Practice Essentials
Duodenal atresia is a congenital intestinal obstruction in the form of complete obliteration of the duodenal lumen (see the images below). A duodenal diaphragm (or duodenal web) is thought to represent a mild form of atresia. Duodenal stenosis (incomplete obstruction of the duodenal lumen) is discussed with duodenal atresia because the 2 disorders together represent a spectrum of similar intrauterine events. Duodenal atresia can cause bilious or nonbilious vomiting within the first 24 to 38 hours after birth, typically following the first oral feeding. The diagnosis can be made by antenatal ultrasound. If duodenal atresia is not diagnosed antenatally, the diagnosis can be made bt plain abdominal radiograph. The incidence of duodenal atresia is 1 per 6000 births in the United States. Intrinsic congenital duodenal obstruction constitutes two thirds of all congenital duodenal obstructions (duodenal atresia, 40-60%; duodenal web, 35-45%; annular pancreas, 10-30%; duodenal stenosis, 7-20%). [1, 2]
 Types of duodenal recanalization anomalies. Dilatation of the proximal normal segment is seen in each type. A. Diaphragm. B. Solid cord and atresia. C. Segmental absence.
Types of duodenal recanalization anomalies. Dilatation of the proximal normal segment is seen in each type. A. Diaphragm. B. Solid cord and atresia. C. Segmental absence.
 Anteroposterior radiograph of the abdomen depicts the double-bubble sign of duodenal atresia. Note the flattened acetabular angles and broadened ilia of a patient with trisomy 21.
Anteroposterior radiograph of the abdomen depicts the double-bubble sign of duodenal atresia. Note the flattened acetabular angles and broadened ilia of a patient with trisomy 21.
One half of the neonates with duodenal atresia or stenosis are born prematurely, and hydramnios occurs in approximately 40% of neonates with duodenal obstruction. In addition, duodenal atresia or duodenal stenosis is most commonly associated with trisomy 21 (see the following image), with about 22-30% of patients with duodenal obstruction having trisomy 21. [3]
 Anteroposterior radiograph of the abdomen depicts the double-bubble sign of duodenal atresia. Note the flattened acetabular angles and broadened ilia of a patient with trisomy 21.
Anteroposterior radiograph of the abdomen depicts the double-bubble sign of duodenal atresia. Note the flattened acetabular angles and broadened ilia of a patient with trisomy 21.
Anatomy
In most cases, duodenal atresia occurs below the ampulla of Vater. In a very few cases, the atresia occurs proximal to the ampulla. Annular pancreas occurs when pancreatic tissue surrounds the second portion of the duodenum. [4] If the encirclement is complete, it may be associated with complete or incomplete duodenal obstruction. Because duodenal atresia or duodenal stenosis occurs in all cases of annular pancreas, the anomalous pancreas should be considered a secondary change rather than a primary cause of duodenal obstruction.
Preferred examination
Plain radiographs that demonstrate a double-bubble appearance with no distal gas are characteristic of duodenal atresia (see the images below). Distal bowel gas indicates stenosis, incomplete membrane, or a hepatopancreatic ductal anomaly. Occasionally, a radiograph must be obtained with the patient in the erect or the decubitus position to delineate the duodenal component. If a combination of esophageal atresia and duodenal atresia is present, ultrasonography is preferred. [5]
 Anteroposterior radiograph of the abdomen depicts the double-bubble sign of duodenal atresia. Note the flattened acetabular angles and broadened ilia of a patient with trisomy 21.
Anteroposterior radiograph of the abdomen depicts the double-bubble sign of duodenal atresia. Note the flattened acetabular angles and broadened ilia of a patient with trisomy 21.
 Anteroposterior projection of the chest and abdomen demonstrates the double-bubble sign of duodenal atresia in the abdomen, as well as a proximal dilated pouch (right arrow) resulting from esophageal atresia; this displaces the trachea (left arrow) toward the right side in the superior mediastinum. The presence of air in the stomach and duodenum is related to the existence of a distal fistula.
Anteroposterior projection of the chest and abdomen demonstrates the double-bubble sign of duodenal atresia in the abdomen, as well as a proximal dilated pouch (right arrow) resulting from esophageal atresia; this displaces the trachea (left arrow) toward the right side in the superior mediastinum. The presence of air in the stomach and duodenum is related to the existence of a distal fistula.
