Practice Essentials
Gallbladder carcinoma (GBC) is the most common and aggressive biliary tract malignancy, with high postoperative recurrence rates. [1, 2] GBC may present as mass lesions replacing the gallbladder, focal or diffuse thickening of the gallbladder wall, and intraluminal masses in the gallbladder. Various benign conditions can mimic GBC. [3] Wall thickening does not always indicate malignancy and can be secondary to inflammatory or benign gallbladder disease and extracholecystic causes and systemic pathologies. About 20-30% of patients with GBC have gallbladder thickening. Gallbladder wall thickness greater than 3 mm is considered pathologic. GBC can present as both focal and diffuse thickening, with the focal pattern being more common. Overall 5-year survival rate in patients with in situ disease is 80%, but it declines to 8% in patients with lymph node involvement and 2% in patients with stage 4b disease. [4, 5, 6, 7, 8]
GBC predominantly affects older persons with long-standing cholecystolithiasis. GB epithelial tumors tend to behave similarly to other GI adenocarcinomas. When the diagnosis is made incidentally at the time of cholecystectomy, surgical resection can be curative [9, 10, 11] ; however, more commonly, the tumor is unresectable and is rarely diagnosed preoperatively despite patients' symptoms. Early diagnosis can improve the clinical outcome and the cure rate of GBC.
According to an extensive literature study by Cocco et al, melanoma accounts for about 55.6% of cases of gallbladder metastases. The remaining cases of metastatic spread originate from breast cancer (13.6%), hepatocellular carcinoma (13.6%), renal cell carcinoma (6.8%), lung cancer (4.5%), lymphoma (3.5%), and gastric cancer (2.4%). [12]
The only curative approach to GBC is surgery; however, more than 50% of cases are unresectable at the time of diagnosis. Together with surgery and chemotherapy, endoscopy represents an available palliative option for patients with advanced GBC not eligible for curative treatment. Cholangitis, jaundice, gastric outlet obstruction, and pain are common complications of advanced GBC for which endoscopic management can improve overall survival and patient quality of life. [2]
Ultrasonography (US), which is readily available, noninvasive, and cost-effective, is the imaging modality of choice for GBC. [13, 14, 15, 16] However, US cannot be used to stage the tumor. Visualization of lymph nodes, intraperitoneal disease, and distant metastases is difficult.
Computed tomography (CT) scans can detect GB masses and thickening of the GB wall.
Plain abdominal radiographic films have a limited role in GBC. These images may reveal porcelain GB, calcified gallstones, and, rarely, biliary gas from a GB-enteric fistula. Mucinous tumors may produce vague or punctate calcification in the primary tumor or in metastatic foci that may be visible on plain films. Barium studies, if positive, show duodenal invasion and displacement. Transverse colon invasion occasionally may be seen.
Magnetic resonance imaging (MRI) is not used commonly in the diagnostic process for GBC. Findings are analogous to those derived from CT scanning. The tumor usually is bright on T2-weighted images and is poorly marginated. On T1-weighted images, relative to the liver, GBC ranges from isointense to hypointense. [13] Magnetic resonance imaging with the use of gadolinium and diffusion-weighted sequence is the preferred modality for GB wall characterization. [17]
Nonopacification of the GB on cholescintigraphy with technetium-99m (99mTc) iminodiacetic acid analogue scanning is a nonspecific sign that indicates the possibility of carcinoma. This modality is not used commonly and has generally been replaced by US.
Fluoro-2-deoxy-D-glucose (FDG) positron emission tomography (PET)–CT has been used to determine optimal management of biliary tumors. [18]
Angiography may reveal the neovascularity that arises from the cystic arteries, as well as arterial and venous encasement in the area of the GB, although this modality is not used as a diagnostic tool.
(See the images of gallbladder carcinoma below.)
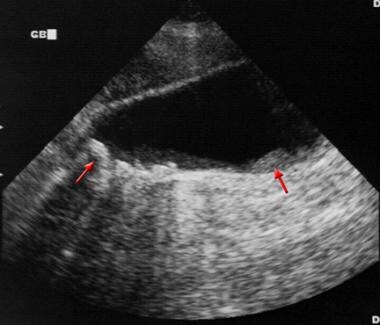 Sagittal sonogram in a 71-year-old woman. This image demonstrates heterogeneous thickening of the gallbladder wall (arrows). The diagnosis was primary papillary adenocarcinoma of the gallbladder.
Sagittal sonogram in a 71-year-old woman. This image demonstrates heterogeneous thickening of the gallbladder wall (arrows). The diagnosis was primary papillary adenocarcinoma of the gallbladder.
