Practice Essentials
Paraspinal ligaments undergo degeneration secondary to attrition, and they often ossify, a condition broadly termed spinal enthesopathy. Physicians recognize Forestier disease [1] (involves the anterior longitudinal ligament), diffuse idiopathic skeletal hyperostosis (DISH) (more diffuse variant of Forestier disease that exhibits additional extra-axial features), and ossification of the posterior longitudinal ligament (OPLL) as being associated with this phenomenon. [2] Clinically, DISH is often referred to as senile ankylosing spondylitis, because there are similarities in appearance between the 2 conditions; however, DISH and ankylosing spondylitis differ in their age of onset. [3, 4, 5, 6]
DISH has rarely been reported in patients younger than 50 years. In persons older than 50 years, DISH occurs in about 25% of males and 15% of females, with rates reaching 28% in men and 26% in women after 80 years of age. In the general population, the incidence has been reported to be 6-12%. [6]
In a population-based cohort study called Research on Osteoarthritis/osteoporosis Against Disability (ROAD), whole-spine radiographs of 1,647 individuals showed DISH prevalence of 10.8%. The rate was significantly higher for patients who were older (72.3 years), were male, had a higher body mass index, had lumbar spondylosis, and had knee osteoarthritis. [7]
Of 938 patients recruited from a University of Toronto psoriatic arthritis (PsA) observational cohort, 78 (8.3%) were found to have DISH. Patients with DISH were older and had longer disease duration, higher body mass index, and higher uric acid levels. In addition, diabetes and hypertension were more prevalent in patients with DISH than in those without. The severity of radiographic damage to peripheral joints was also greater in patients with DISH. [8]
Peripheral involvement of DISH can include elbows, metacarpophalangeal joints, and shoulders, which are not commonly associated with osteoarthritis. [9] Patients with DISH are at increased risk for spinal fractures and spinal cord injuries. Elderly patients suffering traumatic spinal cord injuries due to falls from a standing/sitting height have been reported. [10, 11]
(See the following images depicting diffuse idiopathic skeletal hyperostosis.)
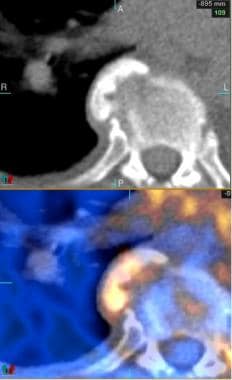 Positron emission tomography (PET)/CT image (axial cut, anterior view) through a midthoracic vertebral body demonstrates focal hypermetabolism within a large right-sided anterolateral bony excrescence.
Positron emission tomography (PET)/CT image (axial cut, anterior view) through a midthoracic vertebral body demonstrates focal hypermetabolism within a large right-sided anterolateral bony excrescence.
 Bone scan (posterior image) demonstrates increased uptake along the right anterolateral aspect of more than 4 thoracic vertebrae.
Bone scan (posterior image) demonstrates increased uptake along the right anterolateral aspect of more than 4 thoracic vertebrae.
 Radiograph of the lumbosacral spine (anteroposterior view) showing flowing osteophytes and soft-tissue ligamentous ossification consistent with diffuse idiopathic skeletal hyperostosis.
Radiograph of the lumbosacral spine (anteroposterior view) showing flowing osteophytes and soft-tissue ligamentous ossification consistent with diffuse idiopathic skeletal hyperostosis.
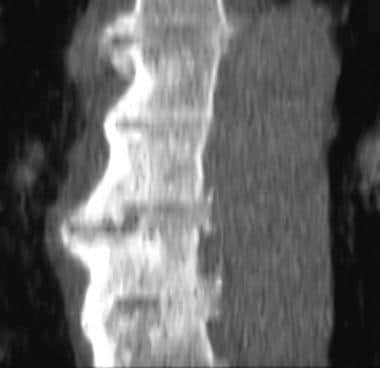
 Sagittal, T2-weighted magnetic resonance image of the cervical spine showing ossification of the posterior longitudinal ligament. Courtesy of A. Vincent Thamburaj, MD, Apollo Hospital, Chennai, India.
Sagittal, T2-weighted magnetic resonance image of the cervical spine showing ossification of the posterior longitudinal ligament. Courtesy of A. Vincent Thamburaj, MD, Apollo Hospital, Chennai, India.
Preferred examination
Radiography of the spine is the single most useful imaging modality in the diagnosis of DISH. However, patient body habitus or an inability of the patient to lie on his or her side for a lateral view may compromise the quality of radiographs. In addition, radiographs are inadequate for evaluating the extent of the compression caused by the large syndesmophytes on the trachea, bronchi, or esophagus. In this case, CT scanning of the spine is helpful and is aided by coronal and sagittal reconstructions. CT scanning may be performed to evaluate complications, such as fracture, or symptoms caused by pressure effects on the trachea, esophagus, and veins. [4, 12, 13, 14, 2, 15, 16]
CT scanning usually is not cost-effective for imaging the entire spine and provides limited information about spinal cord involvement. In this situation, MRI is of benefit and thus is reserved primarily for evaluating possible cord compression. This is especially true if DISH is associated with ossification of the posterior longitudinal ligament (OPLL), as it is in a minority of patients. [17, 2, 18] In a study by Nishimura et al of 234 patients with OPLL who underwent whole-spine CT, the prevalence of DISH in patients with cervical OPLL was 48.7%. [2]
The differential diagnosis includes ankylosing spondylitis, neuropathic arthropathy (Charcot joint), primary osteoarthritis, and psoriatic arthritis. Musculoskeletal involvement in Reiter syndrome is another condition to be considered.
