Practice Essentials
As the nucleus pulposus loses its turgor and the elasticity of the anulus diminishes, the disk bulges outward beyond the vertebral body margins, causing bulging of the disk. Herniation of the nucleus pulposus (HNP) through an anular defect causes focal protrusion of the disk material beyond the margins of the adjacent vertebral endplate, resulting in disk herniation. [1, 2, 3, 4, 5]
Trauma is the single most common cause of rupture of the nucleus pulposus through the anulus fibrosus. The result is protrusion or extrusion of the disk material into the vertebral canal. This outcome can be caused by a single event or by repeated trauma. Predisposition to degeneration is also a factor. Alterations in the vertebral endplate cause loss of disk nutrition and disk degeneration.
MRI is the imaging modality of choice. Herniated disks are often seen on MRI in asymptomatic patients, but imaging is not indicated in patients who have signs and symptoms of a stable herniated disk until the patient has had 6 weeks of persistent symptoms. [6]
(See the images of disk herniation, below.)
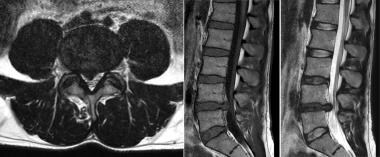
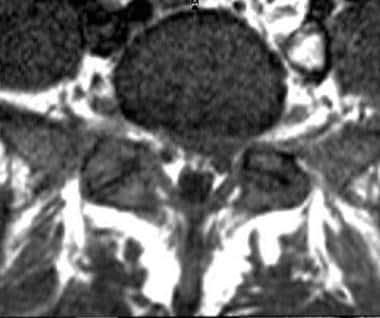 Axial T1-weighted image shows protrusion of a left paracentral disk with compression of left S1 root.
Axial T1-weighted image shows protrusion of a left paracentral disk with compression of left S1 root.
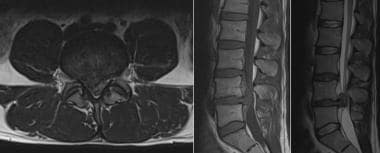
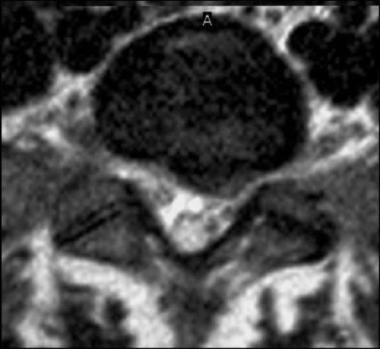 Axial T2-weighted image shows protraction of a left paracentral disk with compression of left S1 root (same patient as in previous image).
Axial T2-weighted image shows protraction of a left paracentral disk with compression of left S1 root (same patient as in previous image).
 Axial CT myelogram shows a posterior central disk extrusion present at the L1-2 level; it compresses the proximal cauda equina.
Axial CT myelogram shows a posterior central disk extrusion present at the L1-2 level; it compresses the proximal cauda equina.
 Axial CT myelogram shows posterior, central disk protrusion present at the T11-12 level. Mild cord compression is noted.
Axial CT myelogram shows posterior, central disk protrusion present at the T11-12 level. Mild cord compression is noted.
Other potentiating factors include the following [7, 8, 9] :
-
Age
-
Apoptosis
-
Abnormalities in collagen
-
Vascular ingrowth
-
Loads placed on the disk
-
Abnormal proteoglycan
-
Obesity
-
Sedentary lifestyle
-
Poor physical fitness
The North American Spine Society (NASS), the American Society of Neuroradiology (ASNR), and the American Society of Spine Radiology (ASSR) are joint task forces overseeing the standardization of the terms used to define conditions of the lumbar disk. This article reflects the work of those task forces. Although the principles and most of the definitions used in this article are focused on the lumbar spine, they are easily applied to the cervical and thoracic spine. [4]
Normal disk
The term normal applies to disks that are morphologically normal, without consideration of the clinical context. It means they are free of any changes of disease, trauma, or aging. This class does not include disks with degenerative, developmental, or adaptive changes that may be considered clinically normal in some contexts (eg, disks that have undergone typical changes associated with aging, scoliosis, or spondylolisthesis would not be considered normal). However, the bilocular appearance of the adult nucleus resulting from the development of a central horizontal band of fibrous tissue is considered a sign of normal maturation. [4]
Degeneration
Because of confusion in differentiating changes of pathologic degenerative process from those of normal aging, the classification of degenerated disk includes all such changes. Degenerative changes in the disk represent a broad category that includes the subcategories of annular fissure, herniation, and degeneration. [4]
Degeneration may include any or all of the following: real or apparent desiccation; fibrosis; narrowing of the disk space; diffuse bulging of the annulus beyond the disk space; extensive fissuring (eg, numerous annular fissures) and mucinous degeneration of the annulus; intradiskal gas; defects and sclerosis of the endplates; and the occurrence of osteophytes at the vertebral apophyses.
