Practice Essentials
Ganglioglioma was first described by Courville in 1930 as a central nervous system neoplasm containing both astrocytic and neuronal components. [1] Gangliogliomas may occur anywhere in the central nervous system but are not encountered commonly. Although most lesions are benign, significant clinical symptoms may occur. [2, 3] Hydrocephalus can result from increased intracranial pressure. [3] Epileptic seizures are associated with supratentorial gangliogliomas. Focal neurologic symptoms such as headache, nausea and vomiting are more common indications of infratentorial located tumors. [2]
Typically, gangliogliomas are grade I tumors that localize in the cerebral hemisphere but may involve deep structures such as the basal ganglia. They are usually well-differentiated, slow-growing tumors, and complete resection is curative in most cases. [4, 5]
As with many other brain tumors, imaging techniques define the location of gangliogliomas and their relationship to adjacent structures. Because of the relative rarity and nonspecific appearance of these lesions, gangliogliomas are only infrequently considered a presurgical diagnosis. [6, 7, 8, 9, 10, 11, 12]
Magnetic resonance imaging (MRI) with contrast enhancement is more sensitive and specific than other imaging techniques in determining the presence and location of gangliogliomas and in characterizing the lesions' cystic and/or solid components. [13] However, the imaging appearances of these tumors are nonspecific, and the diagnosis is usually established by histology and immunohistochemistry. [14, 15]
(See the image below.)
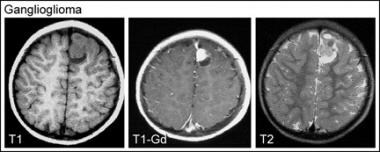 Axial magnetic resonance images (T1-weighted, T1-weighted with contrast, and T2-weighted) demonstrate a left superior medial frontal mixed solid and cystic mass that is surgically proven and typical ganglioglioma. The solid anterior component is hypointense on the T1-weighted image, of intermediate intensity on the T2-weighted image, and reveals dense contrast enhancement. The cystic posterior component has low cerebrospinal fluidlike signal on the T1-weighted image and bright signal on the T2-weighted image with no contrast enhancement. Note that the tumor extends to a cortical surface, and no surrounding edema is seen.
Axial magnetic resonance images (T1-weighted, T1-weighted with contrast, and T2-weighted) demonstrate a left superior medial frontal mixed solid and cystic mass that is surgically proven and typical ganglioglioma. The solid anterior component is hypointense on the T1-weighted image, of intermediate intensity on the T2-weighted image, and reveals dense contrast enhancement. The cystic posterior component has low cerebrospinal fluidlike signal on the T1-weighted image and bright signal on the T2-weighted image with no contrast enhancement. Note that the tumor extends to a cortical surface, and no surrounding edema is seen.
Usually, plain films do not contribute to the diagnosis of gangliogliomas. Rarely, findings may be related to increased intracranial pressure. Occasionally, gangliogliomas are sufficiently calcified to be visible on plain radiographs.
Nuclear medicine studies are not helpful in the diagnosis of gangliogliomas. Solid tumors may show increased radiotracer uptake on single-photon emission CT studies. In a small cohort, fluorodeoxyglucose positron emission tomography (FDG-PET) scanning and thallium-201 (201Tl) single-photon emission CT (SPECT) scanning reportedly have helped in preoperative grading of these tumors [16] ; however, this observation has not been substantiated. Only limited information is available in the literature regarding FDG-PET scan findings in these tumors. Grade I/II gangliogliomas showed hypometabolic or isometabolic changes.
Cerebral angiography provides no additional information apart from confirming the nonvascular nature of the tumors. Rarely, the enhancement pattern of the ganglioglioma may mimic a vascular malformation, and catheter angiography is required to exclude a vascular malformation.
Computed Tomography
On CT scans, most of the tumors are hypodense or isodense to brain parenchyma with poor contrast enhancement. The gangliogliomas are usually well circumscribed and located peripherally. However, the imaging appearance is nonspecific. Grossly, one half of the tumors show cystic areas, calcification, and enhancement. Punctate or flecklike calcification is seen in one third of tumors. Surrounding edema is unusual, although a correlation between surrounding edema and anaplasia has been described, and hemorrhage is rarely identified.
Cystic tumors are predominantly found (with decreasing frequency) in the cerebellum, temporal, frontal, and parietal lobes and have a variable appearance from a single large cyst to a cyst with mural nodule to a multicystic mass. Solid tumors usually are seen in the temporal lobe and have more contrast enhancement. Anaplastic tumors have a heterogeneous appearance with excellent contrast enhancement.
Solid enhancing tumors in the temporal lobe in younger patients with seizures may suggest the diagnosis. In addition, ganglioglioma is the most common neoplastic cause of temporal lobe seizures.
Low-grade gliomas may appear similar; calcified lesions may mimic oligodendrogliomas, and cystic tumors may mimic juvenile pilocytic astrocytoma.
