Practice Essentials
Developmental dysplasia of the hip (DDH) is a spectrum of disorders affecting the proximal femur and acetabulum that leads to hip subluxation and dislocation. It results from abnormal hip development and presents in infancy or early childhood ranging from dysplasia to dislocation of the hip joint. DDH is the most common congenital abnormality of the musculoskeletal system. Early diagnosis and treatment is important because failure to diagnose DDH in neonates and young infants can result in significant morbidity. [1, 2, 3, 4, 5, 6, 7, 8]
An Austrian orthopedist, Reinhard Graf, first introduced US examination of the hip in 1980. [9] His technique included the calculation of numerous angles, a complicated classification system of hip subtypes, and the orientation of the B-mode images, so that all hips were displayed on right coronal projections. Proponents of static scanning cite that it is fast, easy to perform, and reproducible. Widespread usage in Western Europe has reduced the incidence of undetected DDH requiring open reduction to the lowest in the world. [10, 11, 12]
With the advent of real-time US in 1984, H. Theodore Harcke and associates at the DuPont Institute in Wilmington, Delaware, introduced a dynamic approach to studying the hips. Harcke is the principal drafter of the American College of Radiology (ACR) standard, and his dynamic approach is predominantly used in US examination. [13] There is no conclusive evidence to prefer one method over the other. However an effective ultrasonographic method should include simple, precise, quantitative and consistent definitions for a proper examination and diagnosis. [14]
Imaging modalities
Ultrasonography (US) is the preferred modality for evaluating the hip in infants who are 6 months or younger. US enables direct imaging of the cartilaginous portions of the hip that cannot be seen on plain radiographs. Furthermore, US enables dynamic study of the hip with stress maneuvering. Practically speaking, the examination can often be successfully performed after 6 months of age (even up to 10-12 months) depending on the degree of ossification of the capital femoral epiphysis. An attempt at US examination is suggested, to limit the neonates exposure to ionizing radiation. If unsuccessful, plain films can follow. [15, 16, 17, 18, 19, 20, 21, 22]
The main ultrasonographic techniques for DDH are the Graf technique, which uses angle measurements of bony and cartilaginous components of the acetabulum; the Harcke technique, which evaluates femoral head stability by using different scans; and the Morin-Terjesen technique, which is based on the calculation of the percentage of bone coverage of the femoral head. [3]
Plain radiographs are typically obtained in the frontal pelvis, with the legs in the neutral position. If the hips are displaced or dysplastic, a second view may be obtained, with the hips in flexion and external rotation (ie, the frog-leg position) to look for reduction. The gonads of male patients should be shielded whenever possible. [23, 24, 25, 26, 27, 28]
The capital femoral epiphyses begin to ossify when an infant is aged 2-8 months. As the size of the ossification centers enlarge, shadowing may obscure the deeper acetabulum and limit US examination. Plain radiography then becomes the preferred modality for evaluating the hip.
Dynamic US examination is operator-dependent, and it requires training and experience for confident evaluation of the infant hip. Also, because US is highly sensitive in hip imaging, minor abnormalities or normal early laxities may be revealed. This is especially true of static imaging alone. Some abnormalities detected by US may not be clinically significant, but they may be mistakenly overdiagnosed and overtreated.
(See the images below.)
 Frontal radiograph of the pelvis. The ossification centers of the capital femoral epiphyses are symmetric and located in the joint spaces. Both heads project in the inner lower quadrants formed by the intersection of the Hilgenreiner (H) and Perkin (P) lines. Shenton lines (S) are continuous and demarcated by the dashed lines. The acetabular angles are symmetric and less than 28° bilaterally.
Frontal radiograph of the pelvis. The ossification centers of the capital femoral epiphyses are symmetric and located in the joint spaces. Both heads project in the inner lower quadrants formed by the intersection of the Hilgenreiner (H) and Perkin (P) lines. Shenton lines (S) are continuous and demarcated by the dashed lines. The acetabular angles are symmetric and less than 28° bilaterally.
