Practice Essentials
Hemangioblastomas are considered to be benign neoplasms (WHO grade I) and represent 1-2.5% of all primary central tumors. [1, 2] Approximately 60-75% of hemangioblastomas are sporadic and 20-40% are associated with von Hippel-Lindau (VHL) disease. [3, 4, 5, 1, 6, 7, 8, 9, 10, 11] In 1927, Arvid Lindau reported the connection between retinal angiomas and hemangiomas of the cerebellum. VHL is an autosomal dominant condition involving chromosome 3 characterized by specific benign and malignant tumors with variable expressivity. [12, 13, 5, 14, 15] Cerebellar hemangioblastoma is the most common initial manifestation, affecting 64% of patients with VHL. [16] In many series, cerebellar hemangioblastoma is the most important cause of mortality, affecting 47.7% of patients with VHL, [17] followed by renal cell carcinoma. [17, 18, 19]
In patients with a positive family history, a single cerebellar hemangioblastoma is sufficient to make the diagnosis. If no known family history exists, at least 2 cerebellar hemangioblastomas or 1 hemangioblastoma plus 1 visceral tumor are necessary to justify the diagnosis of VHL.
The peak age of incidence has been noted to be between 20 and 50 years. Hemangioblastomas are uncommon but not rare in patients older than 65 years. In a study at one institution, all patients (N=77) were older than 18 years, and 6 of those were older than 65 years. [20]
Various organs can be involved. [17] Of patients presenting with hemangioblastomas, 70% do not have a family history, and 3-25% of these patients have tumors associated with VHL. Hemangioblastoma appears to be associated more with VHL than previously reported, and it has been suggested that all patients with sporadic nonhereditary tumors should be evaluated for evidence of VHL disease. [16, 18, 21]
(See the hemangioblastoma images below.)
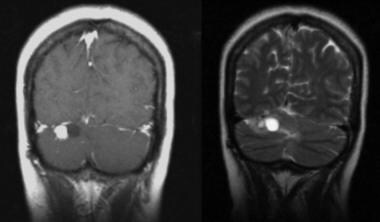
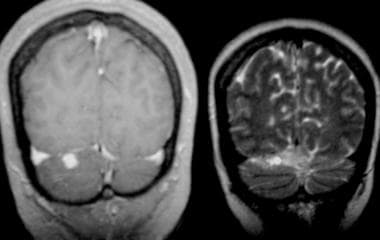 Patient with von Hippel-Lindau disease. T1-weighted gadolinium-enhanced MRI shows an enhancing nodule. Coronal T2-weighted MRI shows a small high-signal-intensity cyst.
Patient with von Hippel-Lindau disease. T1-weighted gadolinium-enhanced MRI shows an enhancing nodule. Coronal T2-weighted MRI shows a small high-signal-intensity cyst.
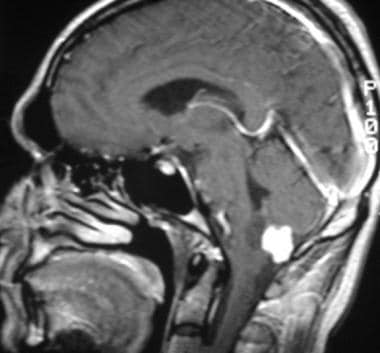 Sagittal T1-weighted gadolinium-enhanced MRI shows a homogeneous intense enhancing tumor in the cistern magna.
Sagittal T1-weighted gadolinium-enhanced MRI shows a homogeneous intense enhancing tumor in the cistern magna.
The nidus of the tumor abuts the pia matter, from which the tumor receives its vascular supply. The tumor is more frequently superficial than deep. Of hemangioblastomas, 60-70% are cystic, and the remainder are solid. Solid tumors are more common in the brainstem and supratentorial locations than elsewhere. The mural nodule is hypervascular and relatively small, less than 15 mm in diameter.
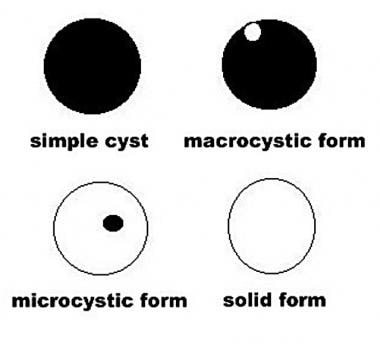
From a macroscopic point of view, hemangioblastomas can appear as solid or cystic tumors with mixed forms. Four types can be distinguished, as follows:
-
Type 1, or the simple cyst form, is rare (6%) and characterized by a cyst with clear fluid and smooth walls and without evidence of a mural nodule at angiography or surgery.