Annular Fissures
Annular fissures are separations between the annular fibers or separations of annular fibers from their attachments to the vertebral bone. Relatively wide annular fissures have sometimes been called annular gaps, but this term is not currently accepted as standard. Fissures may be classified by their orientation: concentric is a separation or delamination of annular fibers parallel to the peripheral contour of the disk; radial fissure is a vertically, horizontally, or obliquely oriented separation of or rent in annular fibers extending from the nucleus peripherally to or through the annulus; and a transverse fissure is a horizontally oriented radial fissure. [4]
Annular fissures have been shown to be associated with low back pain, and typically, simple symptomatic annular fissures without disk herniation can be treated with nonsteroidal anti-inflammatory drugs (NSAIDs) and low-impact physical therapy. Chronic pain due to annular fissures can be caused by granulation tissue or in-growth of nerve endings, which is usually seen near the dorsal root ganglion. [10, 11]
Herniation
Herniation is defined as a localized or focal displacement of disk material beyond the limits of the intervertebral disk space. The disk material may be nucleus, cartilage, fragmented apophyseal bone, annular tissue, or any combination thereof. The endplates of the vertebral body define the disk space cranially and caudally; the outer edges of the vertebral ring apophyses, exclusive of osteophytic formations, define it peripherally. The term localized or focal refers to the extension of the disk material less than 25% (90º) of the periphery of the disk as viewed in the axial plane. To be considered herniated, disk material must be displaced from its normal location and not simply represent an acquired growth beyond the edges of the apophyses. Herniated disks may be considered as protrustion or extrusion. [4]
Bulging
The presence of disk tissue extending beyond the edges of the ring apophyses throughout the circumference of the disk is called bulging and is not considered a herniation. Bulging involves greater than 25% of the circumference of the disk and typically extends a relatively short distance, usually less than 3 mm, beyond the edges of the apophyses. [4]
Protrusion
Disk protrusions are focal or localized abnormalities of the disk margin that involve less than 25% of the disk circumference. Protrusion, a type of herniation, is present if the greatest distance between the edges of the disc material outside the disk space is less than the distance between the edges of the base of the disk material extending outside the disk space. [4]
Extrusion
Extrusion is present when, in at least one plane, any one distance between the edges of the disk material beyond the disk space is greater than the distance between the edges of the base of the disk material beyond the disk space, or when there is no continuity between the disk material beyond the disk space and that within the disk space. [4]
Trauma
Trauma includes disruption of the disk associated with physical and/or imaging evidence of violent fracture and/or dislocation and does not include repetitive injury, contribution of less than violent trauma to the degenerative process, fragmentation of the ring apophysis in conjunction with disk herniation, or disk abnormalities in association with degenerative subluxations. [4]
Containment and Continuity
Herniated disk material can be either contained — a term that refers to the integrity of the outer annulus covering the disk herniation — or uncontained. In cases of contained herniation, fluid that is injected into the disk does not leak into the vertebral canal. The test of containment is whether the displaced disk tissues are wholly held within intact outer annulus and/or posterior longitudinal ligament fibers.
Displaced disk fragments are sometimes characterized as free. A fragment should be considered free, or sequestrated, only if there is no continuity of disk material between the fragment and the disk of origin.
The terms migrated disk and migrated fragment refer to displacement of disk material away from the opening in the annulus through which the material extrudes. Some migrated fragments are sequestrated, but the term migrated refers only to the position and not to continuity.
Regarding the posterior longitudinal ligament (PLL), displaced disk material may be described as subligamentous, extraligamentous, transligamentous, or perforated. The term subligamentous is favored as an equivalent to contained. The terms capsule and subcapsular have been used to refer to containment by an unspecified combination of annulus and ligament but are nonpreferred terms. [4] .
