Practice Essentials
The liver is the largest solid abdominal organ with a relatively fixed position, which makes it prone to injury. The liver is the most regularly injured organ in blunt abdominal trauma. Damage to the liver is the most common cause of death after abdominal injury (see the images below). The most common cause of liver injury is blunt abdominal trauma, which is secondary to motor vehicle accidents in most instances. [1]
In the past, most of these injuries were treated surgically. However, surgical literature confirms that as many as 86% of liver injuries have stopped bleeding by the time surgical exploration is performed, and 67% of operations performed for blunt abdominal trauma are nontherapeutic.
Philipoff et al have proposed that a stiff, cirrhotic liver may represent an important risk factor for blunt gallbladder injury. Almost all gallbladder injuries following blunt trauma are associated with other significant intra-abdominal injuries, and in the setting of acute trauma, the authors recommend an open procedure to facilitate exploration to rule out associated injuries. Cholecystectomy remains the definitive management for gallbladder trauma. Gallbladder rupture is seen in less than 1% of cases of blunt abdominal trauma. [2]
Conservative, nonoperative management has become the treatment of choice for blunt hepatic trauma in hemodynamically stable patients. The increased use of nonoperative management has been facilitated by advancements such as higher-resolution CT, increased availability of interventional procedures such as angiography and embolization, image-guided percutaneous drainage, and endoscopy. Such advancements have also helped to quickly identify the need for urgent laparotomy and attention to visceral and vascular injuries. [3] Almost 80% of adults and 97% of children are treated conservatively by using careful follow-up imaging studies. [4, 5, 6, 7, 8]
For hepatic lesions that are grade 1 through 3, according to the American Association for the Surgery of Trauma (AAST) (see below), nonoperative management is indicated if there is no injury to abdominal organs. Surgical intervention is required for any lesions higher than grade IV in which there is hemorrhagic risk or recurrence. [7]
AAST Liver Trauma Classification
The AAST has classified liver trauma injuries as follows [9, 7, 10] :
-
Grade I: hematoma, subcapsular < 10% surface area; laceration, capsular tear < 1 cm parenchymal depth.
-
Grade II: hematoma, subcapsular 10-50% surface area; intraparenchymal, < 10 cm diameter; laceration, capsular tear 1-3 cm parenchymal depth, < 10 cm in length.
-
Grade III: hematoma, subcapsular >50% surface area of ruptured subcapsular or parenchymal hematoma; intraparenchymal hematoma, >10 cm or expanding; laceration, >3 cm parenchymal depth.
-
Grade IV: laceration, parenchymal disruption involving 25-75% hepatic lobe or 1-3 Couinaud segments.
-
Grade V: laceration, parenchymal disruption involving >75% of hepatic lobe or >3 Couinaud segments within a single lobe; vascular, juxtahepatic venous injuries (ie, retrohepatic vena cava/central major hepatic veins).
-
Grade VI: hepatic avulsion.
The World Society of Emergency Surgery (WSES) has presented the following classification utilizing the AAST grading system [11] :
-
Grade I (minor hepatic injury): AAST-OIS (Organ Injury Scale) grade I-II, hemodynamically stable.
-
Grade II (moderate hepatic injury): AAST-OIS grade III, hemodynamically stable.
-
Grade III (severe hepatic injury): AAST-OIS grade IV-V, hemodynamically stable.
-
Grade IV (severe hepatic injury): AAST-OIS grade I-VI, hemodynamically unstable.
Imaging modalities
The WSES recommends diagnostic methods based on hemodynamic status. Extended-focused abdominal sonography for trauma (E-FAST) provides rapid detection of intra-abdominal free fluid. The WSES notes that CT scan with intravenous contrast is the gold standard for hemodynamically stable trauma patients. [11]
According to the American College of Radiology (ACR), a radiography trauma series and US FAST scan of the chest, abdomen, and pelvis are usually appropriate for the initial imaging of major blunt trauma in a hemodynamically unstable patient. Whole-body CT with IV contrast, a radiography trauma series, and US FAST scan of the chest, abdomen, and pelvis are usually appropriate for the initial imaging of major blunt trauma for a hemodynamically stable patient, not otherwise specified. [12]
Plain radiographic findings are nonspecific, but they may be useful in showing the extent of associated skeletal trauma. Contrast-enhanced CT scanning remains the examination of choice in patients with blunt abdominal trauma. [13, 14, 15, 16, 17, 6, 18]
Radionuclide study with technetium-99m (99mTc) iminodiacetic acid (IDA) is the examination of choice in patients in whom bile leaks are suspected. Magnetic resonance imaging (MRI) has yet to find a role but can be used to monitor liver injury. Magnetic resonance cholangiopancreatography (MRCP) may be used for the diagnosis and follow-up observation of bile duct injuries. [19]
Angiography is useful in localizing the site of hemorrhage and in providing an opportunity for the interventional radiologist to proceed to transcatheter embolization of bleeding sites.
The original guidelines of Practice Management for Nonoperative Management of Blunt Injury to the Liver and Spleen (Eastern Association for the Surgery of Trauma guideline) remain valid, supported by the accumulation of a large amount of data. Stassen et al reviewed 176 papers, of which 94 were used to create the current practice management guideline for the selective nonoperative management of blunt hepatic injury. [20]
The Stassen review concluded that nonoperative management (NOM) of blunt hepatic injuries is the treatment modality of choice in hemodynamically stable patients, irrespective of the grade of injury or patient age. However, nonoperative imaging of blunt trauma should only be considered when reliable monitoring, serial clinical evaluations, and an operating room for urgent laparotomy are readily available. Patients who are hemodynamically unstable and have peritonitis still warrant emergent operative intervention. Ready availability of CT, angiography, percutaneous drainage, ERCP, and laparoscopy remain important adjuncts to nonoperative management of hepatic injuries. [20] The authors add that despite the explosion of literature on this topic, many questions regarding nonoperative management of blunt hepatic injuries remain without conclusive answers in the literature. [20]
In the absence of other internal injuries requiring surgery, nonoperative management is the treatment of choice for all hemodynamically stable minor, moderate, and severe injuries. The WSES further recommends that CT with IV contrast should always be performed when nonoperative management is being considered. Serial clinical evaluations (physical examination and laboratory testing) must be performed to detect a change in clinical status during nonoperative management. [11]
(See the images below.)
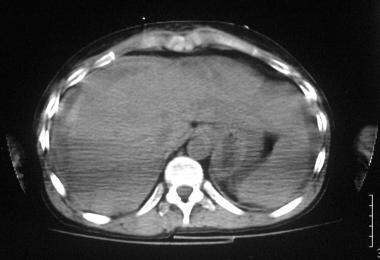
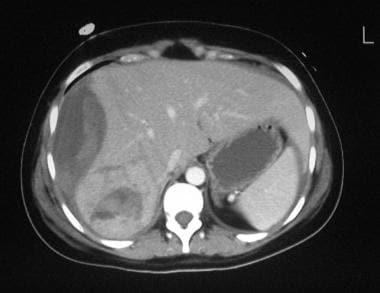
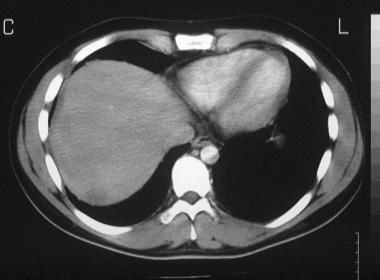 Grade 1 hepatic injury in a 21-year-old man with a stabbing injury to the right upper quadrant of the abdomen. Axial, contrast-enhanced computed tomography (CT) scan demonstrates a small, crescent-shaped subcapsular and parenchymal hematoma less than 1 cm thick.