Magnetic Resonance Imaging
MRI is useful in differentiating the cystic and solid components of tumors (see the images below). Most tumors are hypointense on T1-weighted images and hyperintense on T2-weighted images relative to gray matter. An isolated case report demonstrated leptomeningeal spread of the tumor. [17, 18, 14]
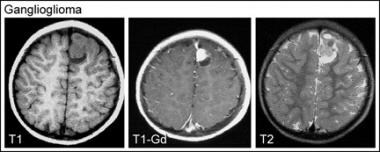 Axial magnetic resonance images (T1-weighted, T1-weighted with contrast, and T2-weighted) demonstrate a left superior medial frontal mixed solid and cystic mass that is surgically proven and typical ganglioglioma. The solid anterior component is hypointense on the T1-weighted image, of intermediate intensity on the T2-weighted image, and reveals dense contrast enhancement. The cystic posterior component has low cerebrospinal fluidlike signal on the T1-weighted image and bright signal on the T2-weighted image with no contrast enhancement. Note that the tumor extends to a cortical surface, and no surrounding edema is seen.
Axial magnetic resonance images (T1-weighted, T1-weighted with contrast, and T2-weighted) demonstrate a left superior medial frontal mixed solid and cystic mass that is surgically proven and typical ganglioglioma. The solid anterior component is hypointense on the T1-weighted image, of intermediate intensity on the T2-weighted image, and reveals dense contrast enhancement. The cystic posterior component has low cerebrospinal fluidlike signal on the T1-weighted image and bright signal on the T2-weighted image with no contrast enhancement. Note that the tumor extends to a cortical surface, and no surrounding edema is seen.
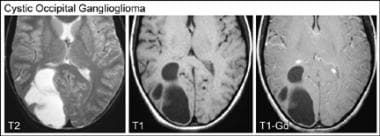 Axial magnetic resonance images (T2-weighted, T1-weighted, and T1-weighted with contrast) show a multiloculated, predominantly cystic right occipital mass that is surgically proven and a typical ganglioglioma. The loculi are isointense to cerebrospinal fluid on both T1-weighted and T2-weighted images. Neither contrast enhancement nor surrounding edema is seen.
Axial magnetic resonance images (T2-weighted, T1-weighted, and T1-weighted with contrast) show a multiloculated, predominantly cystic right occipital mass that is surgically proven and a typical ganglioglioma. The loculi are isointense to cerebrospinal fluid on both T1-weighted and T2-weighted images. Neither contrast enhancement nor surrounding edema is seen.
A proton magnetic resonance spectroscopy signal from N-acetylaspartate is an endogenous marker for functioning neurons. The choline-to-creatine ratio is lower and the N-acetylaspartate-to-creatine ratio is higher in gangliogliomas than in gliomas. A high N-acetylaspartate-to-creatine ratio may be due to a neoplastic neuronal component.
In a study of 10 patients aged 14-67 years with histologically proven supratentorial gangliogliomas, minimum apparent diffusion coefficient (minADC) values of gangliogliomas (1.45 +/- 0.20 × 10-3 mm2/s) was found to be significantly higher than the minADC values of astrocytomas. [19] Kikuchi et al determined that minADC values accurately reflect the low tumor cellularity of gangliogliomas and may therefore be helpful in the differential diagnosis of the tumors. [19]
As with CT scanning, the imaging patterns are nonspecific. Temporal lobe gangliogliomas usually present with temporal lobe seizures: a solid enhancing tumor located in the temporal lobe with no surrounding edema in a younger patient with intractable seizures is highly suggestive of the diagnosis. With the advent of more routine magnetic resonance screening of seizure patients, these tumors are increasingly identified on imaging.
Low-grade gliomas may appear similar; calcified lesions may mimic oligodendrogliomas, and cystic tumors may mimic juvenile pilocytic astrocytoma.
-
Axial magnetic resonance images (T1-weighted, T1-weighted with contrast, and T2-weighted) demonstrate a left superior medial frontal mixed solid and cystic mass that is surgically proven and typical ganglioglioma. The solid anterior component is hypointense on the T1-weighted image, of intermediate intensity on the T2-weighted image, and reveals dense contrast enhancement. The cystic posterior component has low cerebrospinal fluidlike signal on the T1-weighted image and bright signal on the T2-weighted image with no contrast enhancement. Note that the tumor extends to a cortical surface, and no surrounding edema is seen.
-
Axial magnetic resonance images (T2-weighted, T1-weighted, and T1-weighted with contrast) show a multiloculated, predominantly cystic right occipital mass that is surgically proven and a typical ganglioglioma. The loculi are isointense to cerebrospinal fluid on both T1-weighted and T2-weighted images. Neither contrast enhancement nor surrounding edema is seen.