No oral contrast materials are necessary in the evaluation of complete duodenal obstruction. Occasionally, a small amount of positive contrast material can be instilled through a feeding tube into the distal stomach and duodenum to differentiate the diaphragm from a long stenosis.
Occasionally, barium enema examination is suggested as an adjunct study in the evaluation of duodenal atresia (see the image below). Barium enema findings can demonstrate a malpositioned cecum, but this is not always diagnostic of malrotation and volvulus. [6] In addition, if a microcolon is demonstrated, the presence of additional, more distal atresias can be suggested. Succus entericus may be prevented from reaching the colon because of the additional area of bowel obstruction. Multiple atresias are present in approximately 15% of patients. However, most surgeons can determine the presence of malrotation and additional atresias at the time of surgery. [7]
 Barium air contrast–enhanced study of the duodenal membrane (arrows) in the lateral projection shows a small amount of barium exiting into the more distal bowel. Coincidentally, 2 coronal cleft vertebrae are noted.
Barium air contrast–enhanced study of the duodenal membrane (arrows) in the lateral projection shows a small amount of barium exiting into the more distal bowel. Coincidentally, 2 coronal cleft vertebrae are noted.
Ultrasonography
On ultrasonography, a finding of 2 echo-free fluid collections in the upper abdomen suggests duodenal atresia in association with esophageal atresia. Esophageal atresia without a fistula does not permit air to reach the stomach and duodenum. [8] These findings do not require confirmation with additional procedures.
MRI
Cronin et al retrospectively assessed the role of a magnetic resonance small-bowel follow-through (MR SBFT) for small-bowel pathology in 17 children and found that MR SBFT allows pseudodynamic functional imaging and identifies extraluminal disease without biologic risk. [9] MR SBFT advantages included high tolerability (84.2%), lack of ionizing radiation, avoidance of duodenojejunal intubation, and excellent achievement of luminal distention. Pathologic lesions were identified in 53% of cases. In addition, there was high interobserver agreement regarding mean distention scores; the MR table time was short, without any early termination; there were few visits to the MR table; and the mean duration for complete small-bowel evaluation was 25 minutes.
Differential diagnosis and other problems to be considered
Duodenal atresia or duodenal stenosis can be associated with other gastrointestinal and biliary tract abnormalities (malrotation, esophageal atresia, ectopic anus, annular pancreas, gallbladder or biliary atresia, vertebral anomalies). Sandrasegaran et al reviewed the records of 42 adults with annular pancreas who underwent endoscopic retrograde cholangiopancreatography (ERCP), computed tomography (CT) scanning, and magnetic resonance imaging (MRI) evaluations to determine whether annular pancreas can be diagnosed without radiologic findings of a complete ring of pancreatic tissue, and they found that of 24 patients who had CT scan or MRI findings of annular pancreas, 9 had a radiologically incomplete ring of pancreatic tissue surrounding the second part of the duodenum. [10] Three of 9 patients had gastric outlet obstruction, and 6 of 15 patients with complete annular pancreas were also found to have gastric outlet obstruction.
The Sandrasegaran et al study demonstrated a 92% sensitivity and 100% specificity for annular pancreas when pancreatic tissue was present posterolateral to the second part of the duodenum. [10] In addition, there was a 37% rate of pancreatic divisum and a 48% rate of chronic pancreatitis. Sandrasegaran et al also observed that a crocodile jaw configuration of pancreatic tissue was suggestive of annular pancreas. [10]
Duodenal atresia can also be associated with a duodenal diaphragm, as well as with congenital abnormalities in other systems. Examples include VATER (vertebral defects, anal atresia, tracheoesophageal fistula with esophageal atresia, radial and renal anomalies) association and VACTERL (vertebral, anal, cardiac, tracheal, esophageal, renal, limb) syndrome. [11, 12, 13]
Anomalies of the kidneys can occur in VATER association; the most common of these renal abnormalities include aplasia, dysplasia, hydronephrosis, ectopia, persistent urachus, vesicoureteral reflux, and ureteropelvic obstruction.
Ruptured abdominal aortic aneurysm and midgut volvulus are considered in the differential diagnosis of duodenal atresia and duodenal stenosis. In addition, other conditions to be considered include a preduodenal portal vein, Ladd bands, duplication of the duodenum, tumor or hematoma of the duodenum, and a retroperitoneal tumor.