Grade 1 hepatic injury in a 21-year-old man with a stabbing injury to the right upper quadrant of the abdomen. Axial, contrast-enhanced computed tomography (CT) scan demonstrates a small, crescent-shaped subcapsular and parenchymal hematoma less than 1 cm thick.
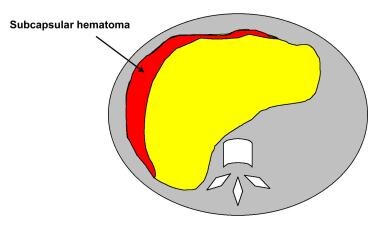
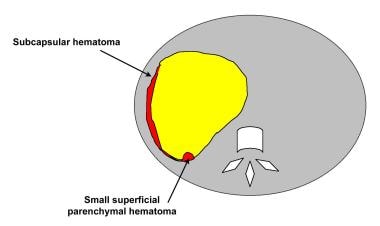 Grade 1 hepatic injury in a 21-year-old man with a stabbing injury to the right upper quadrant of the abdomen. Diagram of the CT scan in the previous image.
Grade 1 hepatic injury in a 21-year-old man with a stabbing injury to the right upper quadrant of the abdomen. Diagram of the CT scan in the previous image.
Limitations of techniques
Plain radiographs cannot depict liver trauma directly, and radiographic findings may be completely normal. In penetrating abdominal trauma, overall sensitivity of focused ultrasonography is 46%, and specificity is 94%. [21] Emergency ultrasonographic findings based on the demonstration of free fluid and/or parenchymal injury demonstrate the overall sensitivity of ultrasonography for detection of blunt abdominal trauma to be 72%. However, the sensitivity is higher (98%) for injuries of grade 3 or higher. However, negative ultrasonographic findings do not exclude hepatic injury. Angiographic images can fail to depict active bleeding, and false-negative or false-positive diagnoses can occur with liver trauma.
Radiography
Plain radiographs are usually the first radiologic examination performed in patients in whom liver trauma is suspected. Radiographs may initially depict opaque foreign bodies, such as bullets or shrapnel. Plain radiographic findings are nonspecific, but they are useful in evaluating rib and spinal injuries in patients with blunt abdominal trauma. Fractures of the right lower ribs should suggest the possibility of underlying liver injury. Pneumoperitoneum, major diaphragmatic injury, gross organ displacement, and metallic foreign bodies may be identified. [22] Because plain radiography is performed in a traumatized patient, an optimal-quality radiograph is not always possible. Fractures and a pneumoperitoneum may be missed.
Computed Tomography
CT scanning, particularly contrast-enhanced CT scanning, is accurate in localizing the site and extent of liver injuries and associated trauma, providing vital information for treatment. [13, 14, 6, 18] Spiral CT scanning is the preferred scanning technique, if available. Multidetector-row CT scanning offers the further advantages of fast scanning times (allowing scanning during specific phases of intravenous contrast enhancement) and the acquisition of thin sections over a large area (allowing high-quality multiplanar reconstruction). [23] CT scanning without intravenous contrast enhancement is of limited value in hepatic trauma, but it can be useful in identifying or following up a hemoperitoneum.
CT scans can be used to monitor healing. Trauma to the liver may result in subcapsular or intrahepatic hematoma, contusion, vascular injury, or biliary disruption. [24] CT scan criteria for staging liver trauma based on the AAST liver injury scale include the following:
-
Grade 1 - Subcapsular hematoma less than 1 cm in maximal thickness, capsular avulsion, superficial parenchymal laceration less than 1 cm deep, and isolated periportal blood tracking (see the images below).
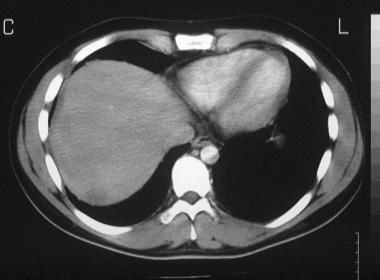 Grade 1 hepatic injury in a 21-year-old man with a stabbing injury to the right upper quadrant of the abdomen. Axial, contrast-enhanced computed tomography (CT) scan demonstrates a small, crescent-shaped subcapsular and parenchymal hematoma less than 1 cm thick.
Grade 1 hepatic injury in a 21-year-old man with a stabbing injury to the right upper quadrant of the abdomen. Axial, contrast-enhanced computed tomography (CT) scan demonstrates a small, crescent-shaped subcapsular and parenchymal hematoma less than 1 cm thick.
-
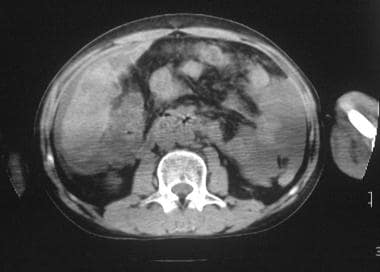
Grade 2 - Parenchymal laceration 1-3 cm deep and parenchymal/subcapsular hematomas 1-3 cm thick (see the images below).
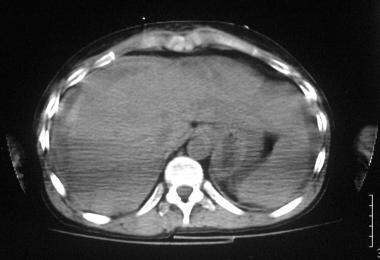 A 20-year-old man with systemic lupus erythematosus presented with grade 2 liver injury after minor blunt abdominal trauma. Nonenhanced axial CT scan at the level of the hepatic veins shows a subcapsular hematoma 3 cm thick.
A 20-year-old man with systemic lupus erythematosus presented with grade 2 liver injury after minor blunt abdominal trauma. Nonenhanced axial CT scan at the level of the hepatic veins shows a subcapsular hematoma 3 cm thick.
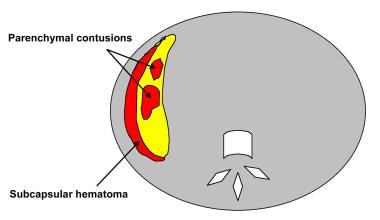
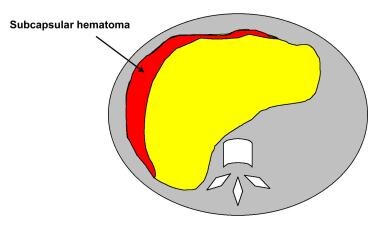 A 20-year-old man with systemic lupus erythematosus presented with grade 2 liver injury after minor blunt abdominal trauma. Diagram of the CT scan in the previous image.