-
Type 2, or the macrocystic form, is the most frequent (65%) and characterized by a cyst of variable size with a mural nodule of approximately 1 cm.
-
Type 3, or the solid form (25%), has a solid consistency with blurred limits and marked vascularization.
-
Type 4, or the microcystic form (4%), is solid but contains small cysts of a few millimeters in size; therefore, 75% of infratentorial hemangioblastomas have a cystic component of variable size (see the image below).
Preferred examination
Contrast-enhanced MRI is considered to be the best method for screening patients with von Hippel-Lindau (VHL) and to be the first evaluation used in symptomatic patients. However, preoperative angiography remains important for defining feeding vessels and aiding in embolization. [22, 23, 24, 25] Before the advent of MRI, contrast-enhanced CT scanning was performed frequently; however, beam-hardening artifacts produced by the petrous and vertebral bone limited its use.
MRI is superior to nonenhanced CT in the detection of vascular components of the tumor. [22, 26] Contrast-enhanced CT has the same sensitivity as nonenhanced MRI; however, it is inferior to contrast-enhanced MRI. [22] Contrast-enhanced MRI permits the identification of small tumor nodules. In addition, MRI is helpful in separating cystic and solid components of the tumor from edema. Patients with VHL should be screened, and follow-up studies should be performed at 6 months.
The sensitivity of MRI increases with the use of gadolinium-based contrast material. Angiography is better in the detection of small (< 1 cm) vascular tumor components, and it is better for showing the vascular nature, supply, and drainage of tumors, as compared to CT. [27] However, CT and MRI depict tumor cysts better. [28]
Use of a gadolinium-based contrast agent is mandatory in the evaluation of hemangioblastomas because it increases the sensitivity for small, solid lesions. [27, 29] When the diagnosis of hemangioblastoma is established, a careful evaluation for other small enhancing lesions should be performed because of the multiple lesions seen in some patients. The presence of multiple lesions has an important impact on the prognosis. [18]
In hemangioblastomas located near the pia, differentiation from meningiomas can be difficult in certain patients. It is always important to look for characteristics that can help in diagnosing a vascular tumor, which is particularly important before surgery. In some patients, complete removal of the mural nodule is enough; however, in patients in whom the transition from solid tumor to cystic tumor with a mural nodule has been observed, the radiologist should perform careful follow-up imaging to assess the behavior of the lesions.
Further follow-up studies should be performed at 1-year intervals to detect the development of additional tumors and monitor progression of existing lesions. [22] Early treatment improves the outcome. Using MRI and CT at 1- to 2-year intervals, Conway et al identified 74% of lesions that required surgery before the patients became symptomatic. [16]
Computed Tomography
On CT scans, the hemangioblastoma tumor appears well circumscribed, solid, or cystic, with a mural nodule. Usually, the nodule is smaller than the cyst. This feature helps in differentiating it from cystic astrocytoma, which tends to have a larger nodule. The cyst is hypoattenuating on CT scans. [30, 31, 32, 33]
In precontrast studies, the nodule is isoattenuating relative to the surrounding brain tissue, but it is hyperattenuating in occasional cases. After the administration of contrast material, the attenuation is equivalent to or higher than that of the straight sinus, and the nodule enhances homogeneously. Commonly, the nodule abuts a pial surface. Multiplanar CT and MRI help in identifying the subpial localization (see the image below).
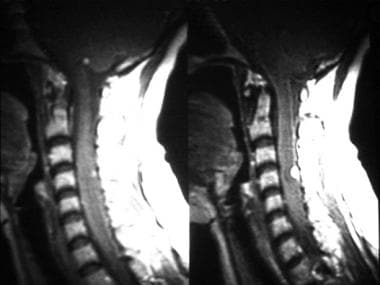 T1-weighted postgadolinium MRI shows 2 subpial, enhancing nodules in a patient with von Hippel-Lindau disease. One nodule is small and present in the cistern magna; the other is in the cervical spine.
T1-weighted postgadolinium MRI shows 2 subpial, enhancing nodules in a patient with von Hippel-Lindau disease. One nodule is small and present in the cistern magna; the other is in the cervical spine.
