Practice Essentials
Primary hyperparathyroidism affects approximately 0.3% of the population, with about 90% of patients having a single parathyroid adenoma and 10% having multigland hyperplasia or multiple adenomas. In rare cases, patients are found to have parathyroid carcinoma. [1, 2] Primary hyperparathyroidism is the most common cause of hypercalcemia in the outpatient population, and it is second only to malignancy as an etiology of hypercalcemia in the inpatient population. [3]
In 1891, von Recklinghausen described the classic bone disease termed osteitis fibrosa cystica. In 1925, the Viennese surgeon Mandl performed the first parathyroid exploration and adenoma resection. Mandl noted improvement of the patient's severe skeletal abnormalities postoperatively, thereby linking hyperparathyroidism with bone disease. Albright later described the clinical entity of classic primary hyperparathyroidism in the 1930s on the basis of 17 cases from his clinical practice. [4]
Historically, the disorder was marked by characteristic skeletal changes, nephrolithiasis, and neuromuscular dysfunction. [5] Primary hyperparathyroidism is now a different entity. Since the advent of chemical screening with an autoanalyzer in the 1960s, most cases are discovered in asymptomatic patients with hypercalcemia. [6, 7, 8, 9]
Primary hyperparathyroidism is predominant in postmenopausal women, with a female-to-male ratio of 3-4:1. Also, the disease is common in areas where biochemical screening is utilized, such as North America and Western Europe. but is seen much less frequently where such screening is not commonly available, such as India. [10, 11, 12]
The clinical presentation of primary hyperparathyroidism includes target organ involvement of the renal and skeletal systems; mild asymptomatic hypercalcemia; and high parathyroid hormone (PTH) levels with persistently normal albumin-corrected and ionized serum calcium values. When biochemical screening is available, asymptomatic primary hyperparathyroidism is the most likely presentation. In areas where vitamin D deficiency is prevalent and biochemical screening is not available, symptomatic disease with skeletal abnormalities is more likely. [13, 10, 11]
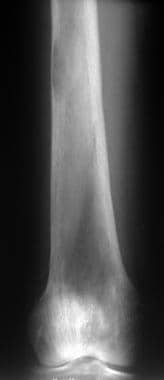
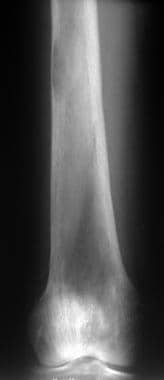
(See the radiograph showing hyperparathyroidism below.)
 Radiograph of the proximal tibia and fibula. Diffuse demineralization attributed to trabecular resorption is the most common plain radiographic sign of primary hyperparathyroidism.
Radiograph of the proximal tibia and fibula. Diffuse demineralization attributed to trabecular resorption is the most common plain radiographic sign of primary hyperparathyroidism.
Imaging modalities
The 2 most commonly used imaging modalities are cervical sonography and technetium-99m-sestamibi (99mTC MIBI) tomoscintigraphy. To image the parathyroid glands before a repeat operation for recurrent or persistent disease, 99mTc MIBI scanning and magnetic resonance imaging (MRI) are the preferred imaging modalities because of their high sensitivities in depicting ectopic or mediastinal glands. [14] Tc-99m MIBI imaging has a sensitivity of 70-95% in depicting parathyroid tumors, and this modality allows 3-dimensional (3D) imaging with anterior-to-posterior localization of the tumor. Studies have revealed equal sensitivities of 99mTc MIBI imaging and MRI in the localization of abnormal glands before a repeat surgery, with sensitivities of 82-85%. By combining the 2 modalities, the sensitivity increases to 94%. The limitations of MIBI scintigraphy include reduced sensitivity in patients who have multiglandular lesions or small lesions, as well as low levels of parathyroid hormone. [15, 16, 17, 18, 19, 20, 21, 22, 23, 14, 24, 25]
Ultrasonography may be preferred for initial preoperative tumor localization, if desired by the surgeon, because of this technique's low risk, low cost, and high sensitivity in depicting parathyroid glands that are not ectopic or in the mediastinum. [26, 27, 28, 29]
However, many surgeons believe that the initial 4-gland exploration enables a 95% cure rate with little morbidity and that initial preoperative localization provides no improvement in the outcome. Some surgeons advocate initial localization to guide directed dissection, obviating bilateral exploration. Opponents argue that the sensitivities of imaging modalities are not sufficient and that parathyroid glands can be missed in an unacceptable number of patients.
Fluorine-18 (18F) fluorocholine (FCH) PET/MR imaging has been show to provide localization of adenomas with high accuracy when ultrasound or Tc-99m MIBI scintigraphy results are negative or inconclusive. [30]
The diagnosis of primary hyperparathyroidism is made by means of the laboratory confirmation of an elevated PTH level in the setting of hypercalcemia. [31]
The 2 most commonly used imaging modalities are cervical sonography and Tc-99m-sestamibi (MIBI) tomoscintigraphy. The limitations of MIBI scintigraphy include reduced sensitivity in patients who have multiglandular lesions or small lesions, as well as low levels of parathyroid hormone.