Volume and Composition of Displaced Material
Canal compromise of less than one third of the canal at that section is classified as mild. Compromise of one to two thirds is classified as moderate, and compromise of over two thirds is classified as severe. The same grading system can be applied to foraminal involvement.
Composition of the displaced material may be characterized by terms such as nuclear, cartilaginous, bony, calcified, ossified, collagenous, scarred, desiccated, gaseous, or liquefied.
From central to right lateral in the axial (horizontal) plane, the location may be defined as central, right central, right subarticular, right foraminal, or right extraforaminal. [4]
Preferred examination
Preferred examinations for the evaluation of disk herniation include MRI of the spine (lumbosacral, thoracic, or cervical images), bone scanning, and CT scanning of the spine (lumbosacral, thoracic, or cervical images). [12, 1, 13, 14, 15, 16, 17, 18]
Additional tests, when indicated, include assessments of any of the following, alone or in combination: erythrocyte sedimentation rate (ESR), serum glucose level, prostate-specific antigen (PSA) concentration, alkaline phosphatase value, serum protein immunoelectrophoresis result, and urine findings for Bence Jones protein.
Myelography with CT scanning is usually indicated in the following conditions: when surgery is contemplated in cases of spinal stenosis; with lateral recess stenosis; with multiple abnormal disks; with spondylolisthesis; with possible neoplasm; and after severe trauma. [1]
Regarding limitations of MRI, some individuals with implanted devices (eg, pacemakers) or with metal in their body may not be able to undergo MRI because pacemaker dysfunction and/or electrode heating are possible adverse effects of MRI. Although changing the gradient fields can induce currents in leads, the radiofrequency (RF) pulses are typically the cause of inappropriate pacing. [13, 19]
The physician ordering MRI and the MRI staff must determine whether it is safe for the patient to be examined with MRI. Patients undergoing MRI lie on a table that slides into the MRI unit. MRI of the head or neck area requires the patient's head and upper body to enter a narrow canal. Individuals with claustrophobia may require light sedation to improve their ability to tolerate the closeness of the machine. Although open MRI is an option for patients with claustrophobia, open MRI units are usually equipped with weak magnets (strength measured in Tesla units), which may prevent depiction of fine details. To obtain the best images, the patient must not move during the examination. Some patients and small children undergoing MRI may require sedation to ensure that they remain still. [15, 18, 20, 21, 22]
Although conventional radiographs probably show cortical bone better than MRIs do, the bone marrow is best imaged with MRI, and MRI is superior for demonstrating most bone abnormalities. MRI may be useful for predicting the likelihood that a patient with lumbar disk herniation will require microdiskectomy. [23]
CT is preferred for unstable patients with severe bleeding. MRI may not always be useful for distinguishing between tumor tissue and edema fluid, and it does not depict calcium well when it is present in a tumor.
MRI is generally avoided during the first 12 weeks of pregnancy, though the hazards of MRI use during this period have not been proven. Severe obesity limits MRI of the spine. Postoperative scarring and/or edema and surgical instrumentation with rods and screws can limit results of the study. [24]
Limitations of techniques
A meta-analysis of 14 studies and 940 patients who underwent MRI, CT, or myelography for lumbar disk herniation reported comparable accuracy among the modalities (see Table 1). [25]
Table 1. Sensitivity and Specificity of Imaging Modalities [25] (Open Table in a new window)
| Modality | Sensitivity | Confidence Interval (CI) | Specificity | Confidence Interval (CI) |
|---|---|---|---|---|
| MRI | 80.9% | 95%CI: 68.8–89.1% | 81.0% | 95%CI: 59.2–92.6% |
| CT | 81.3% | 95%CI: 72.3–87.7% | 77.1% | 95%CI: 61.9–87.5% |
| Myelography | 75.7% | 95%CI: 64.9–84.1% | 76.5% | 95%CI: 67.8–83.4% |
The researchers noted that there are no data on modern imaging, as all but one study in the analysis were published between 1984 and 1994. Additionally, no data were found on the rates of false positive or negative results. [25]
General diagnostic testing and surgery