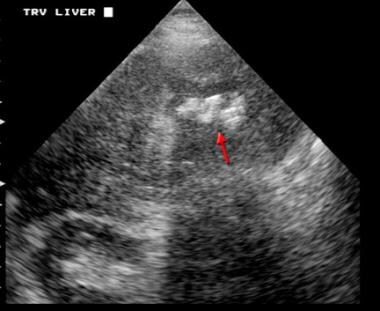
 Computed tomography scan in a 65-year-old man. This image depicts squamous cell carcinoma of the gallbladder and invasion of the liver.
Computed tomography scan in a 65-year-old man. This image depicts squamous cell carcinoma of the gallbladder and invasion of the liver.
Computed Tomography
Computed tomography (CT) scanning can detect GB masses and thickening of the GB wall, as well as the extent of hepatic invasion (see the images below). [19, 20] Peritoneal or distant disease, although uncommon, may be seen.
 Computed tomography scan in a 65-year-old man. This image depicts squamous cell carcinoma of the gallbladder and invasion of the liver.
Computed tomography scan in a 65-year-old man. This image depicts squamous cell carcinoma of the gallbladder and invasion of the liver.
 Computed tomography (CT) scan in a 65-year-old man with squamous cell carcinoma of the gallbladder and invasion of the liver (same patient as in the previous image). This CT scan depicts a lower cut through the liver than does the previous image.
Computed tomography (CT) scan in a 65-year-old man with squamous cell carcinoma of the gallbladder and invasion of the liver (same patient as in the previous image). This CT scan depicts a lower cut through the liver than does the previous image.
Three patterns of findings are identified on CT scans. In 50% of patients, a heterogeneous mass that replaces the GB is present. The term "jam-packed GB" refers to filling of the entire GB lumen by tumor.
Focal or diffuse wall thickening is seen on CT scans in approximately 25% of patients, but this finding often is better appreciated on US. The thickened GB wall may show abnormally bright or persistent enhancement on infused CT scans.
In the remaining 20-25% of patients, a discrete intraluminal mass that enhances heterogeneously is visualized after administration of intravenous contrast. Trapped stones within the mass occasionally may be seen. CT scans may also show biliary dilatation and metastases.
On multivariate analysis, high carbohydrate antigen 19-9, low muscle attenuation, high visceral fat attenuation, liver invasion, and other organ invasion on preoperative CT have been identified as independent risk factors for early recurrence of GBC. [21] Xanthogranulomatous cholecystitis is an inflammatory process that cannot be reliably distinguished from GBC on CT scans because of multiple, overlapping features such as GB wall thickening and involvement of surrounding tissues, including portal lymph node, fat, and liver tissue.
In a retrospective analysis by Han and Han of clinical data from patients with thick-wall GBC or chronic cholecystitis who underwent multislice spiral CT (MSCT), findings of disruption of the gallbladder mucosa line, blurred gallbladder outline, high obstruction of the biliary tract, lymphomegaly, adjacent invasion, peritoneal effusion, wall nodules, and gallbladder wall thickness were greater in patients with thick-wall GBC than in patients with chronic cholecystitis. The sensitivity and specificity of MSCT in diagnosing thick-wall GBC were 86.11% and 95%, respectively. [17]
Ultrasonography
Ultrasound (US) is the most commonly used imaging modality for evaluating GBC; however, no pathognomonic findings have been identified. [22] Indirect signs that suggest the presence of GBC include the following:
-
GB wall thickening
-
Single or multiple intraluminal masses
-
Extraluminal mass that extends to the liver
-
Polyps >1 cm in diameter
Transabdominal US is the first-line investigation for evaluation of GB wall thickening. However, further characterization requires additional imaging tests. [23]
The thickening associated with early lesions is rarely detected. More advanced lesions may produce marked mural thickening with irregular and mixed echogenicity, as shown in the first image below; this is the second most common manifestation of GBC, accounting for 20-30% of patients. The GB may be small, normal, or distended, and gallstones are often present (see the second image below). GB wall thickening is nonspecific and may be seen in multiple medical conditions, including acute and chronic cholecystitis, heart failure, hypoalbuminemia, hepatitis, and cirrhosis. However, GB wall thickening in these patients is usually diffuse in contrast to focal thickening in patients who have GBC.
 Sagittal sonogram in a 71-year-old woman. This image demonstrates heterogeneous thickening of the gallbladder wall (arrows). The diagnosis was primary papillary adenocarcinoma of the gallbladder.
Sagittal sonogram in a 71-year-old woman. This image demonstrates heterogeneous thickening of the gallbladder wall (arrows). The diagnosis was primary papillary adenocarcinoma of the gallbladder.