 Frontal radiograph of the pelvis obtained in an infant before ossification of the capital femoral epiphyses begins. The legs are in the neutral position. The projected location of the unossified femoral heads must be estimated. The right hip is normal. The probable location of the left femoral head projects beyond the joint space and into the lower outer quadrant formed by the intersection of the Hilgenreiner and Perkin lines.
Frontal radiograph of the pelvis obtained in an infant before ossification of the capital femoral epiphyses begins. The legs are in the neutral position. The projected location of the unossified femoral heads must be estimated. The right hip is normal. The probable location of the left femoral head projects beyond the joint space and into the lower outer quadrant formed by the intersection of the Hilgenreiner and Perkin lines.
 Frontal radiograph of the pelvis in a 1-year-old child with a dislocated right hip. The degree of ossification of the femoral head on the dislocated side is decreased compared with that of the normally located left hip. The abnormally located hip articulates with a false neoacetabulum.
Frontal radiograph of the pelvis in a 1-year-old child with a dislocated right hip. The degree of ossification of the femoral head on the dislocated side is decreased compared with that of the normally located left hip. The abnormally located hip articulates with a false neoacetabulum.
Using expected-value decision analysis, Mahan et al, of Children's Hospital in Boston, found that the screening strategy associated with the highest probability of having a nonarthritic hip at the age of 60 years was to screen all neonates for hip dysplasia with a physical examination and to use ultrasonography selectively for infants who are at high risk. The expected value of a favorable hip outcome was 0.9590 for the strategy of screening all neonates with physical examination and selective use of ultrasonography, 0.9586 for screening all neonates with physical examination and ultrasonography, and 0.9578 for no screening. [29]
Intervention
Arthrography can be performed to assess the dislocated hip; often, it is performed at the time of surgical reduction, particularly if the reduction appears to be difficult to maintain. The indications for arthrography are fewer with the development of better sonography, the advent of magnetic resonance imaging (MRI), and the availability to confirm reductions in spica casts with computed tomography (CT) scanning. [30, 31]
The initial treatment for DDH involves the use of a brace that maintains the hip in flexion and abduction. The brace is worn until the clinical and radiologic examination findings are normal. Children older than 6 months usually are too large to tolerate a brace. Closed reduction under general anesthesia is usually attempted first. The reduction can be evaluated with MRI or an arthrogram and a postreduction CT scan.
Radiography
Plain radiographs of the pelvis are most helpful when significant ossification of the capital femoral epiphyses has occurred and when adequate ultrasound evaluation cannot be performed. Plain radiographs of the pelvis are obtained in the frontal projection with the legs in the neutral position. Before the femoral heads begin to ossify, the projected locations must be estimated.
Line measurements made on the anteroposterior radiograph help determine the relationship of the femoral head with the acetabulum. (See the image below.)
 Frontal radiograph of the pelvis. The ossification centers of the capital femoral epiphyses are symmetric and located in the joint spaces. Both heads project in the inner lower quadrants formed by the intersection of the Hilgenreiner (H) and Perkin (P) lines. Shenton lines (S) are continuous and demarcated by the dashed lines. The acetabular angles are symmetric and less than 28° bilaterally.
Frontal radiograph of the pelvis. The ossification centers of the capital femoral epiphyses are symmetric and located in the joint spaces. Both heads project in the inner lower quadrants formed by the intersection of the Hilgenreiner (H) and Perkin (P) lines. Shenton lines (S) are continuous and demarcated by the dashed lines. The acetabular angles are symmetric and less than 28° bilaterally.
The acetabular angle is determined by first drawing the Hilgenreiner (or Y-Y) line, which is a horizontal line between the 2 triradiate or Y-Y cartilages, and then drawing a second line connecting the superolateral and inferomedial margins of the acetabular roof, as Kirks and Griscom reported. [24] The normal acetabular angle is approximately 28° at birth. The angle decreases gradually with age as a result of modeling of the acetabulum by the femoral head and of the maturation of developing bone along the superolateral acetabular roof. The acetabular angle is often increased in DDH because maturation and ossification of the acetabulum are abnormal and delayed.