Diagnostic testing for herniated disk includes MRI, CT, myelography, and plain radiography, either alone or in different combinations, as the occasion demands. Surgery should occur only when objective findings of structural defects are correlated with the patient's symptoms and signs. [8, 26, 27]
Lumbar diskectomy is a common procedure for the management of lumbar radiculopathy, but recurrent lumbar disk herniation is one of the most common complications of the procedure, sometimes necessitating repeat surgery. In a systematic review and meta-analysis by Brooks et al, disk height index, Modic changes, and sagittal range of motion were found to be significantly correlated with an increased rate of recurrent lumbar disk herniation. [28]
Diskography
Diskography consists of injecting contrast medium into the disk and assessing the patient's response to the injection. Reproduction of pain similar to the patient's existing back or neck pain suggests that the disk may be the source. CT performed after diskography is often useful in assessing anatomic changes in the disk and in demonstrating pathology in the disk, including clefts and radial fissures. [29]
Early studies indicated that diskography had low specificity, but more recent studies have failed to induce pain in asymptomatic control subjects, suggesting that diskography has utility in identifying patients with diskogenic pain. Pain reproduction during diskography in symptomatic individuals is variable. The incidence of pain reproduction is lower in patients with disk degeneration than in those with posterior fissures of the annulus fibrosus or with significant disk bulges. [10]
In essence, when outcomes of fusion procedures are compared, lumbar diskography is sensitive but lacks specificity.
Diskography is recommended only when adequate attempts at conservative therapy and noninvasive diagnostic tests, such as MRI, have failed to reveal the etiology of back pain.
Specific indications for diskography include the following:
-
Investigation of persistent, severe symptoms when results of other diagnostic tests for identifying the disk that is suspected of being a source of the pain are negative.
-
Evaluation of abnormal disks, evaluation of recurrent pain from a disk that underwent previous operation, or evaluation of lateral disk herniation.
-
Evaluation of patients in whom surgery has failed, to determine whether pseudoarthrosis or a symptomatic disk in a posteriorly viewed segment could be the source of pain.
-
Evaluation of disks before fusion to determine whether the disks of the proposed fusion segment are symptomatic and whether the disks adjacent to this segment can support a fusion.
-
Evaluation of patients with a confirmed disk herniation as candidates for minimally invasive surgery.
Complications associated with diskography include the following [30] :
-
Spinal headache
-
Meningitis
-
Diskitis
-
Intrathecal hemorrhage
-
Arachnoiditis
-
Severe reaction to accidental intradural injection
-
Damage to the disk
-
Urticaria
-
Retroperitoneal hemorrhage
-
Nausea
-
Seizures
-
Headache
-
Increased pain
One study identified radiographic features of degeneration in the disks of patients 10 years after undergoing diskography; however; with modern techniques utilizing lower pressures, the actual risk is likely to be minimal. [31] Herniated nucleus pulposus is not a complication related to diskography. With prophylactic use of antibiotics, the incidence of diskitis is significantly reduced.
The Modified Dallas Classification system is based on contrast extravasation seen on coronal CT imaging through the disk itself. The different categories in the Modified Dallas Diskogram Classification describe the severity of the radial annular tear, as follows [32] :
-
Grade 0 is a normal disk—no contrast material leaks from the nucleus.
-
Grade 1 tear will leak contrast material into the inner 1/3 of the annulus.
-
Grade 2 tear will leak contrast through the inner 1/3 and into the middle 1/3 of the disk.
-
Grade 3 tear will leak contrast through the inner and middle annulus. The contrast spills into the outer 1/3 of the annulus.
-
Grade 4 tear includes a grade 3 tear, and the contrast is also seen spreading concentrically around the disk. The concentric spread must be greater than 30 degrees. A full-thickness radial tear and concentric annular tear merge together.
-
Grade 5 tear ('evil' grade) includes a grade 3 or grade 4 radial tear that has completely ruptured the outer layers of the disk and is leaking contrast material out of the disc. This type of tear is felt to be associated with "chemical radiculopathy," with the low pH of the nuclear material theoretically irritating nerve roots directly.