A 20-year-old man with systemic lupus erythematosus presented with grade 2 liver injury after minor blunt abdominal trauma. Diagram of the CT scan in the previous image.
 A 20-year-old man with systemic lupus erythematosus presented with grade 2 liver injury after minor blunt abdominal trauma (same patient as in the previous 2 images). Axial CT image through the inferior aspect of the right lobe of the liver demonstrates multiple low-attenuation lesions in the liver consistent with parenchymal contusion.
A 20-year-old man with systemic lupus erythematosus presented with grade 2 liver injury after minor blunt abdominal trauma (same patient as in the previous 2 images). Axial CT image through the inferior aspect of the right lobe of the liver demonstrates multiple low-attenuation lesions in the liver consistent with parenchymal contusion.
-
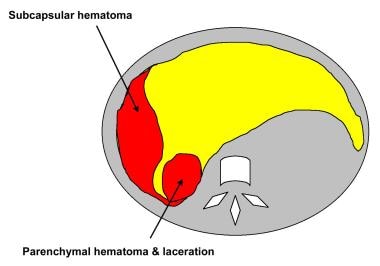
Grade 3 - Parenchymal laceration more than 3 cm deep and parenchymal or subcapsular hematoma more than 3 cm in diameter (see the images below).
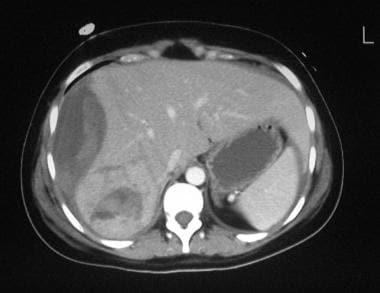 Grade 3 liver injury in a 22-year-old woman after blunt abdominal trauma. Contrast-enhanced axial CT scan through the upper abdomen shows a 4-cm-thick subcapsular hematoma associated with parenchymal hematoma and laceration in segments 6 and 7 of the right lobe of the liver. Free fluid is seen around the spleen and left lobe of the liver consistent with hemoperitoneum.
Grade 3 liver injury in a 22-year-old woman after blunt abdominal trauma. Contrast-enhanced axial CT scan through the upper abdomen shows a 4-cm-thick subcapsular hematoma associated with parenchymal hematoma and laceration in segments 6 and 7 of the right lobe of the liver. Free fluid is seen around the spleen and left lobe of the liver consistent with hemoperitoneum.
-
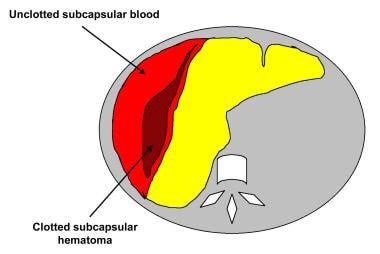
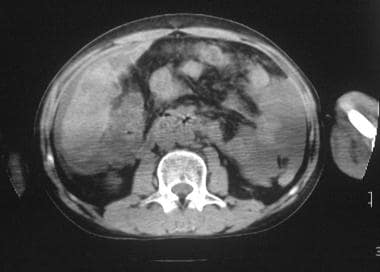
Grade 4 - Parenchymal/subcapsular hematoma more than 10 cm in diameter, lobar destruction, or devascularization (see the images below).
 Image obtained in a 35-year-old male bouncer after blunt abdominal injury. Nonenhanced axial CT scan of the abdomen demonstrates a large subcapsular hematoma measuring more than 10 cm. The high-attenuating areas within the lesion represent clotted blood. The injury was classified as a grade 4 liver injury.
Image obtained in a 35-year-old male bouncer after blunt abdominal injury. Nonenhanced axial CT scan of the abdomen demonstrates a large subcapsular hematoma measuring more than 10 cm. The high-attenuating areas within the lesion represent clotted blood. The injury was classified as a grade 4 liver injury.
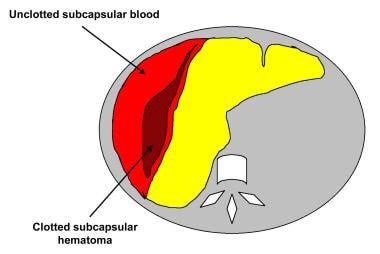 Image in a 35-year-old male bouncer after blunt abdominal injury (same patient as in the previous image). Diagram of the CT scan in Image above.
Image in a 35-year-old male bouncer after blunt abdominal injury (same patient as in the previous image). Diagram of the CT scan in Image above.
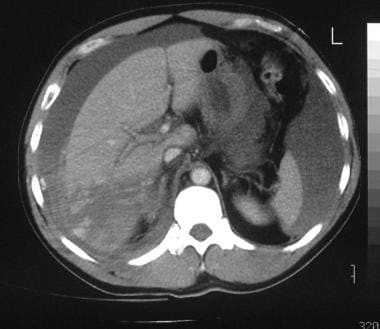
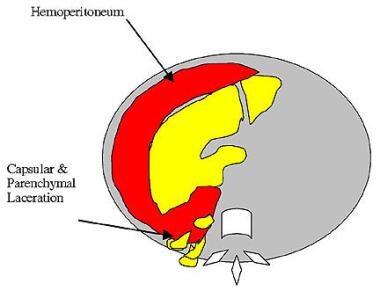
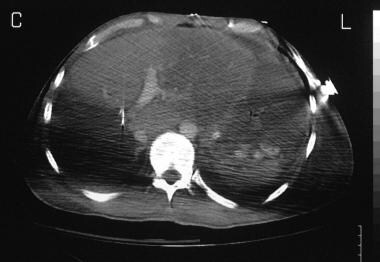
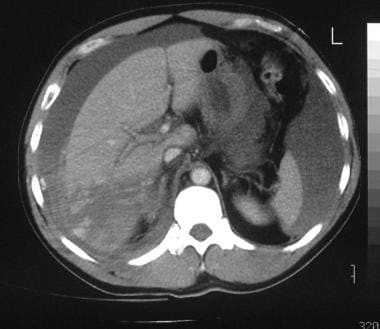 Contrast-enhanced axial CT scan in a 39-year-old man with a grade 4 liver injury shows a large parenchymal hematoma in segments 6 and 7 of the liver with evidence of an active bleed. Note the capsular laceration and large hemoperitoneum.
Contrast-enhanced axial CT scan in a 39-year-old man with a grade 4 liver injury shows a large parenchymal hematoma in segments 6 and 7 of the liver with evidence of an active bleed. Note the capsular laceration and large hemoperitoneum.
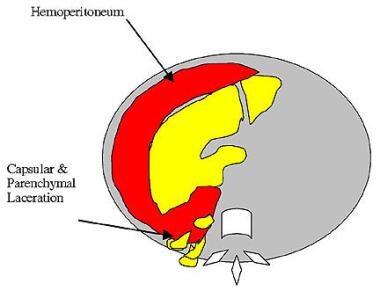 Diagram of the CT scan in Image above in a 39-year-old man with a grade 4 liver injury shows a large parenchymal hematoma in segments 6 and 7 of the liver with evidence of an active bleed.
Diagram of the CT scan in Image above in a 39-year-old man with a grade 4 liver injury shows a large parenchymal hematoma in segments 6 and 7 of the liver with evidence of an active bleed.
