Practice Essentials
Dandy-Walker malformation (DWM) is a rare congenital malformation that involves the cerebellum and fourth ventricle. Dandy-Walker malformation and related variants have a prevalence of 1 in 35,000 live births in the United States. [1, 2, 3, 4] Dandy-Walker malformation is characterized by agenesis or hypoplasia of the cerebellar vermis, cystic dilatation of the fourth ventricle, and enlargement of the posterior fossa. A large number of concomitant problems may be present, but Dandy-Walker malformation is recognized whenever these 3 features are found. Approximately 70-90% of patients have hydrocephalus, which often develops postnatally. Dandy-Walker malformation may be associated with atresia of the foramen of Magendie and, possibly, the foramen of Luschka. [5, 6, 7, 8, 9]
(See the images of Dandy-Walker malformation below.)
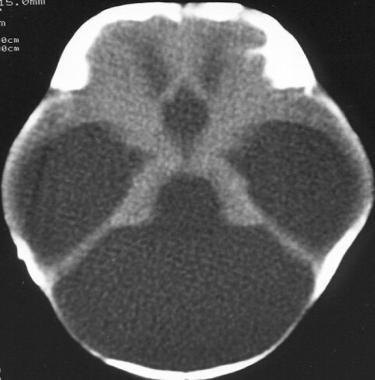
 Dandy-Walker malformation. An axial T2-weighted MRI scan that shows hydrocephalus, a large cerebrospinal fluid cyst in the posterior fossa, thinned occipital bone (arrows), and hypoplastic cerebellar hemispheres with a winged appearance (c).
Dandy-Walker malformation. An axial T2-weighted MRI scan that shows hydrocephalus, a large cerebrospinal fluid cyst in the posterior fossa, thinned occipital bone (arrows), and hypoplastic cerebellar hemispheres with a winged appearance (c).
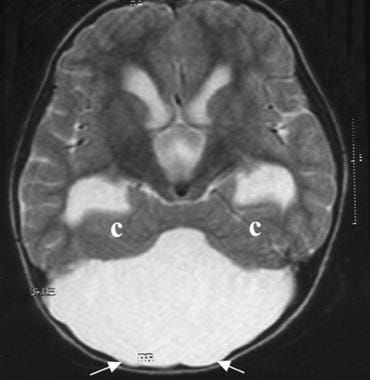
 Dandy-Walker malformation. An axial T1-weighted MRI scan showing ventriculomegaly and a superiorly displaced posterior fossa cyst.
Dandy-Walker malformation. An axial T1-weighted MRI scan showing ventriculomegaly and a superiorly displaced posterior fossa cyst.
Dandy-Walker complex
Classically, posterior fossa cystic malformations have been divided into Dandy-Walker malformation, Dandy-Walker variant, mega cisterna magna, and posterior fossa arachnoid cyst. Precisely differentiating the malformations may not be possible using imaging studies. Dandy-Walker malformation, variant, and mega cisterna magna are currently believed to represent a continuum of developmental anomalies on a spectrum that has been termed the Dandy-Walker complex. [10, 11, 12, 8]
Dandy-Walker complex is characterized by an enlarged posterior fossa; a high position of the tentorium, with upward displacement of the lateral sinuses; torcular herophili associated with varying degrees of vermian aplasia or hypoplasia; and a cystic dilatation of the fourth ventricle that nearly fills the entire posterior fossa. Since the vermis is present in posterior fossa arachnoid cyst, this is considered separately from Dandy-Walker malformation.
Dandy-Walker variant
Dandy-Walker variant (see the image below) consists of vermian hypoplasia and cystic dilatation of the fourth ventricle, without enlargement of the posterior fossa.
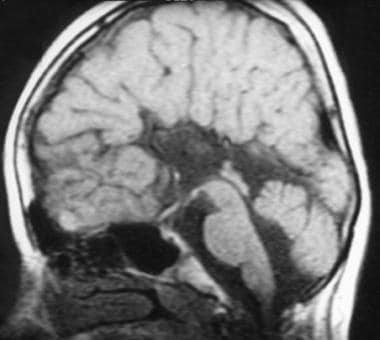 Dandy-Walker malformation. This sagittal T1-weighted MRI shows agenesis of the corpus callosum and a hypoplastic inferior vermis in a 13-year-old girl with thoracal scoliosis and Dandy-Walker variant. The fourth ventricle is slightly enlarged, but the posterior fossa typically is normal in size.
