Practice Essentials
Herpes simplex encephalitis (HSE) is the most common cause of sporadic viral encephalitis, with a predilection for the temporal lobes and with clinical presentations ranging from aseptic meningitis and fever to a severe rapidly progressive form involving altered consciousness. In adults, herpes simplex virus type 1 (HSV-1) accounts for 95% of all fatal cases of sporadic encephalitis and usually results from reactivation of the latent virus. The clinical findings and neuroimaging appearance are both consistent with spread of the virus from a previously infected ganglion. [1, 2]
Herpes simplex encephalitis has an annual prevalence of 1 in 500,000 cases in the United States. About 50% of the cases of HSE occur in individuals older than 50 years. Delay of treatment with acyclovir may result in permanent neuropsychological impairment and increases mortality from 19% to more than 70%. [3] [2]
Sporadic cases of human herpesvirus 6 (HHV6) have been described in immunocompromised patients or those with lymphoproliferative disorders. In children and neonates, herpes simplex virus type 2 (HSV-2) accounts for 80-90% of neonatal and almost all congenital infections. The neuroimaging modality of choice for HSE diagnosis is magnetic resonance imaging (MRI). Edema, hemorrhage, and necrosis in the inferomedial temporal lobe are common findings. Brain involvement may be unilateral or bilateral. Traditionally on MRI, herpes simplex encephalitis exhibits bilateral asymmetrical involvement of the limbic system, including the medial temporal lobes, insular cortices and inferolateral frontal lobes, and cingulate gyri. [2, 4, 5, 6, 7] Sparing of the basal ganglia is a key feature, which also helps differentiate HSE from middle cerebral artery infarction on diffusion-weighted imaging (DWI). Atypical patterns, if seen, usually affect younger patients, with involvement of the cerebral hemispheres and rarely the midbrain and pons. [1, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19]
Biochemical abnormalities in CSF analysis with positive CSF polymerase chain reaction (PCR) testing confirm the diagnosis. The sensitivity of CSF PCR testing is 98%, and specificity is 94% for the detection of HSV-1 virus in the CSF. [4]
(See the image of herpes encephalitis below.)
On pathology, herpes viruses cause a fulminant hemorrhagic and necrotizing meningoencephalitis, with typical gross findings of severe edema and massive tissue necrosis, with petechial hemorrhages and hemorrhagic necrosis. Often, the petechial hemorrhage is not observed on computed tomography (CT) scanning or MRI. On microscopy, a focal necrotizing vasculitis is observed with perivascular and meningeal lymphocytic infiltration and eosinophilic intranuclear inclusions in glial cells and neurons. Taira et al found that a lower Glasgow Coma Scale score and a greater number of lesions detected on CT scanning were predictors of prolonged acyclovir therapy [20] (see the Glasgow Coma Scale calculator).
Preferred examination
MRI is the preferred modality for evaluating the brain. [21, 22, 23] However, early in the clinical course of the disease, MRI results may be negative. A negative MRI does not rule out HSV encephalitis. Therapy should be empirically continued until laboratory tests definitely exclude the diagnosis. A case report of West Nile Virus causing focal temporal lobe findings was described in the literature. [24]
Early imaging with CT scanning or radionuclide studies may also reveal normal findings. CT scanning may not reveal abnormalities until 3-5 days after symptom onset, by which time the patient may be stuporous and comatose. As noted above, in the acute setting, even contrast-enhanced MRIs may be negative.
Computed Tomography
In adults, CT scans classically reveal hypodensity in the temporal lobes either unilaterally or bilaterally, with or without frontal lobe involvement. Hemorrhage is usually not observed. A gyral or patchy parenchymal pattern of enhancement is observed. Contrast enhancement generally occurs later in the disease process. [22, 25]
The herpes virus preferentially involves the temporal lobe and orbital surfaces of the frontal lobes. This involvement may extend to the insular cortex, posterior occipital cortex, and cerebral convexity; however, the basal ganglia are spared. Bilateral involvement is frequent. Involvement of the cingulate gyrus occurs later in the disease. The classic involvement of the medial temporal and frontal lobes is consistent with intracranial spread along the small meningeal branches of the fifth cranial nerve. Cingulate gyrus involvement may arise from efferent hippocampal connections. A rhomboencephalitis resulting from pontine involvement may occur and likely arises from retrograde viral transmission along the cisternal portion of the trigeminal nerve to the brainstem.