Other interventions
Other interventions include imaging procedures necessary to aid in the injection procedures and to supplement and enhance already applied active treatment in motion. They include the following:
-
Epidural steroid injections
-
Selective nerve root blocks
-
Facet joint injections
-
Trigger-point injections
Radiography
In cases of disk bulging, plain radiographs reveal indirect findings of disk degeneration in the form of loss of height of the intervertebral disk, vacuum phenomenon in the form of gas in the disk, and endplate osteophytes. Moderate bulges appear as nonfocal protrusion of disk material beyond the borders of the vertebra; this is typically broad based, circumferential, and symmetric.
In most cases of herniated nucleus pulposus (HNP), plain radiographs of the lumbosacral spine or cervical spine are not needed. Plain radiographs do not reveal disk herniation; they are usually used to exclude other conditions (eg, fracture, cancer, infection). When the clinical condition strongly suggests HNP, plain radiographs can be avoided.
Myelographic findings in patients with HNP include extradural deformity or displacement of the contrast-filled thecal sac. In addition, myelograms may show elevation, deviation, or amputation of the root sleeve and edema of the affected nerve.
When used in routine practice, magnetic resonance (MR) myelography has been shown to be of limited value. In one study, it assisted in establishing a diagnosis in only a small percentage of cases (6%). The technique was of limited additional value in patients with multilevel pathology, and it was of even less value in patients with scoliosis, for whom it was used to help establish the most likely level to account for the pathology. [15]
Computed Tomography
CT has proved to be as good as or even better than myelography alone in the diagnosis of herniated disk. CT scanning with myelography is superior to either one alone.
In subligamentous herniation, images show a focal, smooth, outward displacement of the disk margin in the spinal canal, in the neural foramen, or lateral to the neural foramen. CT scans may further demonstrate calcification or, less commonly, gas in the herniation.
In disk herniation, CT scans show a soft-tissue mass with effacement of the epidural fat and displacement of the thecal sac. If the fragment is no longer restrained by the PLL but is still in contact with the disk margin, an irregular, lobulated excrescence on the disk margin is seen. A separated disk fragment is often detected in the epidural fat adjacent to the dural sac or sheath of a nerve root. The disk margin may appear normal. The attenuation of the nuclear fragments of a fragmented disk is usually 80-120 HU.
To achieve optimal results with CT, a localizer image should be obtained at the site of pathology by using relatively thin sections and optimal resolution. A CT-based diagnosis of herniated disk is difficult in patients who have previously undergone laminectomy, because the epidural fat is partially replaced by fibrosis and the surgical scar. Deformity of the dural sac and nerve sheath, along with the bony changes, help in the diagnosis (see the images below).
 Axial CT myelogram of a large, central calcified disk extrusion present at the T5-6 level; it causes severe spinal cord compression.
Axial CT myelogram of a large, central calcified disk extrusion present at the T5-6 level; it causes severe spinal cord compression.
 Axial CT myelogram shows a posterior central disk extrusion present at the L1-2 level; it compresses the proximal cauda equina.
Axial CT myelogram shows a posterior central disk extrusion present at the L1-2 level; it compresses the proximal cauda equina.
 Sagittal reformatted CT myelogram shows a large, calcified, posterior central disk extrusion, causing severe cord compression at the T5-6 level.
Sagittal reformatted CT myelogram shows a large, calcified, posterior central disk extrusion, causing severe cord compression at the T5-6 level.
 Axial CT myelogram shows posterior, central disk protrusion present at the T11-12 level. Mild cord compression is noted.
Axial CT myelogram shows posterior, central disk protrusion present at the T11-12 level. Mild cord compression is noted.
Cervical disk
The uncinate processes project superiorly from the vertebral bodies posteriorly and laterally to the intervertebral disks. With wear and tear, disk degeneration and narrowing of the intervertebral spaces result in an abnormal relationship of the uncinate processes with adjacent vertebral body, resulting in sclerosis and hypertrophy of the uncinate processes. As the spinal canal is compromised by the degenerating disk, myelopathy results. When a similar process occurs in the neural foramen, radiculopathy is encountered. Cervical epidural space is naturally narrow; therefore, even small disk herniations and protrusions result in dural sac impingement.
Epidural fat that highlights lumbar intervertebral herniation is nearly absent in the cervical disk. In cervical DDD associated with hard disks, CT often reveals the hypertrophied uncinate processes and osteophytes along the disk margin. On CT scans, soft disks are often characterized by the dural sac indentation by the disk, with the disk having an attenuation slightly greater than that of the sac.