The Perkins line is drawn at the outer acetabular margin and is perpendicular to the Hilgenreiner line. These lines divide the hip into quadrants. The unossified femoral head normally is centered in the inferomedial quadrant. (See the image below.)
 Frontal radiograph of the pelvis obtained in an infant before ossification of the capital femoral epiphyses begins. The legs are in the neutral position. The projected location of the unossified femoral heads must be estimated. The right hip is normal. The probable location of the left femoral head projects beyond the joint space and into the lower outer quadrant formed by the intersection of the Hilgenreiner and Perkin lines.
Frontal radiograph of the pelvis obtained in an infant before ossification of the capital femoral epiphyses begins. The legs are in the neutral position. The projected location of the unossified femoral heads must be estimated. The right hip is normal. The probable location of the left femoral head projects beyond the joint space and into the lower outer quadrant formed by the intersection of the Hilgenreiner and Perkin lines.
In the normal hip, the Shenton line is a smooth, unbroken arc that bridges the medial femoral metaphysis and the inferior edge of the superior pubic ramus. Displacement of the femoral head out of the joint space and disruption of the Shenton line are suggestive of DDH.
Delayed ossification of the femoral epiphysis is observed in the unstable hip. A false acetabulum eventually develops secondary to molding of the displaced ossification center against the bony pelvis. (See the image below.)
 Frontal radiograph of the pelvis in a 1-year-old child with a dislocated right hip. The degree of ossification of the femoral head on the dislocated side is decreased compared with that of the normally located left hip. The abnormally located hip articulates with a false neoacetabulum.
Frontal radiograph of the pelvis in a 1-year-old child with a dislocated right hip. The degree of ossification of the femoral head on the dislocated side is decreased compared with that of the normally located left hip. The abnormally located hip articulates with a false neoacetabulum.
To assess reducibility, a frontal view of the pelvis can be obtained with the legs in external rotation (ie, frog-leg position). (See the image below.)
 Frontal radiograph of the pelvis obtained with the legs in the frog-leg position indicates that the plane of the femoral projection is toward the triradiate cartilage, suggesting that the hips are reducible.
Frontal radiograph of the pelvis obtained with the legs in the frog-leg position indicates that the plane of the femoral projection is toward the triradiate cartilage, suggesting that the hips are reducible.
Plain radiography has a low sensitivity, exposes the infant to ionizing radiation, and does not provide dynamic information. Radiographs are difficult to interpret before the capital femoral epiphyses ossify. Because some hips may be subluxatable but not frankly dislocated or dislocatable only with Barlow maneuvers, plain radiographs obtained in neonates or infants with their hips in the neutral position frequently fail to depict DDH.
CT and MRI
Computed tomography (CT) is useful for evaluating complicated dislocations and for postoperative evaluation of the hip. CT can depict osseous blocks to relocation, as well as iliopsoas tendon capsule constriction, a thick ligamentum teres, and fibrofatty pulvinar hypertrophy. CT can also be used to evaluate femoral and acetabular anteversion. [25, 32]
In infants with spica casts, low-milliamperage selective thin-section CT sections can confidently and quickly assess concentric reduction before the patient is discharged.
MRI can be useful in the preoperative and postoperative evaluation of a hip with many complications. MRI can be used to distinguish the labrum, capsule, and acetabular cartilage. MRI is useful for detecting the complications of DDH and treatment for DDH, such as avascular necrosis of the femoral head and joint effusions. MRI can also be used to demonstrate iliopsoas tendon compression, a thick ligamentum teres, and pulvinar hypertrophy. [25, 32, 33]
Ultrasonography
American College of Radiology (ACR) standard US examination of the infant hip is performed in 2 planes: the coronal and transverse. [34, 35] (See the images below.)
