiny nodules (1-2 mm), which tend to be smooth and well marginated. Calcification is notably absent; this observation may aid in differentiating tuberculosis from metastatic diseases such as thyroid carcinoma.
CT scans may aid in the evaluation of uncommon complications of miliary tuberculosis, such as acute respiratory distress syndrome (ARDS) and pulmonary hemorrhage resulting from disseminated intravascular coagulopathy. Both ARDS and pulmonary hemorrhage may manifest as alveolar filling in a background of miliary nodules.
Airway involvement
CT scanning is the examination of choice for evaluating the tracheobronchial tree. Lymphadenopathy is a feature of primary infection; however, calcified lymph nodes may cause persistent extrinsic compression on the bronchi.
Bronchial stenosis is more common in postprimary disease than in primary tuberculosis. In fibrocavitary tuberculosis, the proximal bronchi are more typically involved than the peripheral airways. Variable areas of stenosis are demonstrated. Wall thickening tends to be less marked than in primary tuberculosis. [34]
Bronchiectasis is a well-known sequela of postprimary disease. Bronchiectasis tends to occur in the upper lobes and often manifests as traction bronchiectasis on the basis of fibrotic disease with subsequent traction on the airways. Recurrent infections and hemoptysis may result from traction bronchiectasis.
Pleural involvement
Empyema is visualized on contrast-enhanced CT scans with enhancement of the parietal and visceral pleurae. They may demonstrate enhancing septa within the pleural fluid collections. The pleural fluid collections are characterized by low attenuation; however, they do not have attenuation values consistent with simple fluid. Empyemas demonstrate the so-called split pleura sign. This sign consists of the pleural fluid collection tracking between the abnormally enhancing parietal and visceral pleura.
Spontaneous pneumothorax is an uncommon complication of disease; it may be secondary to peripherally located lesions. Involvement of the pericardium and spine may be demonstrated on CT images.
-
Young male patient with fever and cough has a focal opacity in the left lower lobe that looks like a pneumonia. This is a case of primary tuberculosis in an adult.
-
Posteroanterior chest radiograph in a young patient shows a right upper lobe and right lower lobe consolidation and a small pleural effusion on the right side.
-
CT scan in a young patient, obtained with the pulmonary window setting, demonstrates consolidation in the right upper lobe, ground-glass opacities in the right lower lobe, and a pleural effusion on the right side. This patient has extensive tuberculous pneumonia and is immunocompromised.
-
A middle-aged man presents with a cough and fever lasting several weeks. Posteroanterior chest radiograph shows a prominent paratracheal area on the right, lymphadenopathy, a cavitary opacity in the right upper lobe, and a focal consolidation in the middle lung zone on the right. The patient was ultimately found to have primary progressive tuberculosis.
-
A middle-aged man presents with a cough and fever lasting several weeks. CT scan obtained with the pulmonary window setting in the right upper lobe shows an irregular, thick-walled cavity with some increased markings around it. A nearby nodule is also shown.
-
CT scan obtained with pulmonary window setting in the right middle lobe (same patient as in the previous image) shows a focal area of consolidation with what may be tiny nodules. This patient has primary progressive tuberculosis with radiographic manifestations of mediastinal adenopathy, cavitary process, and endobronchial spread that occurs over a short period. He had a history of alcohol abuse.
-
Pulmonary Tuberculosis with Air fluid Level