In neonates, involvement is in the periventricular white matter, sparing the medial temporal and inferior frontal lobes. In addition, meningeal enhancement may be observed following contrast. [26, 27]
Taira et al analyzed specific variables as predictors of a need for a prolonged course of acyclovir therapy in 23 patients with HSV encephalitis and reported a lower Glasgow Coma Scale score and a greater number of lesions detected on CT scans were predictors of prolonged therapy [20] (see the Glasgow Coma Scale calculator). The investigators concluded that standard initial ACV treatment may not be sufficient for patients with such predictors and that initial treatment modifications may be necessary in such patients. [20]
Late in the disease process, when temporal and frontal lobe involvement is seen, CT findings may be characteristic. Reports exist of patients with normal CT results and cerebrospinal fluid (CSF) studies in the presence of abnormal MRI and EEG findings, indicating that MRI is more sensitive. Early in the disease process, limited sensitivity of approximately 50% was noted. When typical findings of HSV encephalitis are observed on CT scan, they often are associated with severe brain damage and a poor prognosis. [22]
Because of bone artifact, the temporal lobes can be difficult to assess on CT scanning. Early in the disease process, CT scanning may be normal. Other causes of encephalitis, tumor, or lymphoma may appear similar.
Magnetic Resonance Imaging
The neuroimaging modality of choice for HSE diagnosis is magnetic resonance imaging (MRI). The diagnosis of herpes encephalitis can be strongly suggested by the typical appearance of medial temporal abnormalities that do not respect hippocampal borders. Edema, hemorrhage, and necrosis in the inferomedial temporal lobe are common findings. Brain involvement may be unilateral or bilateral. Traditionally on MRI, herpes simplex encephalitis exhibits bilateral asymmetrical involvement of the limbic system, including the medial temporal lobes, insular cortices and inferolateral frontal lobes, and cingulate gyri. [2, 4, 5, 6, 7] Sparing of the basal ganglia is a key feature, which also helps differentiate HSE from middle cerebral artery infarction on diffusion-weighted imaging (DWI). Atypical patterns, if seen, usually affect younger patients, with involvement of the cerebral hemispheres and rarely the midbrain and pons. [1, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19]
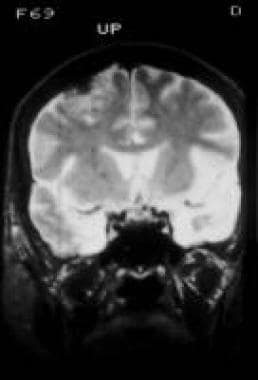
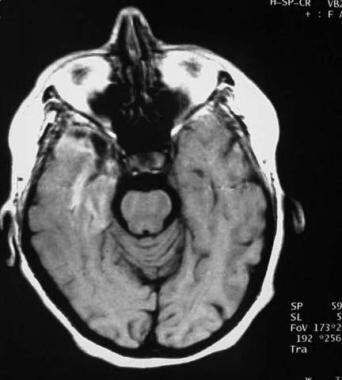
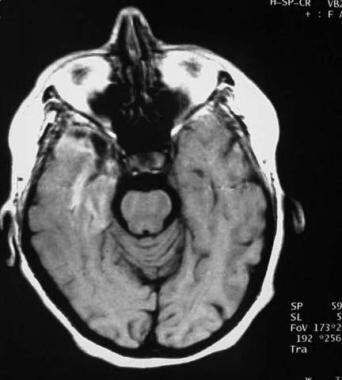
In adults, T2-weighted MRI reveals hyperintensity corresponding to edematous changes in the temporal lobes (see the first 2 images below), inferior frontal lobes, and insula, with a predilection for the medial temporal lobes. Foci of hemorrhage occasionally can be observed on MRI (see the third image below).
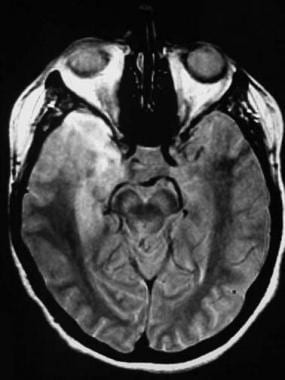 Axial proton density–weighted image in a 62-year-old woman with confusion and herpes encephalitis shows T2 hyperintensity involving the right temporal lobe.
Axial proton density–weighted image in a 62-year-old woman with confusion and herpes encephalitis shows T2 hyperintensity involving the right temporal lobe.
 Axial gadolinium-enhanced T1-weighted image reveals enhancement of the right anterior temporal lobe and parahippocampal gyrus. At the right anterior temporal tip is a hypointense, crescentic region surrounded by enhancement consistent with a small epidural abscess.
Axial gadolinium-enhanced T1-weighted image reveals enhancement of the right anterior temporal lobe and parahippocampal gyrus. At the right anterior temporal tip is a hypointense, crescentic region surrounded by enhancement consistent with a small epidural abscess.
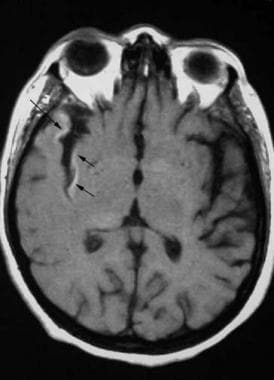 Axial nonenhanced T1-weighted image shows cortical hyperintensity (arrows) consistent with petechial hemorrhage. In general, this is a common pathologic finding but less commonly depicted in herpes encephalitis.