A retrospective study by Benjamin et al of the use of 18F-choline PET/CT in preoperative detection of parathyroid adenoma in 215 primary hyperparathyroidism patients (269 glands) showed that 18F-choline PET/CT performed favorably as a second-line imaging method, with SUVmax, lesion size, and unilocularity predicting a high correlation between the 18F-choline PET/cCT and surgical findings. The 8F-choline PET/CT detected 240 glands as having pathological findings. The mean SUVmax was 3.76 ± 2.34 (0–18.5), and the mean lesion size was 10.70 ± 7.99 (0–53) mm. [32, 33, 14]
In a study, by Dudoignon et al, comparing the sensitivity and accuracy of 18F-fluorocholine PET/CT, cervical ultrasound (CUS), and 99mTc-MIBI scintigraphy for detection of abnormal parathyroid glands in 51 patients, sensitivity and accuracy were 76% and 76% for 18-F fluorocholine PET/CT; 71% and 71% for CUS; and 33% and 33% for 99mTc-MIBI scintigraphy. However, sensitivity for the combination of all 3 was 94%. [34]
Radiographs may yield the most specific findings that are consistent with the disorder, and radiography is the preferred examination when the clinical findings suggest primary hyperparathyroidism. Radiographs of the hands may yield the diagnostic finding of subperiosteal resorption, which is virtually pathognomonic for the disease. (See the images below.)
 Bilateral anteroposterior (AP) radiographic views of the hands in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) and primary hyperparathyroidism. These images show subperiosteal bone resorption along the radial aspects of the middle phalanges.
Bilateral anteroposterior (AP) radiographic views of the hands in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) and primary hyperparathyroidism. These images show subperiosteal bone resorption along the radial aspects of the middle phalanges.
 Anteroposterior radiographic view of the right hand in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) and primary hyperparathyroidism (same patient as in the previous image). This image shows subperiosteal bone resorption along the radial aspects of the middle phalanges (arrows).
Anteroposterior radiographic view of the right hand in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) and primary hyperparathyroidism (same patient as in the previous image). This image shows subperiosteal bone resorption along the radial aspects of the middle phalanges (arrows).
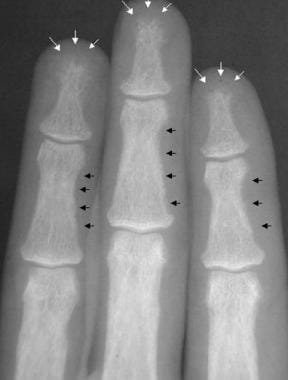 Radiograph of the middle phalanges in a patient with primary hyperparathyroidism. This image demonstrates subperiosteal resorption that has resulted in severe tuftal resorption (white arrows). Also, note the subperiosteal and intracortical resorption of the middle phalanges (black arrows).
Radiograph of the middle phalanges in a patient with primary hyperparathyroidism. This image demonstrates subperiosteal resorption that has resulted in severe tuftal resorption (white arrows). Also, note the subperiosteal and intracortical resorption of the middle phalanges (black arrows).
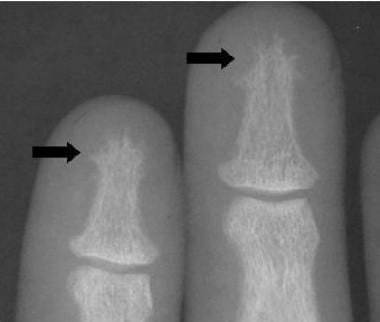 Radiograph of the phalanges in a patient with primary hyperparathyroidism. This image demonstrates subperiosteal resorption that has resulted in severe tuftal resorption (arrows).
Radiograph of the phalanges in a patient with primary hyperparathyroidism. This image demonstrates subperiosteal resorption that has resulted in severe tuftal resorption (arrows).
If radiographs of the hands reveal no abnormalities, other sites are unlikely to demonstrate abnormal findings. Dual-energy x-ray absorptiometry (DXA) and quantitative CT (QCT) scanning may provide evidence of osteoporosis that is consistent with the diagnosis; however, the finding is nonspecific for primary hyperparathyroidism.
Annual monitoring of calcium and PTH along with DXA imaging has been proposed for patients with asymptomatic primary hyperparathyrodism. [31]
Limitations of techniques
Radiographs of the hand may yield the pathognomonic finding of subperiosteal resorption, which is consistent with a diagnosis of primary hyperparathyroidism. However, other findings on radiographs are not specific for this disorder. In addition, DXA and QCT scanning are the preferred diagnostic modalities for the evaluation of osteoporosis, which is one of the most common findings in patients with primary hyperparathyroidism. However, osteoporosis may be associated with a host of other diagnoses; therefore, the specificity of this condition may be limited.