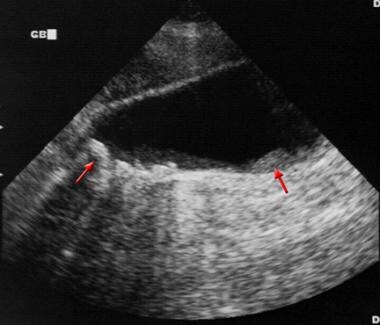
 Transverse ultrasonogram in a 66-year-old man. This image shows the gallbladder is filled with shadowing stones (arrow) that are surrounded by the hypoechoic liver parenchyma, which represents direct invasion by carcinoma. The diagnosis was squamous cell carcinoma of the gallbladder.
Transverse ultrasonogram in a 66-year-old man. This image shows the gallbladder is filled with shadowing stones (arrow) that are surrounded by the hypoechoic liver parenchyma, which represents direct invasion by carcinoma. The diagnosis was squamous cell carcinoma of the gallbladder.
The polyps or masses are of homogeneous echotexture without evidence of shadowing. Polyps are usually sessile and only rarely have a stalk; this is the least common manifestation of GBC, seen in 15-25% of cases. Visualization of a polyp that is smaller than 1 cm in the appropriate age group should arouse suspicion for adenoma/adenocarcinoma because only these incidental early lesions have a good prognosis. Gallstones may also be present and may prevent recognition of a small polypoid mass. Tumefactive sludge can mimic a mass.
An extraluminal mass is often accompanied by a large mass that replaces the GB fossa. This mass is often complex, with visible areas of necrosis; this is the most common manifestation of GBC, seen in 40-65% of cases of GBC (see the second image above). According to studies, polyps with a diameter greater than 1 cm are malignant in 23-88% of cases. [24]
A mass that arises from the GB may be difficult to differentiate from a mass that arises from the liver. Visualization of gallstones located centrally in a solid mass can facilitate diagnosis. Adenomyomatosis can also cause focal GB wall thickening. This benign condition may mimic a GB tumor. [25] US may show focal or diffuse wall thickening, with echogenic foci in Rokitansky-Aschoff sinuses that often are seen as "comet-tail" reverberation artifacts.
Benign polypoid lesions are difficult to distinguish from polypoid carcinoma; the cauliflower-like appearance suggests malignancy. [26] Polyps smaller than 5 mm are unlikely to be malignant; polypoid lesions that measure 5-10 mm should be followed up. In a patient with melanoma, metastases can cause multiple polypoid lesions. Tumefactive sludge can also mimic an intraluminal mass; usually, this is easy to differentiate by demonstrating the mobility of the sludge. Color Doppler US can be used; evidence of flow within the lesion indicates that this is a solid mass rather than sludge.
High-resolution ultrasound (HRUS) has been shown to enable accurate T categorization of GBC and to provide high-resolution images of gallbladder polyps. [16] HRUS may also have a role in stratifying the risk for malignancy. [27] One study found that contrast-enhanced harmonic endoscopic ultrasound (CH-EUS) may improve preoperative diagnostic accuracy and interobserver agreement in the differential diagnosis of gallbladder wall thickening. [28]
Questions & Answers
Overview
What is carcinoma of the gallbladder?
What is the role of ultrasonography in the workup of carcinoma of the gallbladder?
What is the role of CT scans in the workup of carcinoma of the gallbladder?
What is the role of abdominal radiography in the workup of carcinoma of the gallbladder?
What is the role of MRI in the workup of carcinoma of the gallbladder?
What is the role of cholescintigraphy in the workup of carcinoma of the gallbladder?
What is the role of FDG PET-CT in the workup of carcinoma of the gallbladder?
What is the role of angiography in the workup of carcinoma of the gallbladder?
Which findings on CT scans are characteristic of carcinoma of the gallbladder?
Which findings on ultrasonography are characteristic of carcinoma of the gallbladder?
-
Sagittal sonogram in a 71-year-old woman. This image demonstrates heterogeneous thickening of the gallbladder wall (arrows). The diagnosis was primary papillary adenocarcinoma of the gallbladder.
-
Transverse ultrasonogram in a 66-year-old man. This image shows the gallbladder is filled with shadowing stones (arrow) that are surrounded by the hypoechoic liver parenchyma, which represents direct invasion by carcinoma. The diagnosis was squamous cell carcinoma of the gallbladder.
-
Computed tomography scan in a 65-year-old man. This image depicts squamous cell carcinoma of the gallbladder and invasion of the liver.
-
Computed tomography (CT) scan in a 65-year-old man with squamous cell carcinoma of the gallbladder and invasion of the liver (same patient as in the previous image). This CT scan depicts a lower cut through the liver than does the previous image.