Sacroiliac (SI) joint MRI may be more helpful than MRI of the spine in differentiating DISH from axial spondyloarthritis (SpA) in the elderly. [19] MRI may also be useful in differentiating DISH from ankylosing spondylitis, as MRI may show inflammatory changes that are typical of ankylosing spondylitis. [9]
Studies with MRI and ultrasonography have suggested that a local entheseal inflammatory process may precede the ossification process. [15, 20, 18]
DISH diagnostic criteria
The following features are used to diagnose DISH on the basis of the Resnick and Niwayama criteria [17, 21] :
-
Flowing calcifications and ossifications along the anterolateral aspect of at least 4 contiguous vertebral bodies, with or without osteophytes.
-
Preservation of intervertebral disk height in the involved areas and an absence of excessive disk disease.
-
Absence of bony ankylosis of facet joints and absence of sacroiliac erosion, sclerosis, or bony fusion, although narrowing and sclerosis of facet joints are acceptable. [3]
The Julkunen criteria are as follows [21] :
-
Substantially the same as the Resnick and Niwayama criteria but slightly different in that bridges connecting the 2 vertebral bodies in at least 2 sites on the thoracic spine are included.
The Ulsinger criteria include the following [21] :
-
Definite DISH: Bridging of 4 contiguous vertebral bodies primarily in the thoracolumbar spine, minimal intervertebral disk disease, and no facet joint ankylosis.
-
Probable DISH: Bridging of 2 contiguous vertebral bodies plus bilateral patellar tufting, heel spurring, and olecranon tufting.
-
Possible DISH: Two vertebrae joined in the absence of extraspinal enthesophytes or symmetrical extraspinal enthesophytes in the absence of spinal involvement.
Unlike ankylosing spondylitis, DISH does not involve the sacroiliac joint. DISH is also distinct from marginal osteophytes that form in response to degenerative disk disease. Patients with DISH infrequently demonstrate disk height reduction or vacuum changes.
Lower thoracic spine involvement is typical of DISH, but the lumbar and cervical spine can also be affected. The left side of the spine is typically spared or less involved, which is probably attributable to the pulsating aorta. Forestier disease includes many extra-axial features, such as ossification of other ligaments and tendons, as well as subcutaneous calcification. [1]
Radiography
Radiographs of the spine in patients with diffuse idiopathic skeletal hyperostosis (DISH) typically demonstrate thoracic spinal involvement; however, this condition can also affect the lumbar and cervical spine. DISH is distinguished by the presence of flowing syndesmophytes along, but separated from, the anterior aspect of the vertebral bodies, involving at least 4 levels. The disease begins as fine ossification, 1- to 2-mm thick, but ossification may thicken to as much as 20 mm as the disease progresses.
Extra-axial radiographic findings in DISH include ossification of the nuchal ligaments of the skull; enthesopathy at the ischial tuberosities in the pelvis, as well as ossification of the sacrotuberous ligament and the symphysis pubis; ossification of the triceps tendon in the upper extremities, and subcutaneous calcification of the skin.
(The following radiographs show DISH.)
 Radiograph of the lumbosacral spine (anteroposterior view) showing flowing osteophytes and soft-tissue ligamentous ossification consistent with diffuse idiopathic skeletal hyperostosis.
Radiograph of the lumbosacral spine (anteroposterior view) showing flowing osteophytes and soft-tissue ligamentous ossification consistent with diffuse idiopathic skeletal hyperostosis.
 Radiograph of the lumbosacral spine (lateral view) showing flowing anterior osteophytes indicative of diffuse idiopathic skeletal hyperostosis.
Radiograph of the lumbosacral spine (lateral view) showing flowing anterior osteophytes indicative of diffuse idiopathic skeletal hyperostosis.
 Radiograph of the thoracic spine (anteroposterior view) showing osteophytes on the right side only, a feature typical of diffuse idiopathic skeletal hyperostosis.
Radiograph of the thoracic spine (anteroposterior view) showing osteophytes on the right side only, a feature typical of diffuse idiopathic skeletal hyperostosis.
The hallmark of DISH is ossification occurring along the anterior aspect of the vertebral bodies but remaining separate from the vertebrae. Osteophytes of degenerative spinal disease usually occur along the anterolateral aspect. The location of the ossification distinguishes DISH from ossification of the posterior longitudinal ligament (OPLL). [22, 2]
Omnipresent degenerative osteophytes represent the most common finding that mimics DISH; however, DISH is defined by the strict criteria of anterior location and the bridging involvement of 4 contiguous vertebral bodies (3 intervertebral disk spaces).