The diagnosis of primary hyperparathyroidism is primarily based on the laboratory confirmation of elevated PTH concentrations in the setting of an increased calcium level.
American Association of Endocrine Surgeons Guidelines
The American Association of Endocrine Surgeons has published the following guidelines regarding primary hyperparathyroidism [35]
-
Initial evaluation should include 25-hydroxyvitamin D measurement, 24-hour urine calcium measurement, dual-energy x-ray absorptiometry, and supplementation for vitamin D deficiency.
-
Parathyroidectomy is indicated for all symptomatic patients, should be considered for most asymptomatic patients, and is more cost-effective than observation or pharmacologic therapy.
-
Cervical ultrasonography or other high-resolution imaging is recommended for operative planning. Patients with nonlocalizing imaging remain surgical candidates.
-
Preoperative parathyroid biopsy should be avoided.
-
Both focused, image-guided surgery (minimally invasive parathyroidectomy) and bilateral exploration are appropriate operations that achieve high cure rates.
-
For minimally invasive parathyroidectomy, intraoperative parathyroid hormone monitoring via a reliable protocol is recommended.
-
Minimally invasive parathyroidectomy is not routinely recommended for known or suspected multigland disease.
-
Ex vivo aspiration of resected parathyroid tissue may be used to confirm parathyroid tissue intraoperatively.
-
Clinically relevant thyroid disease should be assessed preoperatively and managed during parathyroidectomy.
-
Devascularized normal parathyroid tissue should be autotransplanted.
-
Patients should be observed postoperatively for hematoma, evaluated for hypocalcemia and symptoms of hypocalcemia, and followed up to assess for cure defined as eucalcemia at more than 6 months.
-
Calcium supplementation may be indicated postoperatively.
-
Familial pHPT, reoperative parathyroidectomy, and parathyroid carcinoma are challenging entities that require special consideration and expertise.
Radiography
Hyperparathyroidism is a disease of increased bone resorption and bone formation. Subsequently, plain radiographic findings may include resorption and sclerosis of numerous sites in the skeletal system.
Historically, osteitis fibrosa cystica was used to describe the advanced skeletal disease in primary hyperparathyroidism. Bone findings were characterized by the osteoclastic resorption of bone, osteoblastic bone formation, and fibrous replacement of marrow, with radiographic findings of subperiosteal resorption, brown tumors, [36] bone cysts, and sclerosis.
The most common radiologic finding in primary hyperparathyroidism is osteopenia, which may be generalized or asymmetric. Fine trabeculations are initially lost, with resultant coarse and thickened trabeculae. The disease may progress with further destruction that results in a ground-glass appearance in the trabeculae. About 30-50% of the bone density must be lost to show changes on radiographs. Other methods for the quantification of bone density, such as QCT scanning and DXA, are more sensitive in the evaluation of osteopenia.
Additional findings include bone resorption, which may occur at many different anatomic sites. Bone resorption may be classified as subperiosteal, intracortical, trabecular, endosteal, subchondral, subligamentous, or subtendinous. Subperiosteal bone resorption is an early and virtually pathognomonic sign of hyperparathyroidism, and this finding is marked by marginal erosions with adjacent resorption of bone and sclerosis. An unusual lacelike appearance may be seen beneath the periosteum with an occasional spiculated external cortex. The underlying resorptive process may progress to complete cortical disappearance.
Although subperiosteal bone resorption can affect many sites, the most common site in hyperparathyroidism is the middle phalanges of the index and middle fingers, primarily on the radial aspect (see the images below).
 Bilateral anteroposterior (AP) radiographic views of the hands in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) and primary hyperparathyroidism. These images show subperiosteal bone resorption along the radial aspects of the middle phalanges.
Bilateral anteroposterior (AP) radiographic views of the hands in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) and primary hyperparathyroidism. These images show subperiosteal bone resorption along the radial aspects of the middle phalanges.
 Anteroposterior radiographic view of the right hand in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) and primary hyperparathyroidism (same patient as in the previous image). This image shows subperiosteal bone resorption along the radial aspects of the middle phalanges (arrows).
Anteroposterior radiographic view of the right hand in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) and primary hyperparathyroidism (same patient as in the previous image). This image shows subperiosteal bone resorption along the radial aspects of the middle phalanges (arrows).
Other sites of subperiosteal resorption include the phalangeal tufts (acro-osteolysis), the lamina dura around the teeth, the medial aspect of the tibia, the humerus, the femur, and the distal clavicle. For depictions of these sites, see the images below. When the resorption extends to the margins of joints, particularly in the hands, wrists, and feet, findings may appear articular.