Axial nonenhanced T1-weighted image shows cortical hyperintensity (arrows) consistent with petechial hemorrhage. In general, this is a common pathologic finding but less commonly depicted in herpes encephalitis.
MRI is preferred for imaging and follow-up studies of herpes encephalitis. Typically, temporal lobe T2 hyperintensity spares the basal ganglia. Although this appearance was previously believed to be pathognomonic for herpes involvement, similar findings can be observed in progressive multifocal leukoencephalopathy and primary CNS lymphoma. Patchy parenchymal or gyral enhancement can be observed (see the image below). [28, 29, 30, 31, 32, 33]
 Axial gadolinium-enhanced T1-weighted image reveals enhancement of the right anterior temporal lobe and parahippocampal gyrus. At the right anterior temporal tip is a hypointense, crescentic region surrounded by enhancement consistent with a small epidural abscess.
Axial gadolinium-enhanced T1-weighted image reveals enhancement of the right anterior temporal lobe and parahippocampal gyrus. At the right anterior temporal tip is a hypointense, crescentic region surrounded by enhancement consistent with a small epidural abscess.
In one study of 251 cases of temporal lobe encephalitis identified by MRI, 43% were of an infectious etiology (60 cases were herpes simplex encephalitis) and 16% noninfectious. Therefore, in addition to herpes simplex, other infectious and noninfectious causes should be considered in the differential diagnosis of temporal lobe encephalitis. [34]
Features favoring HSV over other causes include older age, acute clinical presentation, fever, gastrointestinal symptoms, and lower incidences of ataxia. Patients with HSV encephalitis were more likely than those with autoimmune encephalitis to be men and were less likely to have psychosis or rash. On MRI, findings of hemorrhage, enhancement, and restricted diffusion do not differ across the types, although patients with non-HSV encephalitis more frequently have bilateral temporal lesions, as well as lesions outside the temporal lobe and the cingulate and insula areas. [34, 35]
Reports of restricted diffusion in herpes encephalitis exist (see the first image below), with corresponding T2 hyperintensity reflecting edema (see the second image below). Reports suggest diffusion-weighted imaging (DWI) may be more sensitive in the detection of HSV involvement than conventional MRI sequences and may mimic an infarct with involvement of the cortical regions of the temporal lobe. [36]
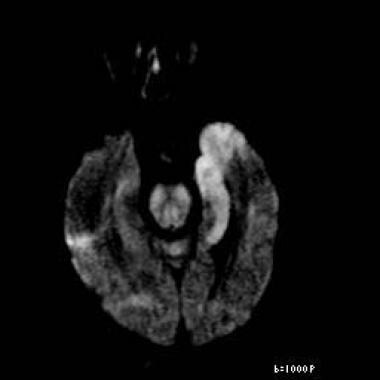 Axial diffusion-weighted image reveals restricted diffusion in the left medial temporal lobe consistent with herpes encephalitis. This patient also had a positive result on polymerase chain reaction assay for herpes simplex virus, which is both sensitive and specific. In addition, the patient had periodic lateralized epileptiform discharges on electroencephalogram, which supports the diagnosis of herpes encephalitis.
Axial diffusion-weighted image reveals restricted diffusion in the left medial temporal lobe consistent with herpes encephalitis. This patient also had a positive result on polymerase chain reaction assay for herpes simplex virus, which is both sensitive and specific. In addition, the patient had periodic lateralized epileptiform discharges on electroencephalogram, which supports the diagnosis of herpes encephalitis.
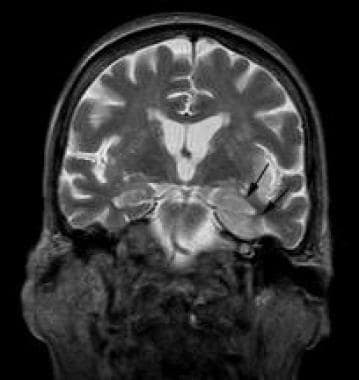 Coronal T2-weighted image reveals hyperintensity in the left temporal lobe (arrows) in a distribution similar to the restricted diffusion abnormality seen in the previous image. This finding is typical for herpes encephalitis. In patients with HHV6 infection, one series noted that in addition to mesial temporal lobe abnormality, abnormal T2 hyperintensity has been seen in the insular and inferior frontal region, which may suggest the diagnosis. There are felt to be 2 typical imaging appearances: one seen in older adults involves T2 hyperintensity confined to the medial temporal lobe; in young adults, a more varied pattern has been described that includes foci of restricted diffusion with an otherwise normal magnetic resonance, diffuse cortical necrosis, or small focal regions of abnormal T2 hyperintensity.