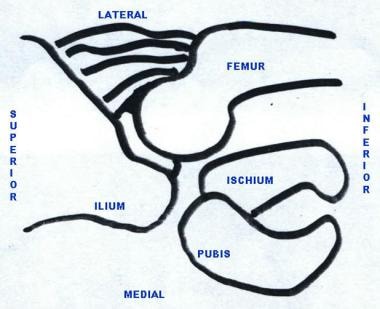 Schematic drawing of the coronal plane used to assess the hip at ultrasonography. The transducer is placed on the lateral aspect of the thigh.
Schematic drawing of the coronal plane used to assess the hip at ultrasonography. The transducer is placed on the lateral aspect of the thigh.
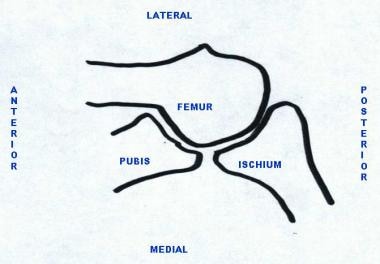 Schematic drawing of the transverse plane of the left hip. The anteroposterior orientation depends on whether the right or left hip is being examined. The transducer is placed in the transverse orientation over the anterior upper thigh.
Schematic drawing of the transverse plane of the left hip. The anteroposterior orientation depends on whether the right or left hip is being examined. The transducer is placed in the transverse orientation over the anterior upper thigh.
A high-resolution linear array transducer must be used. The infant may be examined in the supine or lateral decubitus position, with the hip in a 90º flexed position. The operator uses one hand to hold the infant's knee at a right angle to the thigh. The palm of an open hand may be placed on the small of the infant's back. The thigh is held in the neutral position for imaging.
The unossified cartilaginous femoral head appears as a speckled ball in the acetabular fossa. Once ossification begins, it appears as a central area of increased echogenicity in the center of the cartilaginous head.
The femoral head should be centered in the joint space, with half or more of the femoral head medial to the baseline in the coronal plane. The extent of maturity of the acetabulum can also be quantified by using angular measurements (see the image below). The ACR considers the calculation of these measurements optional. The standard coronal sectioning plane must be used at the deepest portion of the acetabulum, where the ilium appears as a straight line, perpendicular to the femoral head and parallel to the surface of the transducer.
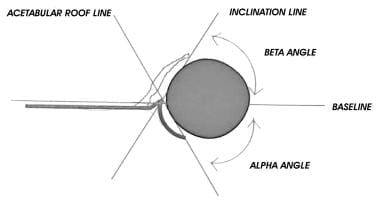 Calculation of the alpha and beta angles to assess acetabular maturity. A standard coronal image is used.
Calculation of the alpha and beta angles to assess acetabular maturity. A standard coronal image is used.
Acetabular maturity
To quantify acetabular maturity, alpha and beta angles are determined by the application of 3 lines drawn in the standard coronal plane (see the image below). The baseline passes through the plane of the ilium, where it connects to the osseous acetabular convexity. The inclination line passes from the lateral end of the acetabulum to the labrum, parallel to the cartilaginous roof. The roofline passes along the plane of the bony acetabular convexity.
 Real-time coronal sonogram of the hip shows calculation of the acetabular alpha angle. An angle of 60° or greater indicates acetabular maturity.
Real-time coronal sonogram of the hip shows calculation of the acetabular alpha angle. An angle of 60° or greater indicates acetabular maturity.
The alpha angle is used most commonly as a measurement of acetabular concavity, and it is calculated as the angle between the baseline and the roofline. A normal alpha angle is 60º or greater. Angles of 50-60º may be physiologically typical in the immediate neonatal period, but hips with these angles are considered immature and require clinical and US follow-up. Angles of less than 50º are always considered abnormal and require treatment.
The beta angle is measured between the baseline and the inclination line. It indicates the acetabular cartilaginous roof coverage. An angle of less than 55º is considered normal. The smaller the angle, the less the cartilaginous coverage and the better the bony acetabular coverage of the femoral head.