Generally, the cyst wall does not enhance, but occasionally, it can appear as a paper-thin line of enhancement that represents a combination of compressed cerebellar tissue and gliosis. [34] Occasionally, the edge of the tentorium can be misinterpreted as an enhancing rim, with differentiation made by using coronal sections.
CT shows all the clinically significant features of hemangioblastoma, along with secondary features such as hydrocephalus and edema. False-negative results are found in patients with small nodules (< 5 mm) that can be obscured by posterior fossa artifacts; therefore, CT is not a sensitive screening procedure. False-positive results are rare. Metastases and cystic astrocytoma can appear similar. A diagnostic pitfall is the hemangioblastoma with a small central lucency, which can be interpreted as a necrotic metastasis. In this case, the ringlike enhancement of the necrotic nodule is thick and irregular. [30]
Magnetic Resonance Imaging
MRI with gadolinium enhancement is the best study for screening hemangioblastomas, with the highest sensitivity and specificity compared with CT and nonenhanced MRI. Large studies are necessary to achieve a high degree of confidence; however, the advantages are obvious. [22, 28, 29, 35]
Intracranial hemangioblastomas can manifest as 3 morphologic patterns based on the macroscopic pathology. These are well correlated with the MRI findings and include the following [36, 23, 37] :
-
Cyst with a small mural nodule
-
Solid mass with a central cystic component
-
Solid tumor without a cystic component
A cyst with a small mural nodule is the most common presentation. Cystic fluid surrounding the nodule is hyperintense on T1-weighted images and hyperintense on T2-weighted images. Characteristics of the fluid vary slightly related to protein content. The mural nodule is isointense on T1-weighted images and demonstrates high signal on T2-weighted images. After the administration of gadolinium-based contrast medium, the nodule shows prominent enhancement and the cyst does not enhance (see the image below). [36]
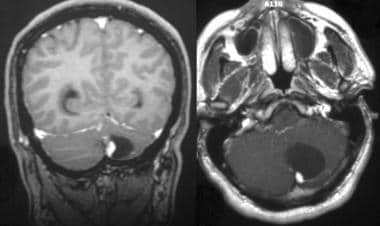 Coronal and axial T1-weighted gadolinium-enhanced MRIs show a large cyst with a peripheral intense enhancing mural nodule.
Coronal and axial T1-weighted gadolinium-enhanced MRIs show a large cyst with a peripheral intense enhancing mural nodule.
Solid masses with a central cyst behave similarly; therefore, the different morphologic patterns have been postulated to be part of the natural history of a solid tumor that develops a cystic component around or within it (see the images below). [38, 39]
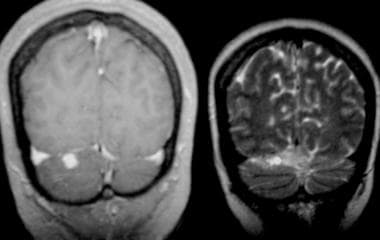 Patient with von Hippel-Lindau disease. T1-weighted gadolinium-enhanced MRI shows an enhancing nodule. Coronal T2-weighted MRI shows a small high-signal-intensity cyst.
Patient with von Hippel-Lindau disease. T1-weighted gadolinium-enhanced MRI shows an enhancing nodule. Coronal T2-weighted MRI shows a small high-signal-intensity cyst.
 Patient with von Hippel-Lindau disease (same patient as in previous image at 1-year follow-up). Coronal T1-weighted gadolinium-enhanced MRI shows an enhancing nodule that has grown in size adjacent to a low-signal-intensity cyst. T2-weighted MRI shows a cystic area that has increased in size, with high-signal-intensity characteristics.
Patient with von Hippel-Lindau disease (same patient as in previous image at 1-year follow-up). Coronal T1-weighted gadolinium-enhanced MRI shows an enhancing nodule that has grown in size adjacent to a low-signal-intensity cyst. T2-weighted MRI shows a cystic area that has increased in size, with high-signal-intensity characteristics.