Radiography
The double-bubble sign represents dilatation of the stomach and duodenum (see the images below). This configuration most commonly occurs with duodenal atresia and an annular pancreas. An annular pancreas is almost always associated with duodenal atresia.
 Anteroposterior radiograph of the abdomen depicts the double-bubble sign of duodenal atresia. Note the flattened acetabular angles and broadened ilia of a patient with trisomy 21.
Anteroposterior radiograph of the abdomen depicts the double-bubble sign of duodenal atresia. Note the flattened acetabular angles and broadened ilia of a patient with trisomy 21.
 Anteroposterior projection of the chest and abdomen demonstrates the double-bubble sign of duodenal atresia in the abdomen, as well as a proximal dilated pouch (right arrow) resulting from esophageal atresia; this displaces the trachea (left arrow) toward the right side in the superior mediastinum. The presence of air in the stomach and duodenum is related to the existence of a distal fistula.
Anteroposterior projection of the chest and abdomen demonstrates the double-bubble sign of duodenal atresia in the abdomen, as well as a proximal dilated pouch (right arrow) resulting from esophageal atresia; this displaces the trachea (left arrow) toward the right side in the superior mediastinum. The presence of air in the stomach and duodenum is related to the existence of a distal fistula.
In a few cases of duodenal atresia, air can be observed distal to the area of obstruction. The anomalous hepatopancreatic ducts permit movement of air through a Y-shaped ductal system, with 1 limb proximal to the obstruction and 1 limb distal to the atresia (see the following image).
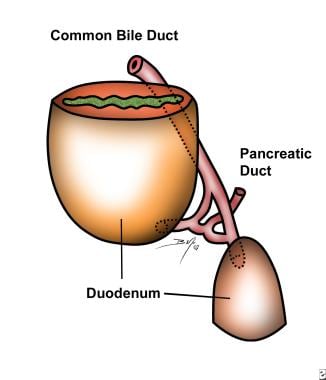 Diagram of a hepatopancreatic ductal anomaly, which permits air to move distal to the obstruction in duodenal atresia.
Diagram of a hepatopancreatic ductal anomaly, which permits air to move distal to the obstruction in duodenal atresia.
When duodenal atresia is combined with esophageal atresia, no air is observed in the stomach. Because the stomach is obstructed at both ends, the infant presents with a large, opaque upper midabdominal mass. If esophageal atresia exists along with a distal fistula, air is found in the stomach and duodenum.
Duodenal obstruction in the neonate may be partial or complete, and it may be secondary to intrinsic or extrinsic abnormalities. The duodenal bulb may be larger in duodenal atresia than in obstructions of the duodenum. Increased intramural pressure in duodenal obstruction can result in gastric pneumatosis.
Once the radiographic finding of a double-bubble sign without distal gas is determined, the diagnosis of duodenal atresia is evident, and usually no additional contrast-enhanced studies are needed.
Duodenal atresia that is associated with a Y-shaped biliary duct connection can have air distal to the point of duodenal atresia. This finding may suggest stenosis rather than atresia (see the following image).
-
Types of duodenal recanalization anomalies. Dilatation of the proximal normal segment is seen in each type. A. Diaphragm. B. Solid cord and atresia. C. Segmental absence.
-
Anteroposterior radiograph of the abdomen depicts the double-bubble sign of duodenal atresia. Note the flattened acetabular angles and broadened ilia of a patient with trisomy 21.
-
Lateral radiograph demonstrates the double-bubble sign of duodenal atresia.
-
Anteroposterior projection of the chest and abdomen demonstrates the double-bubble sign of duodenal atresia in the abdomen, as well as a proximal dilated pouch (right arrow) resulting from esophageal atresia; this displaces the trachea (left arrow) toward the right side in the superior mediastinum. The presence of air in the stomach and duodenum is related to the existence of a distal fistula.
-
Barium air contrast–enhanced study of the duodenal membrane (arrows) in the lateral projection shows a small amount of barium exiting into the more distal bowel. Coincidentally, 2 coronal cleft vertebrae are noted.
-
Anteroposterior radiograph demonstrates an enlarged duodenum, representing duodenal stenosis. Air is observed distally.
-
Diagram of a hepatopancreatic ductal anomaly, which permits air to move distal to the obstruction in duodenal atresia.