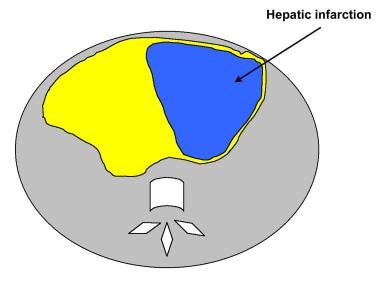
 Multisegment infarct (segments 2, 3, 4a, and 4b) in a 40-year-old man who was in a motor vehicle accident and underwent emergency segmental resection of the right lobe. Note the sharply demarcated wedge-shaped area of infarction; hence, the classification as grade 4.
Multisegment infarct (segments 2, 3, 4a, and 4b) in a 40-year-old man who was in a motor vehicle accident and underwent emergency segmental resection of the right lobe. Note the sharply demarcated wedge-shaped area of infarction; hence, the classification as grade 4.
-
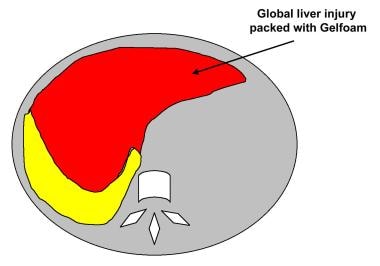
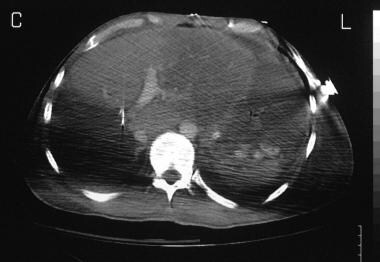
Grade 5 - Global destruction or devascularization of the liver (see the images below).
 Grade 5 injury in a 36-year-old man who was involved in a motor vehicle accident demonstrates global injury to the liver. Bleeding from the liver was controlled by using Gelfoam.
Grade 5 injury in a 36-year-old man who was involved in a motor vehicle accident demonstrates global injury to the liver. Bleeding from the liver was controlled by using Gelfoam.
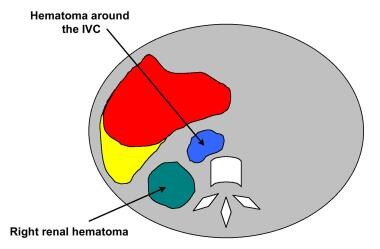
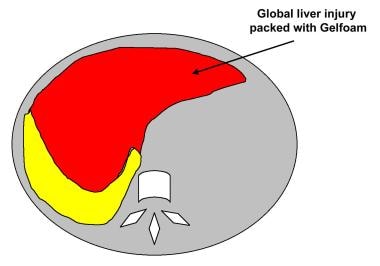 Grade 5 injury in a 36-year-old man who was involved in a motor vehicle accident. Diagram of the CT scan in the previous image.
Grade 5 injury in a 36-year-old man who was involved in a motor vehicle accident. Diagram of the CT scan in the previous image.
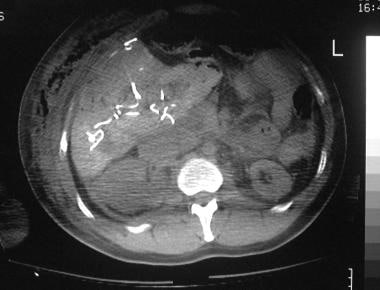
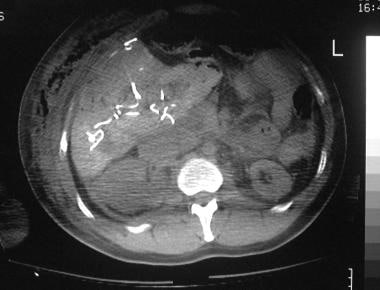 Grade 5 injury in a 36-year-old man who was involved in a motor vehicle accident (same patient as in the 2 previous images). Axial CT scan shows a hematoma around the right kidney and inferior vena cava consistent with renal and inferior vena cava injury.
Grade 5 injury in a 36-year-old man who was involved in a motor vehicle accident (same patient as in the 2 previous images). Axial CT scan shows a hematoma around the right kidney and inferior vena cava consistent with renal and inferior vena cava injury.
-
Grade 6 - Hepatic avulsion.
Subcapsular hematoma
Subcapsular hematoma is usually seen in a lenticular configuration; most subcapsular hematomas are anterolateral to the right lobe of the liver. Subcapsular hematomas cause direct compression and deformity of the shape of the underlying liver.
On nonenhanced CT scans, the liver appears hyperattenuating compared to a subcapsular hematoma. [25] On enhanced CT scans, a subcapsular hematoma appears as a low-attenuating, lenticular collection between the liver capsule and the enhancing liver parenchyma.
Unless bleeding recurs, attenuation of the subcapsular hematoma decreases with time. Subcapsular hematomas resolve within 6-8 weeks.
Intraparenchymal hematomas
On contrast-enhanced CT scans, acute hematomas appear as irregular, high-attenuation areas, which represent clotted blood, surrounded by low-attenuating unclotted blood or bile. Over time, the attenuation of the hematoma is reduced, and the hematoma eventually forms a well-defined serous fluid collection that may expand slightly. A focal, intrahepatic, hyperattenuating area with attenuation of 80-350 HU may represent an active hemorrhage or pseudoaneurysm.
Focal or diffuse periportal low attenuation is believed to be secondary to tracking of blood around the portal vessels, although other possibilities include bile leaks, edema, and dilated periportal lymphatics resulting from increased central venous pressure or injury to the lymphatics.
A low-attenuating periportal collar is seen in children with nonhepatic blunt abdominal trauma, as well as in the absence of intra-abdominal injury. Thus, without other ancillary findings within the liver, the presence of a low-attenuating periportal collar is not indicative of hepatic injury. However, the presence of this sign in documented abdominal trauma correlates with the severity of trauma, physiologic instability, and a higher mortality rate.
CT scan findings in approximately 25% of children with blunt abdominal trauma show periportal low attenuation. That only 40% of these children have evidence of liver injury has been shown.
Laceration
Laceration of the liver appears as a nonenhancing linear or branching structure, usually at the liver periphery. Acute lacerations have a sharp or jagged margin, but with time, lacerations may enlarge, and the margins may develop rolled edges.
Multiple parallel lacerations occur as result of compressive forces (bear claw lacerations). Lacerations may communicate with hepatic vessels and/or biliary radicles.
Vascular injuries
Injuries to the major hepatic veins and the retrohepatic inferior vena cava are uncommon after blunt abdominal trauma.
Retrohepatic vena caval injuries are suggested on CT scans when lacerations extend into the major hepatic veins and the inferior vena cava or when profuse retrohepatic hemorrhage extends into the lesser sac or near the diaphragm.
Perihilar liver tissue may become partially devascularized by a deep laceration or complete avulsion of the dual hepatic blood supply. These devascularized areas of the liver appear as wedge-shaped regions extending toward the liver periphery, and they fail to enhance after the administration of contrast material.