Solid hemangioblastomas occur less frequently than the other patterns (see the image below). The lesion is isointense or hypointense on T1-weighted images and hyperintense on T2-weighted images. Transition from a solid tumor to a classic cystic tumor with a small mural nodule has been reported. Occasionally, signal in solid tumor components can be heterogeneous on T1-weighted images, with areas of increased signal within the solid portion. These regions may represent lipid in the stromal cells or methemoglobin from hemorrhage. [26]
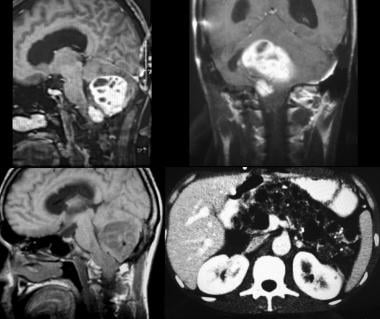 Sagittal (top left) and coronal (top right) T1-weighted gadolinium-enhanced MRI images in a patient with von Hippel-Lindau disease presenting with 2 infratentorial hemangioblastomas. The larger tumor shows with cystic central areas. Bottom left, T1-weighted MRI shows that both lesions have low signal intensity. Bottom right, Abdominal axial image of the same patient shows multiple cysts in the pancreas.
Sagittal (top left) and coronal (top right) T1-weighted gadolinium-enhanced MRI images in a patient with von Hippel-Lindau disease presenting with 2 infratentorial hemangioblastomas. The larger tumor shows with cystic central areas. Bottom left, T1-weighted MRI shows that both lesions have low signal intensity. Bottom right, Abdominal axial image of the same patient shows multiple cysts in the pancreas.
Commonly (60-69% of the time), hemangioblastomas have associated internal or peripheral serpentine signal voids, which represent dilated afferent and efferent vessels. [40] Therefore, the presence of a peripheral cyst with a mural nodule surrounded by signal voids is characteristic of hemangioblastoma. [23] Pathologic dilated vessels can be demonstrated as hyperintense structures on flow-enhanced gadolinium studies. MRI with intravenous contrast enhancement shows enhancing nodules well because of their vascularity (see the image below). [36]
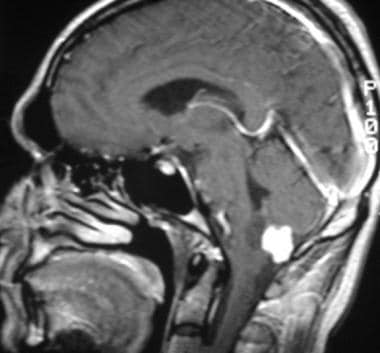 Sagittal T1-weighted gadolinium-enhanced MRI shows a homogeneous intense enhancing tumor in the cistern magna.
Sagittal T1-weighted gadolinium-enhanced MRI shows a homogeneous intense enhancing tumor in the cistern magna.
False-negative results can be seen with small lesions (< 5 mm) and with delayed imaging because of the early enhancement of the lesions. False-positive findings are rare, and most false-positive findings lead to an inadequate diagnosis. For solid and multiple enhancing lesions, metastases are the most important differential diagnosis; supratentorial lesions are more common in metastases. The visualization of associated abnormal vessels helps in differentiating hemangioblastomas from other cystic lesions. [41]
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). NSF/NFD has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Ultrasonography
Gray-scale ultrasonography has been useful in the intraoperative evaluation of cerebellar and spinal hemangioblastomas by shortening and simplifying the surgical procedure. Most hemangioblastomas appear hyperechoic to adjacent neural tissue. Most studied cases have involved spinal hemangioblastomas. The use of ultrasonography is limited in brain lesions.
Doppler color flow images can be helpful in patients with isoechoic lesions, showing increase of vascularity as a tightly packed tangle of vessels. The technique can also demonstrate areas without flow that correspond to cystic areas. [42, 43]
Angiography
For many years, angiography was the primary diagnostic modality and still is a preoperative requisite in many patients. Infratentorial hemangioblastomas are evaluated by using vertebral angiography, which provides a selective opacification of both vertebral arteries by arterial femoral catheterization. Subtraction and magnification are necessary. [27]
Angiography is superior to CT in defining the vascular nodule and in characterizing occult and multiple lesions. The relationship of the nodule with the cyst is not demonstrated as well on angiograms as on MRI or CT scans. [27]
Angiography provides detection, exact localization, and definition of the vascularity of tumors in the vertebrobasilar system. Findings are specific, and the diagnosis can be made with confidence. Nodules usually stain intensely with either a homogeneous or mottled appearance (see the images below). The tumor has irregular vessels. The largest tumors are associated with 1 or more enlarged feeding arteries and draining veins and can demonstrate arteriovenous shunting. When a cyst is present, it can be seen as an avascular area producing vascular displacement. [27, 38]
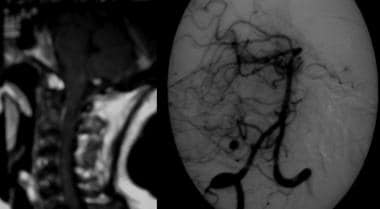 Left, T1-weighted gadolinium-enhanced MRI with an enhancing nodule subpial in the cistern magna. Right, Angiogram obtained with a selective injection of the right vertebral artery shows an intense tumor stain in the arterial phase, without arteriovenous shunting.
