Practice Essentials
The definition of intrauterine growth restriction (IUGR) is a problematic one because we do not know the inherent growth potential of the fetus. The most common definition used is fetal weight below the 10th percentile for gestational age. The preferred method for evaluating intrauterine growth retardation (intrauterine growth restriction; IUGR) is ultrasonographic examination. In most cases of fetal growth restriction, the transcerebellar diameter appears to be spared and can be used as an unbiased measure of gestational age. The transcerebellar diameter in millimeters is equal to gestational age in weeks to 22 weeks of gestation. With this definition, IUGR and "small for gestational age" are synonymous terms. [1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13]
Intrauterine growth restriction has a prevalence of 10% for all pregnancies. However, the figure varies in different patient populations, with rates of 3-5% for healthy mothers and 25% or higher for some high-risk groups, such as hypertensive mothers. Growth-restricted pregnancies are often complicated by a high rate of antepartum and intrapartum fetal distress and the need for cesarean delivery. Infants who are small for their gestational dates are predisposed to low APGAR scores, low cord pH, intraventricular hemorrhage, necrotizing enterocolitis, hypoglycemia, hypocalcemia, and polycythemia.
(See the images below.)
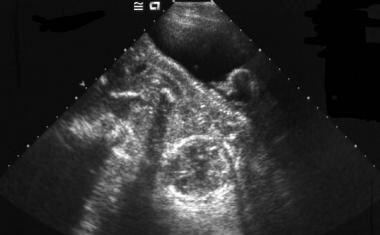 Transabdominal sonogram of an intrauterine pregnancy with marked oligohydramnios associated with intrauterine growth retardation. It is difficult to appreciate the fetal anatomy in the presence of oligohydramnios.
Transabdominal sonogram of an intrauterine pregnancy with marked oligohydramnios associated with intrauterine growth retardation. It is difficult to appreciate the fetal anatomy in the presence of oligohydramnios.
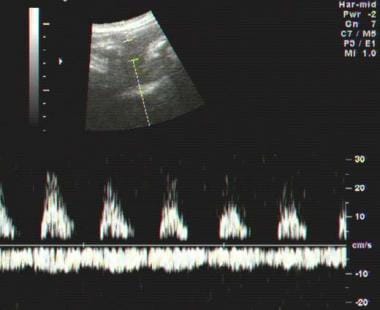 Spectral Doppler waveform of umbilical artery in intrauterine growth retardation (IUGR) demonstrates loss of diastolic flow. Pulsatility of the umbilical vein can also be seen. Both of these findings suggest severe IUGR, and when seen, a perinatologist should be immediately informed.
Spectral Doppler waveform of umbilical artery in intrauterine growth retardation (IUGR) demonstrates loss of diastolic flow. Pulsatility of the umbilical vein can also be seen. Both of these findings suggest severe IUGR, and when seen, a perinatologist should be immediately informed.
The American College of Radiology recommends ultrasound as the initial imaging modality to screen pregnant women for IUGR. For those found to have growth restriction, the ACR notes that duplex Doppler velocimetry of the umbilical artery and a biophysical profile are usually appropropriate. [14] Doppler velocimetry measures hemodynamic flow of major fetal vessels, allowing comparison of the flow indices and patterns of normal and IUGR cases. The most frequently studied vessel in Doppler velocimetry is the umbilical artery because of its accessibility and association with fetal outcome. [15]
To screen for IUGR, ACOG recommends ultrasonography. ACOG describes 4 biometric measures to be used to generate an estimated fetal weight: biparietal diameter, head circumference, abdominal circumference, and femur length. If the estimated fetal weight is below the 10th percentile for gestational age, they suggest that further evaluation be considered, such as amniotic fluid assessment and Doppler blood flow studies of the umbilical artery. Because growth-restricted fetuses have a high incidence of structural and genetic abnormalities, an ultrasonographic examination of fetal anatomy also is recommended. [16]
Melchiorre et al found that there is a significant relationship between first-trimester uterine artery Doppler resistance indices (RI) and the subsequent delivery of neonates who are small for gestational age (SGA) or have intrauterine growth restriction. They found, however, that the sensitivity of first-trimester uterine artery Doppler is greater for SGA with preeclampsia than it is for IUGR alone and noted that this difference could be the result of different underlying placental abnormalities that are detected variably on first-trimester uterine artery Doppler evaluation. [2]
Scifres et al found that oligohydramnios (amniotic fluid index < 5) and abnormal umbilical artery Dopplers (absent or reverse end-diastolic flow) had modest predictive value for perinatal mortality. [17] The authors evaluated whether maternal demographic and ultrasound parameters predict perinatal mortality (in utero death or neonatal death within the first 28 days of life) in preterm IUGR (delivery gestational age < 35 weeks and birth weight < 10th percentile for gestation). Two hundred thirty singleton pregnancies with preterm IUGR meeting the study inclusion criteria were identified.