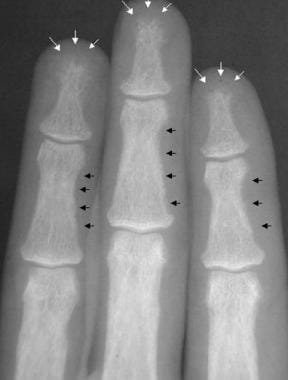 Radiograph of the middle phalanges in a patient with primary hyperparathyroidism. This image demonstrates subperiosteal resorption that has resulted in severe tuftal resorption (white arrows). Also, note the subperiosteal and intracortical resorption of the middle phalanges (black arrows).
Radiograph of the middle phalanges in a patient with primary hyperparathyroidism. This image demonstrates subperiosteal resorption that has resulted in severe tuftal resorption (white arrows). Also, note the subperiosteal and intracortical resorption of the middle phalanges (black arrows).
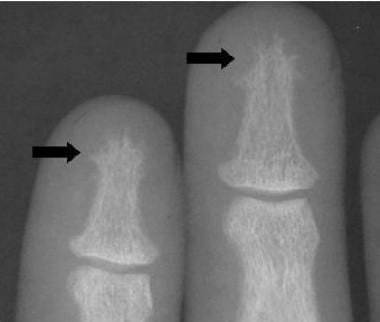 Radiograph of the phalanges in a patient with primary hyperparathyroidism. This image demonstrates subperiosteal resorption that has resulted in severe tuftal resorption (arrows).
Radiograph of the phalanges in a patient with primary hyperparathyroidism. This image demonstrates subperiosteal resorption that has resulted in severe tuftal resorption (arrows).
 Anteroposterior radiographic view of the left shoulder in external rotation in a patient with primary hyperparathyroidism. This image shows the healing stage of marked subperiosteal resorption (arrow) of the medial aspect of the proximal humerus.
Anteroposterior radiographic view of the left shoulder in external rotation in a patient with primary hyperparathyroidism. This image shows the healing stage of marked subperiosteal resorption (arrow) of the medial aspect of the proximal humerus.
 Radiograph of the proximal humerus in a patient with primary hyperparathyroidism (same patient as in the previous image). This image shows the healing stage of marked subperiosteal resorption of the medial aspect of the proximal humerus. A subsequent fracture through the surgical neck of the humerus is also depicted.
Radiograph of the proximal humerus in a patient with primary hyperparathyroidism (same patient as in the previous image). This image shows the healing stage of marked subperiosteal resorption of the medial aspect of the proximal humerus. A subsequent fracture through the surgical neck of the humerus is also depicted.
 Radiograph of the distal femur in a patient with primary hyperparathyroidism. This image shows scalloped defects along the inner margin of the cortex, which denote endosteal resorption.
Radiograph of the distal femur in a patient with primary hyperparathyroidism. This image shows scalloped defects along the inner margin of the cortex, which denote endosteal resorption.
 Radiograph of the femur in primary hyperparathyroidism (same patient as in the previous image). This image shows scalloped defects along the inner margin of the femoral cortex (arrows), which denote endosteal resorption.
Radiograph of the femur in primary hyperparathyroidism (same patient as in the previous image). This image shows scalloped defects along the inner margin of the femoral cortex (arrows), which denote endosteal resorption.
 Radiograph of the shoulder in a patient with primary hyperparathyroidism. This image depicts subperiosteal distal clavicular resorption (arrows).
Radiograph of the shoulder in a patient with primary hyperparathyroidism. This image depicts subperiosteal distal clavicular resorption (arrows).
 Radiograph of the shoulder in a patient with primary hyperparathyroidism. This image demonstrates distal clavicular resorption.
Radiograph of the shoulder in a patient with primary hyperparathyroidism. This image demonstrates distal clavicular resorption.
Other areas of resorption, such as cortical or endosteal regions, are usually accompanied by subperiosteal findings. Intracortical bone resorption is an indicator of rapid bone turnover and is described as linearly oriented striations in the cortex. The linear lucencies are produced by resorption of bone in the haversian canals and are best seen on the cortical surface of the second metacarpal.
Trabecular bone resorption may occur throughout the skeleton and usually accompanies advanced disease. In the skull, areas of decreased radiopacity are intermingled with sclerotic radiopaque areas, resulting in a classic appearance called the salt-and-pepper skull (see the image below).
 Anteroposterior radiographic view of the top of the calvarium in a patient with primary hyperparathyroidism. This image shows trabecular bone resorption that has resulted in the salt-and-pepper appearance of the calvarium.
Anteroposterior radiographic view of the top of the calvarium in a patient with primary hyperparathyroidism. This image shows trabecular bone resorption that has resulted in the salt-and-pepper appearance of the calvarium.
In endosteal resorption, the medullary cavity widens, with thinning of the inner cortex (see the images below). Changes are usually best seen in the hands and appear as scalloped lucencies on the inner aspect of the bony cortex. Endosteal changes are usually accompanied by subperiosteal or cortical resorption.
 Radiograph of the distal femur in a patient with primary hyperparathyroidism. This image shows scalloped defects along the inner margin of the cortex, which denote endosteal resorption.