Computed Tomography
CT scanning is usually not indicated in diffuse idiopathic skeletal hyperostosis (DISH), unless there is a need to evaluate complications, such as fracture, spinal canal stenosis secondary to associated ossification of the posterior longitudinal ligament (OPLL), and pressure effects on the esophagus or inferior vena cava. [23, 2] In a study by Nishimura et al of 234 patients with OPLL who underwent whole-spine CT, the prevalence of DISH in patients with cervical OPLL was 48.7%. [2]
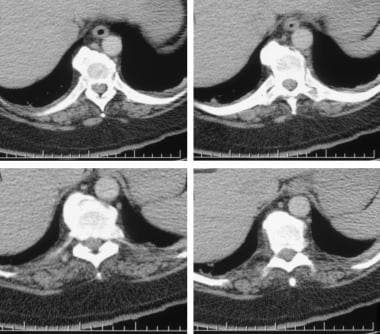
CT scans show ossification along the anterior aspect (see the following image), and coronal reconstruction depicts the classic pattern.
The same criteria used in radiographic evaluation (the location of the ossification and an involvement over at least 4 vertebral bodies) define DISH and distinguish this entity from degenerative osteophytes.
Prominent pelvic enthesophytes on CT have been able to discriminate between DISH and non-DISH patients. In one study, anterior superior iliac spine and greater trochanter enthesophytes significantly distinguished between patients with DISH and those without DISH. [24]
Magnetic Resonance Imaging
MRI of the spine is usually not indicated in diffuse idiopathic skeletal hyperostosis (DISH), because the diagnosis is made using plain radiographic findings. CT scanning, using coronal and sagittal reconstruction, is useful because it provides better anatomic definition. When associated ossification of the posterior longitudinal ligament (OPLL) causes neurologic symptoms, MRI is valuable for determining the extent of the ossification, the mass effect on the thecal sac, and the presence of cord compression. [2] Typically, DISH manifests as a long segment of low T1 and T2 signals that is anterior to several contiguous vertebrae, whereas OPLL manifests as a signal that is posterior to the vertebral body and that extends for several segments. Cord edema manifests as a high T2 signal. [12, 25]
(See the image below.)
 Sagittal, T2-weighted magnetic resonance image of the cervical spine showing ossification of the posterior longitudinal ligament. Courtesy of A. Vincent Thamburaj, MD, Apollo Hospital, Chennai, India.
Sagittal, T2-weighted magnetic resonance image of the cervical spine showing ossification of the posterior longitudinal ligament. Courtesy of A. Vincent Thamburaj, MD, Apollo Hospital, Chennai, India.
Nuclear Imaging
In nuclear medicine, bone scanning is usually requested for the evaluation of back pain, revealing the nonspecific pattern of the diffusely increased and heterogeneous uptake of radiopharmaceutical agents in the spine (see the image below). Diagnosis relies primarily on the use of radiographs. The appearance of diffuse idiopathic skeletal hyperostosis (DISH) on a bone scan is nonspecific, and without radiographic correlation, diagnosis is difficult.
 Bone scan (posterior image) demonstrates increased uptake along the right anterolateral aspect of more than 4 thoracic vertebrae.
Bone scan (posterior image) demonstrates increased uptake along the right anterolateral aspect of more than 4 thoracic vertebrae.
PET/CT imaging
Positron emission tomography (PET) imaging reveals which "flowing osteophytes" (bony excrescences) are metabolically active; this cannot be ascertained using radiographic, CT, or MRI studies.
The increased metabolism can be associated with patient symptomatology; however, and more importantly, the use of PET imaging helps distinguish a metastatic vertebral deposit from a metabolically active osteophyte by its lower metabolic rate and its configuration on the fused PET/CT image.
(See the image below.)
-
Radiograph of the lumbosacral spine (anteroposterior view) showing flowing osteophytes and soft-tissue ligamentous ossification consistent with diffuse idiopathic skeletal hyperostosis.
-
Radiograph of the lumbosacral spine (lateral view) showing flowing anterior osteophytes indicative of diffuse idiopathic skeletal hyperostosis.
-
Radiograph of the thoracic spine (anteroposterior view) showing osteophytes on the right side only, a feature typical of diffuse idiopathic skeletal hyperostosis.
-
Lateral reconstruction computed tomography (CT) scan showing anterior syndesmophytes.
-
Sagittal, T2-weighted magnetic resonance image of the cervical spine showing ossification of the posterior longitudinal ligament. Courtesy of A. Vincent Thamburaj, MD, Apollo Hospital, Chennai, India.
-
Computed tomography (CT) scans showing large, flowing syndesmophytes.
-
Positron emission tomography (PET)/CT image (axial cut, anterior view) through a midthoracic vertebral body demonstrates focal hypermetabolism within a large right-sided anterolateral bony excrescence.
-
Bone scan (posterior image) demonstrates increased uptake along the right anterolateral aspect of more than 4 thoracic vertebrae.