In a prospective study by Bastek et al of 93 women with severe preeclampsia and ultrasound 3 weeks or less before delivery, current ultrasound practice was noted to have moderately good positive and negative predictive values and a high specificity for the diagnosis of IUGR in women with severe preeclampsia. However, according to the authors, the poor sensitivity (56.7%) and low positive likelihood ratio (8.9) indicate that additional modalities are needed to improve the usefulness of ultrasound in detecting IUGR in severe preeclampsia. [3]
Ultrasonography
Doppler study of the umbilical artery can be done anywhere along the length of the umbilical artery. One should try to obtain as vertical view as possible on the umbilical artery. Blood in the main uterine arteries flows in a direction opposite that in the iliac arteries. The typical waveform shows a deep notch in relation to the closure of the aortic valve. The notch that is present before pregnancy gradually disappears during pregnancy, and diastolic flow increases with advancing gestation (ie, the vessel resistance decreases). [1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13]
Fetal weight below the 10th percentile has a negative predictive value of 99%, a sensitivity of 89%, and a specificity of 88% for the detection of IUGR. [18] An elevated HC/AC (head circumference to abdominal circumference) ratio has a negative predictive value of 98%, a sensitivity of 82%, and a specificity of 94% for the detection of IUGR. Decreased weight with decreased amniotic fluid and the presence of hypertension are good predictors of IUGR.
The triplex mode is used for the evaluation of the umbilical venous blood flow. This mode includes color Doppler sonography of the umbilical vein, pulsed Doppler velocimetry, and real-time sonography to measure the diameter of the umbilical vein. [4, 5, 6, 7]
(See the ultrasound images below.)
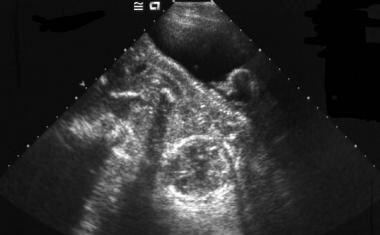 Transabdominal sonogram of an intrauterine pregnancy with marked oligohydramnios associated with intrauterine growth retardation. It is difficult to appreciate the fetal anatomy in the presence of oligohydramnios.
Transabdominal sonogram of an intrauterine pregnancy with marked oligohydramnios associated with intrauterine growth retardation. It is difficult to appreciate the fetal anatomy in the presence of oligohydramnios.
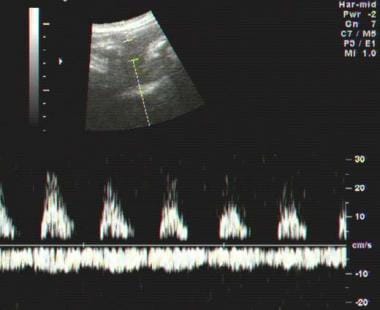 Spectral Doppler waveform of umbilical artery in intrauterine growth retardation (IUGR) demonstrates loss of diastolic flow. Pulsatility of the umbilical vein can also be seen. Both of these findings suggest severe IUGR, and when seen, a perinatologist should be immediately informed.