Radiograph of the distal femur in a patient with primary hyperparathyroidism. This image shows scalloped defects along the inner margin of the cortex, which denote endosteal resorption.
 Radiograph of the femur in primary hyperparathyroidism (same patient as in the previous image). This image shows scalloped defects along the inner margin of the femoral cortex (arrows), which denote endosteal resorption.
Radiograph of the femur in primary hyperparathyroidism (same patient as in the previous image). This image shows scalloped defects along the inner margin of the femoral cortex (arrows), which denote endosteal resorption.
Subchondral bone resorption is most common in the joints of the axial skeleton, such as the sacroiliac, acromioclavicular (see the image below), discovertebral, sternoclavicular, and symphysis pubis, but it may also occur in the joints of the appendicular skeleton. Subchondral bone is resorbed; collapse with subsequent new bone formation and fibrous replacement may result.
 Anteroposterior radiographic view of the clavicles. This image shows symmetric subchondral bone resorption of the acromioclavicular joints. Distal clavicular resorption can be subperiosteal or subchondral, but this finding is not specific for primary hyperparathyroidism.
Anteroposterior radiographic view of the clavicles. This image shows symmetric subchondral bone resorption of the acromioclavicular joints. Distal clavicular resorption can be subperiosteal or subchondral, but this finding is not specific for primary hyperparathyroidism.
On radiographs, areas of subchondral lucency are noted with surrounding sclerosis. In the sacroiliac joint, bilateral findings affect the ilium more than the sacrum and may produce an irregular articular margin with the appearance of a widened joint. At the acromioclavicular joint, bilateral erosions affect the clavicle side more than the acromion, whereas the sternum and clavicle are equally affected at the sternoclavicular joint.
Subligamentous and subtendinous resorption occurs at insertion sites on bones. Common sites are the plantar aspect of the calcaneus, dorsal aspect of the patella, inferior margin of the distal clavicle, trochanters, and ischial and humeral tuberosities.
Brown tumors are well-circumscribed lytic lesions of bone that represent the osteoclastic resorption of a confluent area of bone with subsequent fibrous replacement (see the images below). The lesions may be single or multiple, with expansion of overlying bone, and they may be present in any site, although the lesions usually occur in cortical bone. Common sites include the mandible, clavicle, ribs, pelvis, and femur.
 Radiograph of the humerus in a patient with primary hyperparathyroidism. This image depicts a brown tumor. Note the osseous expansion and lucency of the proximal humerus. Brown tumors can have varied appearances.
Radiograph of the humerus in a patient with primary hyperparathyroidism. This image depicts a brown tumor. Note the osseous expansion and lucency of the proximal humerus. Brown tumors can have varied appearances.
 Radiograph of the mid femoral diaphysis in a patient with primary hyperparathyroidism. This image depicts brown tumors. Note the eccentric (arrowheads) and central positions (arrow) of the lesions.
Radiograph of the mid femoral diaphysis in a patient with primary hyperparathyroidism. This image depicts brown tumors. Note the eccentric (arrowheads) and central positions (arrow) of the lesions.
 Radiograph of the pelvis in a patient with primary hyperparathyroidism. Note the presence of brown tumors in the pelvis.
Radiograph of the pelvis in a patient with primary hyperparathyroidism. Note the presence of brown tumors in the pelvis.
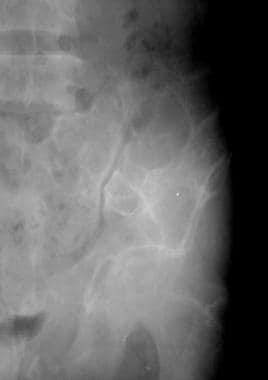 Radiograph of brown tumors of the pelvis in a patient with primary hyperparathyroidism (same patient as in the previous image).
Radiograph of brown tumors of the pelvis in a patient with primary hyperparathyroidism (same patient as in the previous image).
After resection of an adenoma, lesions may become sclerotic on radiographs. Once considered a finding that was characteristic of primary hyperparathyroidism, brown tumors are more common in secondary hyperparathyroidism because of the increasing population and life expectancy of patients undergoing dialysis.
Calcium pyrophosphate dihydrate crystal deposition disease (CPPD) is more common in association with primary hyperparathyroidism than with secondary hyperparathyroidism. Chondrocalcinosis may affect the menisci of the knee, the triangular cartilage of the wrist, and the symphysis pubis. CPPD arthropathy is less common in these patients than in patients with idiopathic disease.
Other radiographic findings in primary hyperparathyroidism include varying degrees of sclerosis, although generalized sclerosis is more common in secondary hyperparathyroidism. Soft-tissue and vascular calcification is more common in secondary disease, as is superior and inferior band sclerosis of the spine, which is called rugger-jersey spine. The laxity of ligaments and tendons primarily affects the sacroiliac and acromioclavicular joints, whereas rupture may be seen at several sites, including the quadriceps, triceps, and patellar tendons.