Coronal T2-weighted image reveals hyperintensity in the left temporal lobe (arrows) in a distribution similar to the restricted diffusion abnormality seen in the previous image. This finding is typical for herpes encephalitis. In patients with HHV6 infection, one series noted that in addition to mesial temporal lobe abnormality, abnormal T2 hyperintensity has been seen in the insular and inferior frontal region, which may suggest the diagnosis. There are felt to be 2 typical imaging appearances: one seen in older adults involves T2 hyperintensity confined to the medial temporal lobe; in young adults, a more varied pattern has been described that includes foci of restricted diffusion with an otherwise normal magnetic resonance, diffuse cortical necrosis, or small focal regions of abnormal T2 hyperintensity.
Immunocompromised patients may have atypical manifestations including widespread cortical involvement, brainstem involvement, or cerebellar involvement. [37] In the pediatric population, diffusion-weighted images are thought to be the most sensitive, and the cingulum was less frequently effected when compared with adults. [38]
In neonates, T2-weighted MRI shows hyperintensity of the periventricular white matter, with the medial temporal and inferior frontal lobes spared. Meningeal enhancement also may be observed. [39]
A study of diffusion-weighted MRI for early diagnosis of neonatal HSE by Okanishi et al sought to determine the early changes and evolutions of brain diffusion-weighted imaging (DWI) and analyze prognostic factors of the early changes. The 13 patients selected developed encephalitis within 28 days after birth; had herpes simplex infection; and underwent MRI, including DWI, at 7 days or less of symptom onset. Cortical lesions were the main findings in the early period, and bilateral deep cerebral lesions at 7 days or less were highly indicative of poor motor and cognitive outcomes. DWI frequently showed multiple cortical lesions in both hemispheres in the early period and both hemispheres on DWI (8/9 scans at ≤48 hr, 7/7 patients). With increased time from onset, cortical lesions tended to coincide with subcortical white-matter lesions beneath the initial cortical lesions. Lesions from the cortex extended to the subcortical white matter in 7 patients. Deep cerebral lesions, involving the basal ganglia, internal capsules, and thalamus, were also found in 9 patients at 7 days or less of onset. [40]
Advanced MR techniques are being increasingly used to study herpes encephalitis. MR spectroscopy using proton spectroscopic MRI has demonstrated a reduction of the N -acetylaspartate (NAA)-to-choline ratio. A decreased NAA peak has been reported 7-14 weeks after onset, and in some cases, an elevated choline peak is seen. Occasionally, the lactate peak may be elevated. The NAA decrease is believed to reflect neuronal injury. NAA recovery has been noted to parallel clinical improvement. [41, 42] Diffusion-tensor imaging has an emerging role in delineating areas of involvement of normal-appearing white matter in the contralateral hemisphere to visible lesions. [43]
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). For more information, see the Medscape Reference topic Nephrogenic Systemic Fibrosis. NSF/NFD has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. For more information, see FDA Information on Gadolinium-Based Contrast Agents or Medscape.
-
Magnetic resonance image depicting herpes encephalitis.
-
Axial proton density–weighted image in a 62-year-old woman with confusion and herpes encephalitis shows T2 hyperintensity involving the right temporal lobe.
-
Axial nonenhanced T1-weighted image shows cortical hyperintensity (arrows) consistent with petechial hemorrhage. In general, this is a common pathologic finding but less commonly depicted in herpes encephalitis.
-
Axial gadolinium-enhanced T1-weighted image reveals enhancement of the right anterior temporal lobe and parahippocampal gyrus. At the right anterior temporal tip is a hypointense, crescentic region surrounded by enhancement consistent with a small epidural abscess.
-
Axial diffusion-weighted image reveals restricted diffusion in the left medial temporal lobe consistent with herpes encephalitis. This patient also had a positive result on polymerase chain reaction assay for herpes simplex virus, which is both sensitive and specific. In addition, the patient had periodic lateralized epileptiform discharges on electroencephalogram, which supports the diagnosis of herpes encephalitis.
-
Coronal T2-weighted image reveals hyperintensity in the left temporal lobe (arrows) in a distribution similar to the restricted diffusion abnormality seen in the previous image. This finding is typical for herpes encephalitis. In patients with HHV6 infection, one series noted that in addition to mesial temporal lobe abnormality, abnormal T2 hyperintensity has been seen in the insular and inferior frontal region, which may suggest the diagnosis. There are felt to be 2 typical imaging appearances: one seen in older adults involves T2 hyperintensity confined to the medial temporal lobe; in young adults, a more varied pattern has been described that includes foci of restricted diffusion with an otherwise normal magnetic resonance, diffuse cortical necrosis, or small focal regions of abnormal T2 hyperintensity.