Pseudoaneurysms are better depicted by using spiral or multisection CT scanning because of the ability to image during peak contrast enhancement.
Acute hemorrhage
Acute, intrahepatic hemorrhage is seen as irregular areas of contrast agent extravasation.
Measurement of attenuation values is useful in differentiating extravasated contrast from hematoma. Extravasated contrast material has an attenuation value of 85-350 HU (mean, 132 HU), whereas hemorrhage has an attenuation value of 40-70 HU (mean, 51 HU).
CT scans can be useful in depicting recurrent bleeding after surgery or radiologic intervention.
Gallbladder injury
Gallbladder injury is uncommon, occurring in 2-8% patients with blunt liver trauma. Prior to the availability of CT scanning and ultrasonography, gallbladder injuries were rarely diagnosed before surgery. [26]
CT findings in gallbladder injuries include ill-defined or irregular wall contour, pericholecystic or subserosal fluid, collapsed gallbladder, wall thickening, intraluminal blood, free intraluminal mucosal flap, contrast enhancement of the gallbladder wall or mucosa, free intraperitoneal fluid iso-attenuating with bile, mass effect on the duodenum, and displacement of the gallbladder toward the midline.
Biloma and bile peritonitis
As a result of the slow rate of leaking, a biloma may take weeks or months to develop after trauma; hence, it usually is diagnosed by using follow-up scans. CT scan findings of a posttraumatic biloma demonstrate a cystic structure of low attenuation in or around the liver. Bilomas may contain debris or septa.
Bile peritonitis is an uncommon complication of blunt liver trauma. CT scan findings of bile peritonitis include persistence or increasing amounts of low-attenuating, free peritoneal fluid and thickening of a peritoneum that shows evidence of enhancement.
Degree of confidence
CT scanning is the mainstay of diagnosis of hepatic injuries following blunt trauma; initial CT scan findings help in determining the type of treatment required. With the use of high-speed, spiral CT scans, predicting the necessity of operative treatment or angiography is possible in patients with blunt hepatic injury before deterioration of their hemodynamic state.
A finding of pooled contrast material within the peritoneal cavity indicates active and massive bleeding; patients with this finding may require emergency surgery. [27] Intrahepatic pooling of contrast material with an intact liver capsule usually indicates a self-limiting hemorrhage; most patients with this finding can be treated conservatively.
CT scanning has been proven to be extremely useful in helping to make therapeutic decisions in hepatic trauma and in helping to reduce laparotomy rates in as many as 70% patients at the time of initial evaluation.
False positives/negatives
False-positive errors in the diagnosis of liver injury with CT scans may occur as a result of beam-hardening artifacts from adjacent ribs, which can mimic contusion or hematoma. An air-contrast level within the stomach in a patient with a nasogastric tube can produce streak artifacts throughout the left lobe of the liver; these may mimic intrahepatic lacerations and/or hemorrhage. The nature of these artifacts can be confirmed if the patient is scanned in a decubitus position.
False-negative findings may occur in the setting of a fatty liver only when contrast-enhanced CT scans are obtained. On these images, the enhanced fatty liver may become iso-attenuating relative to the laceration or hematoma. In this situation, a nonenhanced CT scan may provide useful information regarding hepatic injury. Focal fatty infiltration may also mimic hepatic hematoma, laceration, or infarction. Hepatic lacerations with a branching pattern can mimic nonopacified portal or hepatic veins or dilated intrahepatic bile ducts. Careful evaluation of all branching intrahepatic structures is important, and the diagnosis is made with serial images to differentiate the various structures.
Small amounts of free intraperitoneal blood or fluid in the perihepatic space may mimic a subcapsular hematoma; however, these fluid collections usually do not compress the liver parenchyma. CT scans do not always help in predicting which patients require laparotomy. [28] Hematomas or hemorrhage within the liver can occur with a nontraumatic etiology.
In the evaluation of recurrent hepatic bleeding, particularly after an angiographic intervention, nonenhanced and enhanced scans are important to distinguish extravasated contrast material during angiography from recurrent, ongoing hemorrhage. Other hepatic lesions that may mimic active bleeding on CT scans include calcified liver masses and hemangiomas.
Magnetic Resonance Imaging
MRI has a limited role in the evaluation of blunt abdominal trauma, and it has no advantage over CT scanning. Theoretically, MRI can be used in follow-up monitoring of patients with blunt abdominal trauma, and the modality may be useful in young and pregnant women with abdominal trauma in whom the radiation dose is a concern. [29]
MRCP has been used in the assessment of pancreatic duct trauma and its sequelae, and it can be used to image biliary trauma. [19] Another potential use of MRI is in patients with renal failure and in patients who are allergic to radiographic contrast medium.
Ultrasonography
Ultrasonograms can demonstrate a number of traumatic lesions, such as hematomas, contusions, bilomas, and hemoperitoneum. [30, 31]
Extended-focused abdominal sonography for trauma (E-FAST) has been shown to provide rapid detection of intra-abdominal free fluid. [11, 32]
According to the ACR, a radiography trauma series and US FAST scan of the chest, abdomen, and pelvis are usually appropriate for initial imaging of major blunt trauma in hemodynamically unstable patients, and whole-body CT with IV contrast, a radiography trauma series, and US FAST scan of the chest, abdomen, and pelvis are usually appropriate for initial imaging of major blunt trauma in hemodynamically stable patients. [12]
(See the images below of ultrasounds of the liver.)
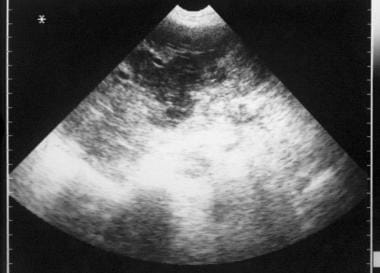 Sonogram of the liver in a 62-year-old woman with a history of recent liver biopsy. The scan shows a loculated anechoic collection in the liver; whether this finding represents a biloma or a hematoma is not clear on this scan.
Sonogram of the liver in a 62-year-old woman with a history of recent liver biopsy. The scan shows a loculated anechoic collection in the liver; whether this finding represents a biloma or a hematoma is not clear on this scan.
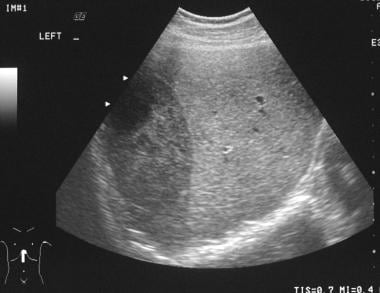 Abdominal sonogram in a 35-year-old male bouncer after blunt abdominal injury shows a crescent-shaped hyperechoic collection along the right lateral aspect of the liver consistent with subcapsular hematoma.
Abdominal sonogram in a 35-year-old male bouncer after blunt abdominal injury shows a crescent-shaped hyperechoic collection along the right lateral aspect of the liver consistent with subcapsular hematoma.