Not all dynamic hip imagers use these angles for the diagnosis and care of babies with DDH. Many use descriptive terms instead of numbers.
In a complementary method of assessing acetabular development, the distance between the medial aspect of the femoral head and the baseline (d) is compared with the maximum diameter of the femoral head (D); this d/D ratio is expressed as a percentage. This ratio represents the coverage of the femoral head by the bony acetabulum in the standard coronal plane (see the image below). Coverage of 58% or greater is considered normal. The smaller the coverage, the greater the acetabular immaturity.
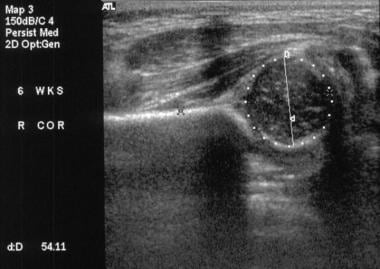 Real-time coronal sonogram of the hip with calculation of the d/D ratio. Coverage of 58% or greater is considered normal.
Real-time coronal sonogram of the hip with calculation of the d/D ratio. Coverage of 58% or greater is considered normal.
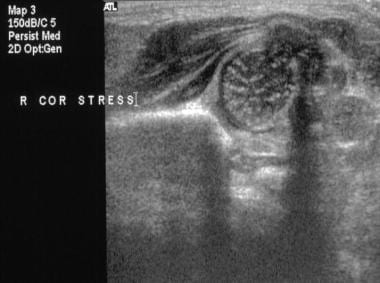
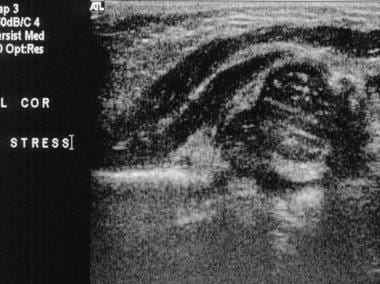
Stress maneuvering (ie, the Barlow maneuver) with the femur in 90º of flexion and maximum adduction is performed during transverse imaging to assess stability (see the first 2 images below). The use of stress is optional in coronal imaging, which may be performed with the patient's leg in a flexed or neutral position. Stress is omitted if the infant is receiving treatment for DDH with a Pavlik harness. Stress maneuvering reveals instability, subluxation (see the third image below), or dislocation (see the fourth image below). In dislocated hips, the Ortolani maneuver should be performed to check for reducibility.
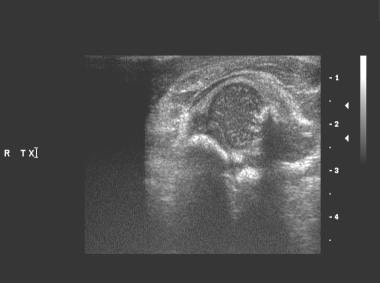 Real-time transverse sonogram of the right hip obtained without stress maneuvering reveals that the cartilaginous femoral head is well centered above the triradiate cartilage between the pubis and ischium. Echoes are present through the interface with the cartilage; this appearance has been likened to that of a lollipop, in which the femoral head is the "candy" and the echoes through the cartilage are the "stick." In a normally stable hip, this appearance should be maintained with stress maneuvering.
Real-time transverse sonogram of the right hip obtained without stress maneuvering reveals that the cartilaginous femoral head is well centered above the triradiate cartilage between the pubis and ischium. Echoes are present through the interface with the cartilage; this appearance has been likened to that of a lollipop, in which the femoral head is the "candy" and the echoes through the cartilage are the "stick." In a normally stable hip, this appearance should be maintained with stress maneuvering.
 Real-time sonogram of the right hip obtained with stress maneuvering reveals that the femoral head is posteriorly displaced over the ischium.
Real-time sonogram of the right hip obtained with stress maneuvering reveals that the femoral head is posteriorly displaced over the ischium.
 Coronal real-time sonogram of the hip obtained with stress maneuvering reveals significant lateral motion, which is not out of the plane of the baseline. This was accompanied by posterior motion in the transverse plane.