Left, T1-weighted gadolinium-enhanced MRI with an enhancing nodule subpial in the cistern magna. Right, Angiogram obtained with a selective injection of the right vertebral artery shows an intense tumor stain in the arterial phase, without arteriovenous shunting.
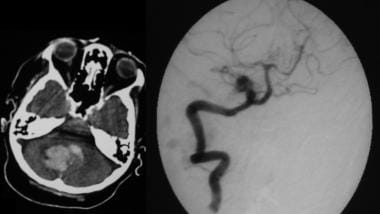 On the left, a nonenhanced CT scan demonstrates acute bleeding in the posterior fossa. On the right, a selective angiogram of the vertebral artery shows an intense tumor stain.
On the left, a nonenhanced CT scan demonstrates acute bleeding in the posterior fossa. On the right, a selective angiogram of the vertebral artery shows an intense tumor stain.
Imaging of the neck with injection of each vertebral artery should be routine in patients with von Hippel-Landau (VHL) complex or a posterior fossa hemangioblastoma. The blood supply is usually received through the pia mater; however, external carotid angiography provides valuable preoperative information in selected patients in whom a hemangioblastoma is superficial and abuts the dura (which is usually supplied by meningeal branches of the carotid system).
-
Major clinical manifestations of von Hippel-Lindau disease.
-
Flow diagram illustrates the role of the von Hippel-Lindau protein in angiogenesis (modified from Richard, 2000).
-
Photomicrograph shows the classic microscopic appearance of a cerebellar hemangioblastoma with numerous capillaries and polygonal stroma cells shows vacuoles of cytoplasm and hyperchromatic nucleus (hematoxylin-eosin stain, high-power magnification). Courtesy of Dr Paul Fiedler.
-
Photomicrograph of a hemangioblastoma shows numerous vascular capillary networks with endothelial linings and stromal cells (hematoxylin-eosin stain, low-power magnification). Courtesy of Dr Paul Fiedler.
-
Diagram illustrates the cystic forms.
-
Patient with von Hippel-Lindau disease. T1-weighted gadolinium-enhanced MRI shows an enhancing nodule. Coronal T2-weighted MRI shows a small high-signal-intensity cyst.
-
Patient with von Hippel-Lindau disease (same patient as in previous image at 1-year follow-up). Coronal T1-weighted gadolinium-enhanced MRI shows an enhancing nodule that has grown in size adjacent to a low-signal-intensity cyst. T2-weighted MRI shows a cystic area that has increased in size, with high-signal-intensity characteristics.
-
Coronal and axial T1-weighted gadolinium-enhanced MRIs show a large cyst with a peripheral intense enhancing mural nodule.
-
Left, T1-weighted gadolinium-enhanced MRI with an enhancing nodule subpial in the cistern magna. Right, Angiogram obtained with a selective injection of the right vertebral artery shows an intense tumor stain in the arterial phase, without arteriovenous shunting.
-
On the left, a nonenhanced CT scan demonstrates acute bleeding in the posterior fossa. On the right, a selective angiogram of the vertebral artery shows an intense tumor stain.
-
Sagittal T1-weighted gadolinium-enhanced MRI shows a homogeneous intense enhancing tumor in the cistern magna.
-
T1-weighted postgadolinium MRI shows 2 subpial, enhancing nodules in a patient with von Hippel-Lindau disease. One nodule is small and present in the cistern magna; the other is in the cervical spine.
-
Sagittal (top left) and coronal (top right) T1-weighted gadolinium-enhanced MRI images in a patient with von Hippel-Lindau disease presenting with 2 infratentorial hemangioblastomas. The larger tumor shows with cystic central areas. Bottom left, T1-weighted MRI shows that both lesions have low signal intensity. Bottom right, Abdominal axial image of the same patient shows multiple cysts in the pancreas.
-
Supratentorial hemangioblastoma proved by histologic analysis. Carotid arteriogram demonstrates a vascular, dense, tumor filled from the anterior cerebral vessels and not involving the sagittal sinus.