Degree of confidence
In the setting of elevated serum calcium levels and elevated PTH levels, the diagnosis of primary hyperparathyroidism is certain. However, radiographic findings of subperiosteal resorption are most specific for the disease and should prompt consideration of the primary hyperparathyroidism.
Magnetic Resonance Imaging
MRI is one diagnostic modality that can be used to evaluate ectopic parathyroid adenomas. On T1-weighted images, adenomas appear as low-signal-intensity masses, whereas intermediate or high signal intensity is seen on T2-weighted images. Gadolinium enhancement with fat suppression results in diffuse enhancement of the adenoma. [19, 20, 27, 37, 38]
(See the images below.)
 Technetium-99m sestamibi scan (99mTc MIBI) in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1). This image demonstrates persistent abnormal activity of the inferior right parathyroid gland that is consistent with an adenoma.
Technetium-99m sestamibi scan (99mTc MIBI) in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1). This image demonstrates persistent abnormal activity of the inferior right parathyroid gland that is consistent with an adenoma.
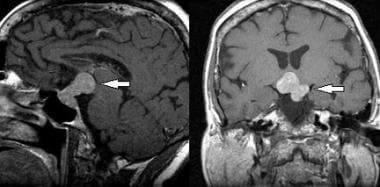 Sagittal (left image) and coronal (right image) T1-weighted magnetic resonance images of the brain in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) (same patient as in the previous image). These images show a pituitary macroadenoma (arrows).
Sagittal (left image) and coronal (right image) T1-weighted magnetic resonance images of the brain in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) (same patient as in the previous image). These images show a pituitary macroadenoma (arrows).
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
MRI findings of brown tumors are nonspecific. Bony expansion can be visualized, and the extent of the lesion can be determined. The imaging characteristics depend on the amount of fibrous tissue, hemorrhage, and cystic changes that are present in the lesion. Lack of an associated soft-tissue mass is a pertinent negative finding that can be demonstrated on MRIs.
Ultrasonography
Ultrasonography is one of the primary modalities used to localize parathyroid tumors. [39, 40] The size of the adenoma is usually correlated with the degree of parathyroid elevation. Adenomas appear as well-defined hypoechoic lesions with potential cystic or necrotic areas. Ultrasonography offers the advantage of depicting potential concomitant thyroid disease, which is present in approximately 40% of patients with parathyroid disease.
Ultrasonography is approximately 75% sensitive in identifying adenomas, but this technique has low sensitivity in identifying ectopic lesions.
In renal imaging, ultrasonography can demonstrate bilateral hyperechoic medullary pyramids that are consistent with medullary nephrocalcinosis; this is a nonspecific finding (see the image below).
 Sonogram of the kidney in a patient with primary hyperparathyroidism. This image shows medullary nephrocalcinosis.
Sonogram of the kidney in a patient with primary hyperparathyroidism. This image shows medullary nephrocalcinosis.
Nuclear Imaging
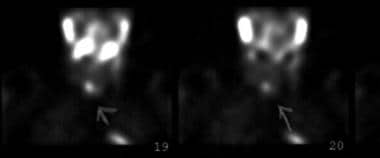
In parathyroid imaging, localization of the parathyroid glands may be accomplished with 99mTc MIBI scanning (see the image below). Both thyroid and parathyroid tissues demonstrate radionuclide uptake, but sestamibi washes out of thyroid tissue early after its injection, leaving only parathyroid tissue that demonstrates activity at 2-4 hours. [21, 22, 23, 40, 37, 41, 42]
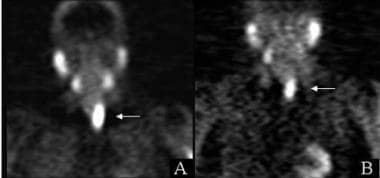 Technetium-99m sestamibi (99mTc MIBI) images in a patient with primary hyperparathyroidism. The initial (A) and 3.5-hour delayed (B) images demonstrate a 6-cm parathyroid adenoma (arrows).
Technetium-99m sestamibi (99mTc MIBI) images in a patient with primary hyperparathyroidism. The initial (A) and 3.5-hour delayed (B) images demonstrate a 6-cm parathyroid adenoma (arrows).
In musculoskeletal imaging, bone densitometry is extremely valuable in assessing primary hyperparathyroidism because it can be used to quantify bone loss, and it may help making predictions regarding the fracture risk (see also the Fracture Index WITH known Bone Mineral Density [BMD] calculator). DXA helps in evaluating the mineral content of all bone in the path of the beam. Bone mineral density is expressed as either a T score, which is based on the standard deviations from a young-adult mean, or as a Z score, which is compared to an age-matched mean. The T score is used to clinically diagnose osteopenia or osteoporosis and to predict the fracture risk. DXA may also be used after an intervention to document improvements in bone density.