Coronal real-time sonogram of the hip obtained with stress maneuvering reveals significant lateral motion, which is not out of the plane of the baseline. This was accompanied by posterior motion in the transverse plane.
 Coronal real-time sonogram of the hip obtained with stress maneuvering reveals that the capital femoral epiphysis displaces out of the plane of the baseline. This dislocatable hip was reimaged after Ortolani maneuvering, and the dislocation was reducible.
Coronal real-time sonogram of the hip obtained with stress maneuvering reveals that the capital femoral epiphysis displaces out of the plane of the baseline. This dislocatable hip was reimaged after Ortolani maneuvering, and the dislocation was reducible.
An ancillary sign of instability is asymmetry in the degree of ossification of the femoral heads.
False positives/negatives
Mild instability may be observed in healthy neonates in their first few days of life, when the typical femoral head has a laxity of 3-4 mm on average. This amount of motion should resolve spontaneously within the first months of an infant's life, after maternal hormonal influences diminish. To increase reliability, guidelines have recommended that US studies be performed when infants are 4-6 weeks of age. [36, 35, 37, 38]
Inexperienced US examiners can mistake the greater trochanter cartilage for the femoral head and incorrectly diagnose developmental dysplasia of the hip (DDH).
It has been suggested that, because US is very sensitive, a plain radiograph be performed to confirm DDH in infants over the age of 4 months with abnormal static US examinations, as ossification of the capital femoral epiphyses would begin to be present, thereby limiting overtreatment. This unnecessary exposure to ionizing radiation, however, can be avoided by the performance of a dynamic US examination. [26, 27]
Guidelines Summary
A number of professional medical organizations have addressed both the clinical practice and imaging aspects of early detection of DDH. Evidence-based clinical practice guidelines have been published by the following organizations:
-
American Academy of Orthopaedic Surgeons (AAOS) [38]
Consensus imaging recommendations have been released by the following organizations:
Screening
Universal ultrasound screening for DDH in newborns is performed in some European countries. Universal screening increases DDH detection, which leads to higher rates of treatment with abduction splinting; however, there is no evidence that it reduces the time to diagnose DDH. This may lead to increased expense, unnecessary treatment, and increased posttreatment complications of AVN. For these reasons, neither the American Academy of Pediatrics (AAP) nor the American Academy of Orthopaedic Surgeons (AAOS) recommends universal screening. [37, 38]
Guidelines by the American Academy of Pediatrics for evaluation and referral of developmental dysplasia of the hip recognize the increased awareness that dislocations of the hip may develop after birth and during early childhood. The term “surveillance” is preferred over “screening,” because screening suggests a one-time process, while surveillance is performed with periodic clinical exams until walking age. Continued surveillance may be more likely to discover dislocations that develop after birth. [37]
Imaging is recommended when physical examination raises clinical suspicion of hip dysplasia. Additionally, risk factors for which the pediatrician may consider an imaging study in the child with a normal screening physical examination are as follows [37] :
-
Breech position in the third trimester [40]
-
Family history of DDH
-
History of improper swaddling
-
History of abnormal hip physical examination in the neonatal period, which subsequently normalizes.
Imaging before 6 weeks of age is discouraged because of the high rate of false positives or immature hips, which spontaneously resolve most often by age 6 weeks. The guidelines note that there is no proven benefit to ultrasound at 6 weeks versus radiographs at 4-6 months; imaging should be chosen based on local conditions and availability of experienced, trained pediatric hip sonographers. [37]
The American Academy of Orthopaedic Surgeons (AAOS) guidelines recommends imaging study before 6 months of age in infants with the following risk factors [38] :
-
Breech presentation
-
Family history
-
History of clinical instability
Ultrasound is recommended for infants younger than 6 weeks with a positive instability examination to guide the decision to initiate brace treatment. [38]
Periodic imaging assessments (ultrasound or radiograph based on age) should be performed during management for unstable infant hips. [38]
Performance of ultrasonography
American Institute of Ultrasound in Medicine (AIUM) guidelines include the following indications for ultrasound examination [36, 34] :
-
Abnormal or equivocal findings on physical or imaging examination of the hip
-
Any family history of DDH
-
Breech presentation regardless of sex
-
Neuromuscular conditions
-
Monitoring patients with DDH being treated with a Pavlik harness or other splint device.