Hepatic hematomas are grouped into 3 categories, as follows:
-
Rupture into the liver and its capsule
-
Separation of the capsule by a subcapsular hematoma
-
Central hepatic ruptures
A subcapsular hematoma usually appears as a curvilinear fluid collection; its echogenicity varies with age. Initially, hematomas are anechoic, becoming progressively more echogenic over the course of 24 hours. With the passage of time, echogenicity of the hematoma once again begins to decrease, and within 4-5 days, the hematoma becomes hypoechoic or anechoic.
Septa and internal echoes often develop within the hemorrhagic collection by 1-4 weeks. Appearances of hepatic laceration change with time. Lacerations appear slightly echogenic, becoming hypoechoic or cystic when scanned days after the injury.
Similar to hematomas, contusions usually are hypoechoic initially, becoming transiently hyperechoic and then hypoechoic. The most common ultrasonographic pattern observed with liver parenchymal injuries is a discrete hyperechoic area; however, a diffuse hyperechoic and occasionally a discrete hypoechoic pattern may be observed. [25, 30]
An echogenic clot often is seen surrounding the liver, and hypoechoic fluid may be observed in other parts of the abdomen.
Bilomas appear as rounded or ellipsoid, anechoic, loculated structures that are fairly well defined in close proximity to the liver and bile duct. Diaphragmatic ruptures appear as a discontinuous line of echoes.
A number of studies have suggested that ultrasonography can replace the invasive procedure of peritoneal lavage in the evaluation of blunt abdominal trauma.
Degree of confidence
Focused assessment performed by using ultrasonography in patients with liver trauma is still investigational for evaluation of blunt and penetrating abdominal trauma. [31] The primary advantage is immediate availability in emergency departments. Some centers use ultrasonography as the initial examination. Patients who are unstable and have a large amount of fluid detected on ultrasonograms are immediately transported for surgery. In addition, patients at these centers who are stable and who have a large amount of intra-abdominal fluid also may be immediately treated with surgery.
An alternative approach is followed in other centers. If ultrasonographic findings are positive for intra-abdominal fluid, CT scanning is the next step. If fluid is not demonstrated on abdominal ultrasonograms, the patient is observed for 12 hours; however, if abdominal pain persists, the patient undergoes CT scanning.
Ultrasonography is the initial examination of choice in the pediatric age group because of the modality's nonionizing and noninvasive nature. Ultrasonography is particularly useful in imaging neonates who are ill and in whom the clinical condition is too unstable to allow transport to a CT scanning facility but who may have a hepatic hematoma after a traumatic delivery or resuscitative efforts.
In a neonate with a decreasing hematocrit level and increasing abdominal distention, ultrasonography may rapidly help in confirming a diagnosis of liver trauma. Because most children with hepatic trauma are treated conservatively, most children can be monitored by using ultrasonography.
Ultrasonography has several advantages over peritoneal lavage in the diagnosis of blunt abdominal trauma. Ultrasonography is a noninvasive procedure that is readily available at the patient's bedside and is less expensive to perform than peritoneal lavage. However, although ultrasonography may be useful in most patients with blunt abdominal trauma, pitfalls remain.
False positives/negatives
Injury to the liver, especially at the dome or lateral segment of the left lobe of the liver, can easily be missed with ultrasonography, particularly in the presence of ileus or when pain makes the examination difficult. The sensitivity of ultrasonography in the detection of free abdominal fluid associated with bowel or mesenteric injury has been reported as only 44%. Blunt abdominal injury may involve organs other than the liver, and these injuries must be detected reliably.
Ultrasonograms may not directly depict injuries to the bowel, mesentery, pancreas, diaphragm, adrenal gland, and bone. Ultrasonography is probably limited in the detection of many vascular injuries as well. A hepatic laceration may be initially difficult to detect, but it may become obvious with the passage of time.
Hepatic hemorrhage may occur as a result of causes other than trauma, including sickle cell anemia, liver tumors, coagulopathies, organ phosphate toxicity, and collagen vascular disease. It may also occur in patients receiving long-term hemodialysis. Hepatic hemorrhage and rupture may occur in eclampsia, pre-eclampsia during the third trimester of pregnancy, HELLP syndrome (hemolysis, elevated liver enzymes, low platelets), hepatic adenoma, and hepatocellular carcinoma.
Nuclear Imaging
Prior to the widespread availability of CT scanning, technetium-99m (99mTc) sulfur colloid or 99mTc-labeled denatured red blood cell studies were widely used in the evaluation of patients with blunt hepatic and splenic trauma. The primary limitations of radionuclides are the nonspecific findings and an inability to evaluate other intraperitoneal and retroperitoneal organs. Despite the disadvantages, radionuclide techniques can offer an important imaging alternative in patients in whom CT scanning cannot be performed, such as those patients in whom the use of intravenous and oral contrast is contraindicated, those who cannot hold their breath, and those who have metallic objects or surgical clips in the abdominal cavity (see the images below).
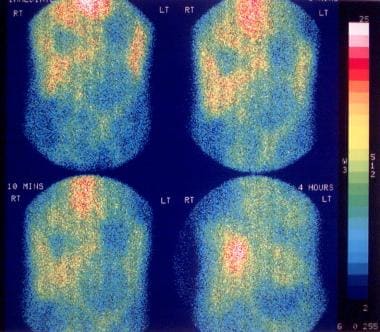 A 62-year-old woman with a history of recent liver biopsy. Technetium-99m iminodiacetic acid (IDA) scan obtained immediately after the injection of the radioisotope shows a large filling defect in the liver, which showed subsequent filling in the 4-hour image consistent with biloma.
A 62-year-old woman with a history of recent liver biopsy. Technetium-99m iminodiacetic acid (IDA) scan obtained immediately after the injection of the radioisotope shows a large filling defect in the liver, which showed subsequent filling in the 4-hour image consistent with biloma.
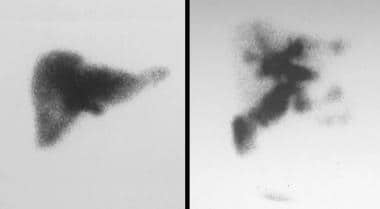 Technetium-99m iminodiacetic acid (IDA) scan in a 30-year-old man who sustained liver injury in a motor vehicle accident. The scan was obtained 1 month later and shows extravasation of the isotope from the biliary tract; this is consistent with a bile leak. Note the relative photon deficiency of the right lobe, which is due to liver contusion.
Technetium-99m iminodiacetic acid (IDA) scan in a 30-year-old man who sustained liver injury in a motor vehicle accident. The scan was obtained 1 month later and shows extravasation of the isotope from the biliary tract; this is consistent with a bile leak. Note the relative photon deficiency of the right lobe, which is due to liver contusion.
Patients who have documented evidence of hepatic or splenic trauma can be monitored noninvasively by using 99mTc sulfur colloid scanning. Most patients with liver trauma show complete or partial resolution of the colloid defects over a period of 3-6 months. However, defects within the spleen may persist indefinitely and do not necessarily indicate a poor prognosis. Whether defects in the liver have similar connotations is uncertain.
After splenic rupture, splenic tissue can become implanted in the peritoneal or intrathoracic cavities (splenosis). Splenosis may be difficult to differentiate from other masses, such as lymphadenopathy, on subsequent scans obtained by using cross-sectional imaging, particularly when scans are performed remote in time from the injury. Uptake with 99mTc sulfur colloid or 99mTc-labeled denatured red cells provides a tissue-specific diagnosis of ectopic splenic tissue.