Thoracic disk
CT is helpful in diagnosing a thoracic disk when the region of interest, determined on the basis of clinical localization, is small. A thoracic disk frequently contains calcium, which is demonstrable on CT scans. A herniated disk may be seen as a clearly defined mass surrounded by epidural fat lateral to the dural sac. However, if the epidural fat is lacking, the disk appears as a mass of slightly increased attenuation that displaces the dural sac. CT findings vary depending on the amount of epidural fat and subarachnoid cerebrospinal fluid in the thoracic region.
Magnetic Resonance Imaging
MRI exquisitely delineates herniated nucleus pulposus (HNP) and its relationship with adjacent soft tissues. On MRI, HNPs appear as focal, asymmetric protrusions of disk material beyond the confines of the annulus. HNPs themselves are usually hypointense. However, because disk herniations are often associated with a radial annular fissure, high signal intensity in the posterior annulus is often seen on sagittal T2-weighted images. On sagittal MRIs, the relationship of HNPs and degenerated facets to exiting nerve roots within the neural foramina is well delineated. In addition, free fragments of the disk are easily detected on MRI (see the images below). [15, 16, 17, 18, 21, 22, 33, 34, 10]
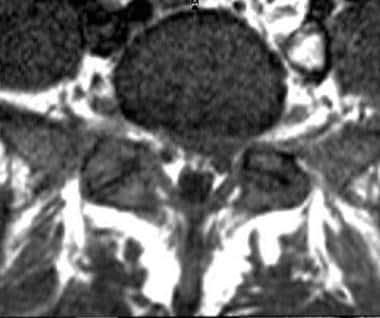 Axial T1-weighted image shows protrusion of a left paracentral disk with compression of left S1 root.
Axial T1-weighted image shows protrusion of a left paracentral disk with compression of left S1 root.
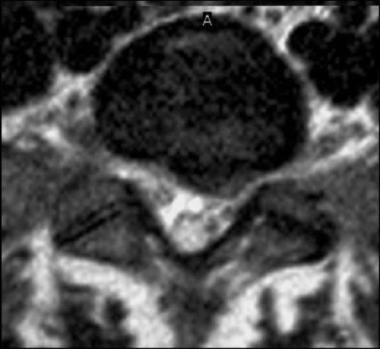 Axial T2-weighted image shows protraction of a left paracentral disk with compression of left S1 root (same patient as in previous image).
Axial T2-weighted image shows protraction of a left paracentral disk with compression of left S1 root (same patient as in previous image).
 Recurrent postoperative disk extrusion at L4-5 after L4-5 diskectomy. Axial and sagittal T1-weighted images obtained before and after contrast enhancement reveal a rim of enhancing, recurrent left central disk extrusion with downward migration.
Recurrent postoperative disk extrusion at L4-5 after L4-5 diskectomy. Axial and sagittal T1-weighted images obtained before and after contrast enhancement reveal a rim of enhancing, recurrent left central disk extrusion with downward migration.
 Right S1 radiculopathy. Sagittal T1- and T2-weighted images show a large, right central disk extrusion at L5-S1 that markedly compresses the thecal sac. The extruded disk is compressing the right S1 nerve root.
Right S1 radiculopathy. Sagittal T1- and T2-weighted images show a large, right central disk extrusion at L5-S1 that markedly compresses the thecal sac. The extruded disk is compressing the right S1 nerve root.
 Right L5 radiculopathy. Axial T1- and T2-weighted images at L4-5 show a large, right paracentral disk extrusion causing marked compression of the thecal sac. Images show compression, but the right L5 root is not visible.
Right L5 radiculopathy. Axial T1- and T2-weighted images at L4-5 show a large, right paracentral disk extrusion causing marked compression of the thecal sac. Images show compression, but the right L5 root is not visible.
 Sagittal T2-weighted imaging of lumbosacral spine shows an annular tear at L4-5 and disk protrusion at the L5-S1 levels.
Sagittal T2-weighted imaging of lumbosacral spine shows an annular tear at L4-5 and disk protrusion at the L5-S1 levels.
 Right paracentral disk herniation at L4-5. Axial T2 and sagittal T1- and T2-weighted images obtained in a patient complaining of left-sided back pain radiating into her leg with imaging findings not correlating with her symptoms.