The AIUM, considers oligohydramnios and other intrauterine causes of postural molding to be a relative indication for ultrasound screening. [34]
In addition, it is recommended that any female infant with a breech presentation at birth and a family history of DDH should undergo ultrasound screening. [36, 34]
There are no absolute contraindications to ultrasound of the infant hip for DDH, but the value of ultrasound diminishes as the femoral head ossifies; therefore, radiography is preferable for patients 6 months of age or older. [36, 34]
American College of Radiology
The American College of Radiology notes that 41-58% of abnormal findings from physical examinations are negative in US studies, thus confirming the value of US evaluation. They also note that for patients 4-6 months of age or older with clinical suspicion of DDH, anteroposterior (AP) radiograph of the pelvis is recommended. [35]
-
Frontal radiograph of the pelvis. The ossification centers of the capital femoral epiphyses are symmetric and located in the joint spaces. Both heads project in the inner lower quadrants formed by the intersection of the Hilgenreiner (H) and Perkin (P) lines. Shenton lines (S) are continuous and demarcated by the dashed lines. The acetabular angles are symmetric and less than 28° bilaterally.
-
Frontal radiograph of the pelvis obtained in an infant before ossification of the capital femoral epiphyses begins. The legs are in the neutral position. The projected location of the unossified femoral heads must be estimated. The right hip is normal. The probable location of the left femoral head projects beyond the joint space and into the lower outer quadrant formed by the intersection of the Hilgenreiner and Perkin lines.
-
Frontal radiograph of the pelvis in a 1-year-old child with a dislocated right hip. The degree of ossification of the femoral head on the dislocated side is decreased compared with that of the normally located left hip. The abnormally located hip articulates with a false neoacetabulum.
-
Frontal radiograph of the pelvis obtained with the legs in the frog-leg position indicates that the plane of the femoral projection is toward the triradiate cartilage, suggesting that the hips are reducible.
-
Schematic drawing of the coronal plane used to assess the hip at ultrasonography. The transducer is placed on the lateral aspect of the thigh.
-
Schematic drawing of the transverse plane of the left hip. The anteroposterior orientation depends on whether the right or left hip is being examined. The transducer is placed in the transverse orientation over the anterior upper thigh.
-
Calculation of the alpha and beta angles to assess acetabular maturity. A standard coronal image is used.
-
Real-time coronal sonogram of the hip shows calculation of the acetabular alpha angle. An angle of 60° or greater indicates acetabular maturity.
-
Real-time coronal sonogram of the hip with calculation of the d/D ratio. Coverage of 58% or greater is considered normal.
-
Real-time transverse sonogram of the right hip obtained without stress maneuvering reveals that the cartilaginous femoral head is well centered above the triradiate cartilage between the pubis and ischium. Echoes are present through the interface with the cartilage; this appearance has been likened to that of a lollipop, in which the femoral head is the "candy" and the echoes through the cartilage are the "stick." In a normally stable hip, this appearance should be maintained with stress maneuvering.
-
Real-time sonogram of the right hip obtained with stress maneuvering reveals that the femoral head is posteriorly displaced over the ischium.
-
Coronal real-time sonogram of the hip obtained with stress maneuvering reveals significant lateral motion, which is not out of the plane of the baseline. This was accompanied by posterior motion in the transverse plane.
-
Coronal real-time sonogram of the hip obtained with stress maneuvering reveals that the capital femoral epiphysis displaces out of the plane of the baseline. This dislocatable hip was reimaged after Ortolani maneuvering, and the dislocation was reducible.