Labeled red cells may be used to detect the site of active intraperitoneal or retroperitoneal hemorrhage, although quantitating the size of the hemorrhage is difficult using this technique.
Bile duct and/or gallbladder injuries occur in 5% of patients with blunt abdominal trauma. Moreover, biliary injuries may not be identified pre-operatively or may remain unidentified for weeks or months after trauma.
Although CT scanning remains the examination of choice in the evaluation of liver trauma, the procedure of choice to evaluate bile leaks is 99mTc iminodiacetic acid (IDA) scanning. CT scanning and ultrasonography can help detect intra-abdominal fluid, but differentiation between loculated ascitic fluid and hematoma, abscess, and biloma may not be always possible. Scanning for 99mTc IDA uptake usually is performed as a dynamic study immediately after the injection of the radionuclide. The angiographic phase can provide important information regarding vascular injuries and associated renal injury, which may subsequently be missed on static scans.
Following the dynamic study, a 20-minute static scan of the liver is obtained in several planes; in appropriate circumstances, scans can be obtained for as long as 24 hours.
Bile leaks are demonstrated as extravasated activity shortly after administration of the radionuclide. Bilomas are demonstrated initially as a photon-deficient mass that shows activity on delayed scans. In the detection of bilomas, delayed images are essential (2-24 hr); otherwise bilomas may be missed.
Degree of confidence
In patients with blunt trauma, there is an inability to evaluate other sites of abdominal injury and to quantitate intraperitoneal and retroperitoneal hemorrhage. However, in patients in whom a bile leak or biloma is suspected, 99mTc IDA uptake imaging is the examination of choice; this provides a noninvasive technique for arriving at a specific diagnosis.
Focal defects identified with 99mTc sulfur colloid scanning or in the angiographic/hepatic phase of 99mTc IDA scanning may not be related to the trauma; these defects may instead represent simple liver cysts, granulomas, pseudotumors, abscesses, or tumors unrelated to trauma. If delayed scans are not performed, bilomas and bile leaks may be missed using 99mTc IDA scans. Delayed imaging not only provides time for the activity to accumulate within the biloma but also allows clearing of the isotope from the liver, increasing the target-to-background ratio of activity.
Angiography
Most patients with liver trauma who present to the emergency department in shock have positive results after peritoneal lavage and require immediate laparotomy to control hemorrhage. Angiography has no role in the evaluation of these patients. However, patients with less severe trauma may be difficult to evaluate at clinical examination and at laparotomy.
If the patient is stable, cross-sectional imaging may provide sufficient detail to treat the patient conservatively. A dynamic angiographic study may demonstrate the site of active bleeding, providing an opportunity for transcatheter embolization, which may be the only treatment required (see the images below).
 Selective celiac arteriogram of a grade 1 hepatic injury in a 21-year-old man with a stabbing injury to the right upper quadrant of the abdomen. The image shows a focal area of hemorrhage in the right lobe of the liver (arrow) due to the stabbing injury. The well-demarcated filling defect seen in the lateral aspect of the right lobe of the liver is due to compression of normal liver parenchyma by the subcapsular hematoma.
Selective celiac arteriogram of a grade 1 hepatic injury in a 21-year-old man with a stabbing injury to the right upper quadrant of the abdomen. The image shows a focal area of hemorrhage in the right lobe of the liver (arrow) due to the stabbing injury. The well-demarcated filling defect seen in the lateral aspect of the right lobe of the liver is due to compression of normal liver parenchyma by the subcapsular hematoma.
 Postembolization selective arteriogram of a grade 1 hepatic injury in a 21-year-old man with a stabbing injury to the right upper quadrant of the abdomen (same patient as in the previous image). The image shows cessation of the bleeding in the right lobe of the liver.
Postembolization selective arteriogram of a grade 1 hepatic injury in a 21-year-old man with a stabbing injury to the right upper quadrant of the abdomen (same patient as in the previous image). The image shows cessation of the bleeding in the right lobe of the liver.
 A 20-year-old man with systemic lupus erythematosus presented with grade 2 liver injury after minor blunt abdominal trauma. Selective celiac artery arteriogram shows multiple microaneurysms due to systemic lupus erythematosus. Note the parenchymal filling defects due to contusion and medial displacement of the right liver margin due to subcapsular hematoma.
A 20-year-old man with systemic lupus erythematosus presented with grade 2 liver injury after minor blunt abdominal trauma. Selective celiac artery arteriogram shows multiple microaneurysms due to systemic lupus erythematosus. Note the parenchymal filling defects due to contusion and medial displacement of the right liver margin due to subcapsular hematoma.
Liver contusion
Angiographic findings in patients with liver contusion include the following:
-
Stretching and elongation of arterial branches around an avascular mass may be observed.
-
Delay in hepatic blood flow to the involved segments may occur.
-
A transient attenuation difference in uninvolved segments may be depicted.
-
Mottled accumulation of contrast material in the parenchymal phase may be noted.
-
The portal venous phase may confirm a parenchymal defect.
-
Peripheral portal venous filling may be unusually well demonstrated in the presence of contusions.
Liver lacerations
Angiographic findings in patients with liver lacerations include the following:
-
Arterial collaterals may bypass arterial occlusions.
-
Contrast material extravasation may occur.
-
Discrete lacerations may appear as linear or complex lucent defects.
-
Intrahepatic hematomas may appear as poorly defined lucent defects.
-
Arterioportal fistulas may be obvious.
-
Contrast material may pass into the biliary tree, identifying the site of hemobilia.
Subcapsular hematoma
Angiographic findings in patients with subcapsular hematoma include the following:
-
Subcapsular hematomas compress normal parenchyma and may appear as sharply defined, lucent defects against the increased contrast accumulation in the compressed parenchyma.
-
Arterial displacement may be seen.
-
Contrast material extravasation may occur.
High-velocity bullet injuries
Angiographic findings in patients with high-velocity bullet injuries include the following:
-
High-velocity bullets tend to cause burst injuries with distant contusions and parenchymal disruption.
-
Occasionally, these injuries are associated with aortic and renal injuries.
-
All of the angiographic findings of blunt liver trauma can be seen in this group of patients.
Low-velocity penetrating injuries (stab wounds, liver biopsy, and biliary drainage TIPS procedure)
Angiographic findings in patients with low-velocity penetrating injuries include the following:
-
Arterial aneurysms and arterial pseudo-aneurysms
-
Arteriovenous fistulas
-
Hematomas
Degree of confidence
Evaluating the extent of liver injury at surgery may be difficult; in fact, identifying the lesion within the liver may occasionally be impossible. Emergency hepatic angiography should be performed if at all feasible, because it not only documents the injury and helps to evaluate complications, such as pseudo-aneurysms, subcapsular hematoma, or hemobilia, but also provides access for transcatheter embolization.
Although angiography is useful in selected patients, false-positive and false-negative results occur in patients with hepatic trauma.