The diagnosis of primary hyperparathyroidism is based on biochemical determinations, and bone scanning has a limited role in making the diagnosis. In addition, a few patients with hyperparathyroidism have insufficient disease for its demonstration on bone scans. However, bone scanning may assist in differentiating hyperparathyroidism from metastatic disease in the setting of elevated calcium levels. Because bone turns over significantly in hyperparathyroidism, findings on bone scans include generalized increased radionuclide uptake throughout the skeleton in contrast to soft tissues; this observation is called a superscan. Because the contrast of the skeletal system is increased, renal activity may not be apparent.
In a meta-analysis, by Lee et al, of 119 studies (8495 patients) that used 2 or more imaging modalities, sensitivity of choline PET-CT was found to be significantly higher than that of technetium-99m sestamibi single-photon emission CT (MIBI SPECT). For surface under the cumulative ranking curve (SUCRA) values, choline PET-CT had the highest SUCRA value in both patient-based and lesion-based analyses. In patient-based analysis after 2010, choline PET-CT had the highest SUCRA value, followed by CT. [43]
A retrospective study by Benjamin et al of the use of 18F-choline PET/CT in preoperative detection of parathyroid adenoma in 215 primary hyperparathyroidism patients (269 glands) showed that 18F-choline PET/CT performed favorably as a second-line imaging method, with SUVmax, lesion size, and unilocularity predicting a high correlation between the 18F-choline PET/cCT and surgical findings. The 8F-choline PET/CT detected 240 glands as having pathological findings. The mean SUVmax was 3.76 ± 2.34 (0–18.5), and the mean lesion size was 10.70 ± 7.99 (0–53) mm. [32, 33, 14]
In a study by Christensen et al, 11C-choline PET/CT and dual-isotope subtraction scintigraphy with 99mTc-MIBI/123iodide using SPECT/CT (Di-SPECT) performed equally well in preoperative location of hyperfunctioning parathyroid glands in 90 patients. Sensitivity was 82% for 11C-choline PET/CT and 87% for Di-SPECT. [44]
Computed Tomography
With parathyroid imaging, ectopic adenomas can be assessed by using contrast-enhanced CT scan studies. However, sestamibi and MRI are more sensitive, and these are the imaging studies of choice in most patients (see the images below). [38] In musculoskeletal imaging, QCT scanning is another method of bone densitometry. This modality offers the advantage of selective evaluation of the mineral content in trabecular bone, which makes QCT scanning more sensitive in detecting small changes in bone density.
Studies have shown 4-dimensional CT (4D CT) to have high sensitivity rates in preoperative localization of parathyroid tumors in primary hyperparathyroidism. [45, 46, 47, 48]
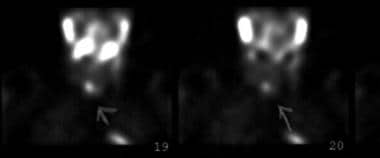 Technetium-99m sestamibi scan (99mTc MIBI) in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1). This image demonstrates persistent abnormal activity of the inferior right parathyroid gland that is consistent with an adenoma.
Technetium-99m sestamibi scan (99mTc MIBI) in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1). This image demonstrates persistent abnormal activity of the inferior right parathyroid gland that is consistent with an adenoma.
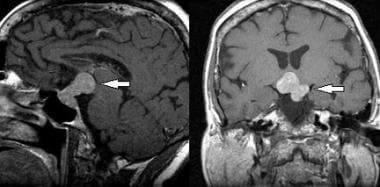 Sagittal (left image) and coronal (right image) T1-weighted magnetic resonance images of the brain in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) (same patient as in the previous image). These images show a pituitary macroadenoma (arrows).
Sagittal (left image) and coronal (right image) T1-weighted magnetic resonance images of the brain in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) (same patient as in the previous image). These images show a pituitary macroadenoma (arrows).
 Computed tomography (CT) scan of the pancreas in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) and a gastrinoma (same patient as in the previous 2 images). This image shows a pancreatic head mass (large white arrow), as well as a low-attenuating lesion in the liver (small black arrowhead) that indicates metastases. Note the calcifications of the right renal medullary pyramids (medullary nephrocalcinosis; black arrows) in this nonenhanced CT scan.
Computed tomography (CT) scan of the pancreas in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) and a gastrinoma (same patient as in the previous 2 images). This image shows a pancreatic head mass (large white arrow), as well as a low-attenuating lesion in the liver (small black arrowhead) that indicates metastases. Note the calcifications of the right renal medullary pyramids (medullary nephrocalcinosis; black arrows) in this nonenhanced CT scan.