Spectral Doppler waveform of umbilical artery in intrauterine growth retardation (IUGR) demonstrates loss of diastolic flow. Pulsatility of the umbilical vein can also be seen. Both of these findings suggest severe IUGR, and when seen, a perinatologist should be immediately informed.
Several clinical and ultrasonographic parameters can be used in combination to establish the diagnosis of intrauterine growth retardation (intrauterine growth restriction; IUGR) with greater certainty. The key parameters for diagnosing IUGR are estimated fetal weight, volume of amniotic fluid, and mother's blood pressure status.
Sonographic criteria for IUGR
The sonographic criteria for IUGR include the following:
-
An elevated ratio of femoral length to abdominal circumference (AC)
-
An elevated ratio of head circumference (HC) to AC
-
Unexplained oligohydramnios
The AC measurement is the best single measurement to assess fetal growth because, in growth curtailment, the liver is virtually always affected. Hadlock charts can be used to calculate the fetal weight from the AC. [19] Most ultrasonography machines also use the Hadlock method of calculating fetal weight. The literature describes at least 47 formulas for the estimation of fetal weight. Using the Shepard formula (AC and biparietal diameter [BPD]), one can come within 5% of the true fetal weight and within 10% of the fetal weight 80% of the time. However, 20% of the time, the estimation of the fetal weight may be discrepant by more than 10%.
Oligohydramnios is an indicator of IUGR. Amniotic fluid of less than 5 cm, as measured in the 4 quadrants, is suggestive of oligohydramnios. Other causes of oligohydramnios include death in utero, renal agenesis, and premature rupture of membranes.
The rationale for performing a Doppler study in the diagnosis of IUGR is that many cases of growth restriction are thought to be associated with small vessel disease in the fetoplacental or uteroplacental circulation. Numerous Doppler criteria have been proposed for diagnosing IUGR. These involve at least 3 of the following waveform indices:
-
Systolic/diastolic (S/D) ratio
-
Pulsatility index (PI)
-
Resistive index (RI)
-
Spectral waveform of the umbilical, uterine, and fetal internal carotid arteries and the fetal descending thoracic aorta
-
Spectral waveform of the ductus venosus and inferior vena cava
Abnormal findings on Doppler waveforms include the following:
-
Highest uterine artery PI – lowest uterine artery PI greater than 1.1
-
Persistence of protodiastolic notch, unilateral or bilateral, after 23 weeks is suggestive of IUGR or preeclampsia
-
RI greater than 0.55 with bilateral notches
-
RI greater than 0.65 with a unilateral notch
-
RI greater than 0.70 with or without notches
-
RI greater than 90th percentile for a given gestational age regardless of notches
An S/D ratio greater than 3 after 30 weeks' gestation is abnormal.
The reversal of flow in ductus venosus is suggestive of a fetus with severely compromised IUGR and reflects fetal metabolic acidemia.
Umbilical blood flow
Umbilical venous blood flow, both absolute flow (in mm/min) and corrected blood flow (in mL/min/kg) are reduced in IUGR. The presence of pulsations in umbilical vein waveform between 8 and 12 weeks is normal, and its persistence is abnormal. The presence of umbilical vein pulsations is associated with an increased risk of an adverse perinatal outcome.
-
Transabdominal sonogram of an intrauterine pregnancy with marked oligohydramnios associated with intrauterine growth retardation. It is difficult to appreciate the fetal anatomy in the presence of oligohydramnios.
-
Normal spectral Doppler waveform of umbilical artery and vein in a near-term fetus.
-
Spectral Doppler waveform of umbilical artery in intrauterine growth retardation (IUGR) demonstrates loss of diastolic flow. Pulsatility of the umbilical vein can also be seen. Both of these findings suggest severe IUGR, and when seen, a perinatologist should be immediately informed.