Right paracentral disk herniation at L4-5. Axial T2 and sagittal T1- and T2-weighted images obtained in a patient complaining of left-sided back pain radiating into her leg with imaging findings not correlating with her symptoms.
 Progression of disk herniation. Axial T2 and sagittal T1- and T2-weighted images in the same patient obtained 6 weeks later shows progression of disk herniation and now superimposed disk extrusion migrating superiorly, causing severe spinal canal stenosis and severe compression of the internal cauda equina.
Progression of disk herniation. Axial T2 and sagittal T1- and T2-weighted images in the same patient obtained 6 weeks later shows progression of disk herniation and now superimposed disk extrusion migrating superiorly, causing severe spinal canal stenosis and severe compression of the internal cauda equina.
 Sagittal T1- and T2-weighted images and axial T1- and T2-weighted images show degenerative changes at the L1-2 and L2-3 levels, facet hypertrophy at the L4-5 level, and disk herniation, leading to extrusion and compressing the left L5 root.
Sagittal T1- and T2-weighted images and axial T1- and T2-weighted images show degenerative changes at the L1-2 and L2-3 levels, facet hypertrophy at the L4-5 level, and disk herniation, leading to extrusion and compressing the left L5 root.
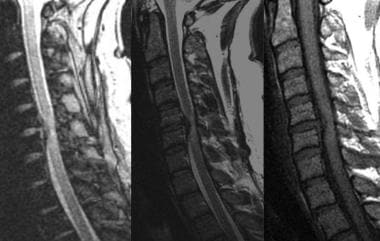 Sagittal T1- and T2-weighted gradient-echo images obtained at C5-6 show a moderate-to-severe central disk extrusion that causes cord compression with abnormal signal intensity in the cord. Gradient-echo images improve the contrast to distinguish between the hyperintense disk and the hypointense osteophytosis.
Sagittal T1- and T2-weighted gradient-echo images obtained at C5-6 show a moderate-to-severe central disk extrusion that causes cord compression with abnormal signal intensity in the cord. Gradient-echo images improve the contrast to distinguish between the hyperintense disk and the hypointense osteophytosis.
In cases of disk bulging, early findings on MRI include loss of the normal posterior disk concavity. Moderate bulges appear as nonfocal protrusions of disk material beyond the borders of the vertebrae; bulges are typically broad based, circumferential, and symmetric.
A radial fissure of the annulus fibrosus is considered a sign of early disk degeneration. It is accompanied by other signs of disk degeneration, such as a bulging annulus, loss of disk height, herniation of the nucleus pulposus, and changes in the adjacent endplates. Radial fissures of the annulus fibrosus can be detected as an area of increased signal intensity on T2-weighted and gadolinium-enhanced MRIs. There is an association between the annular fissure on MRIs and the symptomatic disks. [10, 11]
Raudner et al performed a 5-year follow-up study of 25 patients with symptomatic low back pain and found that quantitative T2 mapping may serve as a clinically feasible, noninvasive imaging biomarker that can indicate disks at risk for herniation and correlate with clinical outcome. [35]
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Uncommon findings on MRI
Uncommon HNP findings on MRI include areas of atypical signal intensity and unusual location.
Some HNPs have high signal intensity on T1- or T2-weighted MRI. Vascularized extruded fragments may show ring enhancement after the administration of contrast material. Lesions in unusual locations include extraforaminal HNPs, fragments sequestered posterior to the thecal sac, and lesions located completely outside the canal (far lateral herniations). Atypical migratory disk patterns may also be seen; occasionally, migration occurs down the root sleeve. In rare cases, HNPs penetrate the PLL and extend intradurally.
A strongly enhancing HNP may mimic a neoplasm such as an ependymoma or a tumor of the nerve sheath.
Contrast enhancement does increase the yield, though minimally. Approximately 5% of patients have abnormally enhancing nerve roots consistent with neuritis; in 70% of these patients, such findings are associated with HNP or disk bulges. In the cervical and thoracic spine, contrast enhancement increases epidural conspicuity and improves diagnostic yield. It is particularly useful in delineating foraminal pathology.