Studies of single-photon emission CT( SPECT)/CT versus SPECT alone in detecting preoperative localization of parathyroid adenomas in primary hyperparathyroidism has found fewer fase-negative findings with SPECT/CT than with SPECT alone. The advantage of SPECT/CT over SPECT alone was most apparent for correct lateralization of small adenomas (< 210 mg). [49] SPECT/CT when combined with TC-99m MIBI double-phase scintigraphy has been shown to have a sensitivity of 90% in the presurgical assessement of patients. [50] However, sensitivity was found to be lower for reoperative parathyroidectomy for persistent primary hyperparathryoidism. [51]
-
Radiograph of the proximal tibia and fibula. Diffuse demineralization attributed to trabecular resorption is the most common plain radiographic sign of primary hyperparathyroidism.
-
Bilateral anteroposterior (AP) radiographic views of the hands in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) and primary hyperparathyroidism. These images show subperiosteal bone resorption along the radial aspects of the middle phalanges.
-
Anteroposterior radiographic view of the right hand in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) and primary hyperparathyroidism (same patient as in the previous image). This image shows subperiosteal bone resorption along the radial aspects of the middle phalanges (arrows).
-
Radiograph of the middle phalanges in a patient with primary hyperparathyroidism. This image demonstrates subperiosteal resorption that has resulted in severe tuftal resorption (white arrows). Also, note the subperiosteal and intracortical resorption of the middle phalanges (black arrows).
-
Anteroposterior radiographic view of the left shoulder in external rotation in a patient with primary hyperparathyroidism. This image shows the healing stage of marked subperiosteal resorption (arrow) of the medial aspect of the proximal humerus.
-
Radiograph of the proximal humerus in a patient with primary hyperparathyroidism (same patient as in the previous image). This image shows the healing stage of marked subperiosteal resorption of the medial aspect of the proximal humerus. A subsequent fracture through the surgical neck of the humerus is also depicted.
-
Radiograph of the shoulder in a patient with primary hyperparathyroidism. This image depicts subperiosteal distal clavicular resorption (arrows).
-
Radiograph of the shoulder in a patient with primary hyperparathyroidism. This image demonstrates distal clavicular resorption.
-
Anteroposterior radiographic view of the top of the calvarium in a patient with primary hyperparathyroidism. This image shows trabecular bone resorption that has resulted in the salt-and-pepper appearance of the calvarium.
-
Radiograph of the distal femur in a patient with primary hyperparathyroidism. This image shows scalloped defects along the inner margin of the cortex, which denote endosteal resorption.
-
Radiograph of the femur in primary hyperparathyroidism (same patient as in the previous image). This image shows scalloped defects along the inner margin of the femoral cortex (arrows), which denote endosteal resorption.
-
Anteroposterior radiographic view of the clavicles. This image shows symmetric subchondral bone resorption of the acromioclavicular joints. Distal clavicular resorption can be subperiosteal or subchondral, but this finding is not specific for primary hyperparathyroidism.
-
Radiograph of the humerus in a patient with primary hyperparathyroidism. This image depicts a brown tumor. Note the osseous expansion and lucency of the proximal humerus. Brown tumors can have varied appearances.
-
Radiograph of the mid femoral diaphysis in a patient with primary hyperparathyroidism. This image depicts brown tumors. Note the eccentric (arrowheads) and central positions (arrow) of the lesions.
-
Radiograph of the pelvis in a patient with primary hyperparathyroidism. Note the presence of brown tumors in the pelvis.
-
Radiograph of brown tumors of the pelvis in a patient with primary hyperparathyroidism (same patient as in the previous image).
-
Sonogram of the kidney in a patient with primary hyperparathyroidism. This image shows medullary nephrocalcinosis.
-
Technetium-99m sestamibi (99mTc MIBI) images in a patient with primary hyperparathyroidism. The initial (A) and 3.5-hour delayed (B) images demonstrate a 6-cm parathyroid adenoma (arrows).
-
Technetium-99m sestamibi scan (99mTc MIBI) in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1). This image demonstrates persistent abnormal activity of the inferior right parathyroid gland that is consistent with an adenoma.
-
Sagittal (left image) and coronal (right image) T1-weighted magnetic resonance images of the brain in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) (same patient as in the previous image). These images show a pituitary macroadenoma (arrows).
-
Computed tomography (CT) scan of the pancreas in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) and a gastrinoma (same patient as in the previous 2 images). This image shows a pancreatic head mass (large white arrow), as well as a low-attenuating lesion in the liver (small black arrowhead) that indicates metastases. Note the calcifications of the right renal medullary pyramids (medullary nephrocalcinosis; black arrows) in this nonenhanced CT scan.
-
Indium-111 (111In) octreotide scan in a patient with multiple endocrine neoplasia syndrome type 1 (MEN 1) (same patient as in the previous 3 images). These nuclear images demonstrate abnormal activity in the pituitary macroadenoma (curved arrow), parathyroid adenoma (straight arrow), and gastrinoma metastases throughout the abdomen (arrowheads).
-
Radiograph of the phalanges in a patient with primary hyperparathyroidism. This image demonstrates subperiosteal resorption that has resulted in severe tuftal resorption (arrows).