Liver rupture may be spontaneous or may occur as result of liver tumors, HELLP syndrome, simple cysts, amebic abscess, and hydatid cysts. Intrahepatic arterial aneurysms may be congenital or may be related to vasculitides.
-
Grade 1 hepatic injury in a 21-year-old man with a stabbing injury to the right upper quadrant of the abdomen. Axial, contrast-enhanced computed tomography (CT) scan demonstrates a small, crescent-shaped subcapsular and parenchymal hematoma less than 1 cm thick.
-
Grade 1 hepatic injury in a 21-year-old man with a stabbing injury to the right upper quadrant of the abdomen. Diagram of the CT scan in the previous image.
-
Selective celiac arteriogram of a grade 1 hepatic injury in a 21-year-old man with a stabbing injury to the right upper quadrant of the abdomen. The image shows a focal area of hemorrhage in the right lobe of the liver (arrow) due to the stabbing injury. The well-demarcated filling defect seen in the lateral aspect of the right lobe of the liver is due to compression of normal liver parenchyma by the subcapsular hematoma.
-
Postembolization selective arteriogram of a grade 1 hepatic injury in a 21-year-old man with a stabbing injury to the right upper quadrant of the abdomen (same patient as in the previous image). The image shows cessation of the bleeding in the right lobe of the liver.
-
A 20-year-old man with systemic lupus erythematosus presented with grade 2 liver injury after minor blunt abdominal trauma. Nonenhanced axial CT scan at the level of the hepatic veins shows a subcapsular hematoma 3 cm thick.
-
A 20-year-old man with systemic lupus erythematosus presented with grade 2 liver injury after minor blunt abdominal trauma. Diagram of the CT scan in the previous image.
-
A 20-year-old man with systemic lupus erythematosus presented with grade 2 liver injury after minor blunt abdominal trauma (same patient as in the previous 2 images). Axial CT image through the inferior aspect of the right lobe of the liver demonstrates multiple low-attenuation lesions in the liver consistent with parenchymal contusion.
-
A 20-year-old man with systemic lupus erythematosus presented with grade 2 liver injury after minor blunt abdominal trauma (same patient as in the previous 3 images). Diagram of the CT scan in the previous image.
-
A 20-year-old man with systemic lupus erythematosus presented with grade 2 liver injury after minor blunt abdominal trauma. Selective celiac artery arteriogram shows multiple microaneurysms due to systemic lupus erythematosus. Note the parenchymal filling defects due to contusion and medial displacement of the right liver margin due to subcapsular hematoma.
-
Grade 3 liver injury in a 22-year-old woman after blunt abdominal trauma. Contrast-enhanced axial CT scan through the upper abdomen shows a 4-cm-thick subcapsular hematoma associated with parenchymal hematoma and laceration in segments 6 and 7 of the right lobe of the liver. Free fluid is seen around the spleen and left lobe of the liver consistent with hemoperitoneum.
-
Grade 3 liver injury in a 22-year-old woman after blunt abdominal trauma. Diagram of the CT scan in the previous image.
-
Grade 3 liver injury in a young male patient who fell off a bike. Transaxial CT scan shows 5-cm-thick subcapsular and parenchymal hematoma containing high-density clotted and low-density unclotted blood.
-
Grade 3 liver injury in a young male patient who fell off a bike (same patient as in the previous image). CT scan was obtained 2 months after the initial injury. The subscapular and intraparenchymal hematoma has organized, showing homogeneous low attenuation.
-
Abdominal sonogram in a 35-year-old male bouncer after blunt abdominal injury shows a crescent-shaped hyperechoic collection along the right lateral aspect of the liver consistent with subcapsular hematoma.
-
Image obtained in a 35-year-old male bouncer after blunt abdominal injury. Nonenhanced axial CT scan of the abdomen demonstrates a large subcapsular hematoma measuring more than 10 cm. The high-attenuating areas within the lesion represent clotted blood. The injury was classified as a grade 4 liver injury.
-
Image in a 35-year-old male bouncer after blunt abdominal injury (same patient as in the previous image). Diagram of the CT scan in Image above.
-
Image in a 35-year-old male bouncer after blunt abdominal. Sonogram of the liver obtained 5 months after the injury demonstrates a well-defined, relatively hypoechoic, subacute or chronic subcapsular hematoma.
-
Contrast-enhanced axial CT scan in a 39-year-old man with a grade 4 liver injury shows a large parenchymal hematoma in segments 6 and 7 of the liver with evidence of an active bleed. Note the capsular laceration and large hemoperitoneum.
-
Diagram of the CT scan in Image above in a 39-year-old man with a grade 4 liver injury shows a large parenchymal hematoma in segments 6 and 7 of the liver with evidence of an active bleed.
-
Multisegment infarct (segments 2, 3, 4a, and 4b) in a 40-year-old man who was in a motor vehicle accident and underwent emergency segmental resection of the right lobe. Note the sharply demarcated wedge-shaped area of infarction; hence, the classification as grade 4.
-
Multisegment infarct (segments 2, 3, 4a, and 4b) in a 40-year-old man who was in a motor vehicle accident and underwent emergency segmental resection of the right lobe. Diagram of the CT scan in the previous image.
-
Axial CT scan in a 40-year-old woman with a grade 4 injury demonstrates a right lobar parenchymal contusion.
-
CT section through the kidneys in a 40-year-old woman with a grade 4 injury shows associated subcapsular hematoma of the right kidney.
-
Grade 5 injury in a 36-year-old man who was involved in a motor vehicle accident demonstrates global injury to the liver. Bleeding from the liver was controlled by using Gelfoam.
-
Grade 5 injury in a 36-year-old man who was involved in a motor vehicle accident. Diagram of the CT scan in the previous image.
-
Grade 5 injury in a 36-year-old man who was involved in a motor vehicle accident (same patient as in the 2 previous images). Axial CT scan shows a hematoma around the right kidney and inferior vena cava consistent with renal and inferior vena cava injury.
-
Grade 5 injury in a 36-year-old man who was involved in a motor vehicle accident (same patient as in the previous 3 images). Diagram of the CT scan in the previous image.
-
Contrast-enhanced axial CT scan in a grade 3 liver injury in a 21-year-old woman. A deep laceration extends from the periphery of the liver to the hilum, damaging the adjacent gallbladder.
-
Grade 3 liver injury in a 21-year-old woman. Nonenhanced abdominal CT scan demonstrates a high-density hemorrhage within the gallbladder due to associated gallbladder injury.
-
Sonogram of the liver in a 62-year-old woman with a history of recent liver biopsy. The scan shows a loculated anechoic collection in the liver; whether this finding represents a biloma or a hematoma is not clear on this scan.
-
A 62-year-old woman with a history of recent liver biopsy. Technetium-99m iminodiacetic acid (IDA) scan obtained immediately after the injection of the radioisotope shows a large filling defect in the liver, which showed subsequent filling in the 4-hour image consistent with biloma.
-
Technetium-99m iminodiacetic acid (IDA) scan in a 30-year-old man who sustained liver injury in a motor vehicle accident. The scan was obtained 1 month later and shows extravasation of the isotope from the biliary tract; this is consistent with a bile leak. Note the relative photon deficiency of the right lobe, which is due to liver contusion.