In their extensive study of HNPs, Mikhael et al found that lumbar MRI and CT results were both diagnostic in cases of herniated and extruded disks. [12] MRI provided the most information about the degenerative state of the intervertebral disks. MRI was more accurate than CT in depicting small, bulging, and herniated disks without a ruptured anulus, as well as the relation of the migrated fragments of extruded disks to the back of the vertebrae and the thecal sac. In addition, MRI was more accurate than CT in differentiating postoperative epidural fibrotic changes from recurrent herniated and/or extruded disk and in depicting distal spinal cord abnormalities. CT easily depicted laterally herniated lumbar disks. Myelography was the diagnostic study in cases of arachnoiditis.
Weishaupt et al found that positional MRI more frequently demonstrated minor neural compromise than conventional MRI. [14] Positional pain differences were related to position-dependent changes in foraminal size.
Jinkins et al studied the general clinical utility of the first dedicated MRI unit that enabled upright, weight-bearing positional MRI of the spinal column during various dynamic-kinetic maneuvers (kinetic MRI) in patients with degenerative conditions of the spine. [2] Upright, weight-bearing positional MRI is thought by some to be useful.
Taneichi et al studied HNPs with gadolinium-enhanced MRI and reported that this technique depicted not only the morphology but also the pathologic changes associated with nerve root compression by herniated disk. [36] Enhanced MRI was performed in 115 patients who were surgically treated for lumbar disk herniation. Nerve root enhancement was seen in 39.1% before surgery and in 58.7% after surgery. Preoperative root enhancement reflected the intensity of radicular pain rather than the degree of neurologic deficits; by contrast, postoperative enhancement was not correlated with radicular symptoms.
Nerve root enhancement represents intraneural edema in the affected nerve root. Enhanced MRI has the potential for identifying an affected nerve root in patients in whom there is a discrepancy between the level of disk herniation and neurologic manifestations. [15, 16, 3, 20, 37]
-
Axial T1-weighted image shows protrusion of a left paracentral disk with compression of left S1 root.
-
Axial T2-weighted image shows protraction of a left paracentral disk with compression of left S1 root (same patient as in previous image).
-
Recurrent postoperative disk extrusion at L4-5 after L4-5 diskectomy. Axial and sagittal T1-weighted images obtained before and after contrast enhancement reveal a rim of enhancing, recurrent left central disk extrusion with downward migration.
-
Right S1 radiculopathy. Sagittal T1- and T2-weighted images show a large, right central disk extrusion at L5-S1 that markedly compresses the thecal sac. The extruded disk is compressing the right S1 nerve root.
-
Right L5 radiculopathy. Axial T1- and T2-weighted images at L4-5 show a large, right paracentral disk extrusion causing marked compression of the thecal sac. Images show compression, but the right L5 root is not visible.
-
Sagittal T2-weighted imaging of lumbosacral spine shows an annular tear at L4-5 and disk protrusion at the L5-S1 levels.
-
Right paracentral disk herniation at L4-5. Axial T2 and sagittal T1- and T2-weighted images obtained in a patient complaining of left-sided back pain radiating into her leg with imaging findings not correlating with her symptoms.
-
Progression of disk herniation. Axial T2 and sagittal T1- and T2-weighted images in the same patient obtained 6 weeks later shows progression of disk herniation and now superimposed disk extrusion migrating superiorly, causing severe spinal canal stenosis and severe compression of the internal cauda equina.
-
Sagittal T1- and T2-weighted images and axial T1- and T2-weighted images show degenerative changes at the L1-2 and L2-3 levels, facet hypertrophy at the L4-5 level, and disk herniation, leading to extrusion and compressing the left L5 root.
-
Axial CT myelogram of a large, central calcified disk extrusion present at the T5-6 level; it causes severe spinal cord compression.
-
Axial CT myelogram shows a posterior central disk extrusion present at the L1-2 level; it compresses the proximal cauda equina.
-
Sagittal reformatted CT myelogram shows a large, calcified, posterior central disk extrusion, causing severe cord compression at the T5-6 level.
-
Axial CT myelogram shows posterior, central disk protrusion present at the T11-12 level. Mild cord compression is noted.
-
Sagittal T1- and T2-weighted gradient-echo images obtained at C5-6 show a moderate-to-severe central disk extrusion that causes cord compression with abnormal signal intensity in the cord. Gradient-echo images improve the contrast to distinguish between the hyperintense disk and the hypointense osteophytosis.