Dandy-Walker malformation. This sagittal T1-weighted MRI shows agenesis of the corpus callosum and a hypoplastic inferior vermis in a 13-year-old girl with thoracal scoliosis and Dandy-Walker variant. The fourth ventricle is slightly enlarged, but the posterior fossa typically is normal in size.
Mega cisterna magna
Mega cisterna magna (see the image below) consists of an enlarged posterior fossa secondary to an enlarged cisterna magna, with a normal cerebellar vermis and fourth ventricle. Ventriculomegaly occurs rarely (2.3%) before or after birth. [13]
 Dandy-Walker malformation. This sagittal T1-weighted MRI shows a large retrocerebellar cerebrospinal fluid collection and a normal fourth ventricle and vermis in a patient with mega cisterna magna in Dandy-Walker malformation.
Dandy-Walker malformation. This sagittal T1-weighted MRI shows a large retrocerebellar cerebrospinal fluid collection and a normal fourth ventricle and vermis in a patient with mega cisterna magna in Dandy-Walker malformation.
Arachnoid cyst
Retrocerebellar arachnoid cysts of developmental origin (see the image below) are uncommon but clinically important. True retrocerebellar arachnoid cysts displace the fourth ventricle and cerebellum anteriorly and show significant mass effect. Because there are different surgical therapy approaches for posterior fossa arachnoid cyst and Dandy-Walker malformation, it is essential to differentiate between the 2 entities. [14]
 Dandy-Walker malformation. A posterior fossa arachnoid cyst in a 15-month-old girl with a lumbar pilonidal sinus. The sagittal T1-weighted MRI shows a large posterior fossa cyst that is compressing the cerebellar hemispheres, vermis, fourth ventricle (arrow), and brainstem.
Dandy-Walker malformation. A posterior fossa arachnoid cyst in a 15-month-old girl with a lumbar pilonidal sinus. The sagittal T1-weighted MRI shows a large posterior fossa cyst that is compressing the cerebellar hemispheres, vermis, fourth ventricle (arrow), and brainstem.
Blake pouch cyst
The Blake pouch cyst (Blake pouch remnant or persistent Blake pouch) is another posterior fossa embryologic anomaly that must be included in the differential diagnoses of Dandy-Walker malformation. This anomaly can cause obstructive hydrocephalus, which requires early surgical intervention. [15] A retrospective analysis of fetal MRIs with posterior fossa malformations found that Dandy-Walker malformation could be differentiated from Blake pouch cyst by a significantly higher tegmentovermian angle (TVA) at any gestational age. Other biomarkers such as anterior-to-posterior and craniocaudal vermes were not significantly different until 23.1 weeks' gestation or later. [16]
Clinical presentation
Most definitions of Dandy-Walker malformation have included dysgenesis of the vermis, cystic dilatation of the fourth ventricle, and enlargement of the posterior fossa with elevation of the tentorium/torcula.
Dandy-Walker malformation consists of a malformation of the roof of the fourth ventricle and of the cerebellum. The cerebellum is poorly developed and is displaced upward and laterally.
The enlarged fourth ventricle balloons out backward. The fourth ventricle is grossly misshapen because it is a membrane-wrapped cyst that extends into the foramen magnum. The membrane-wrapped cyst may lift and displace the posterior portion of the brain, as well as cause an internal obstruction of normal CSF flow, with resultant hydrocephalus.
Dandy-Walker malformation may be associated with atresia of the foramen of Magendie and, possibly, the foramen of Luschka. [17]
Common findings of Dandy-Walker malformation include the following:
-
Enlarged posterior fossa
-
Varying degrees of cerebellar and vermian hypoplasia or complete vermian absence
-
Cyst formation in the posterior fossa
-
Vermian remnant everted above the posterior fossa cyst
-
Hypoplastic cerebellar hemispheres winged anterolaterally (outward) in front of the cyst
-
Absence of the foramina of Luschka and Magendie
-
Obstructive hydrocephalus secondary to cystic dilatation of the fourth ventricle (70-90%)
-
Abnormally high position of the straight sinus, torcular herophili, and tentorium
-
Sinus confluence and lateral sinuses elevated above the lambdoid sutures (high tentorial insertion, also called lambdoid-torcular inversion)
-
Aqueductal obstruction, which may affect the need for supratentorial decompression (and is, therefore, an important component)
-
If callosal agenesis coexists (20-25%), development of dilatation of the occipital horns (colpocephaly)
-
Possible brainstem compression and hypoplasia; the degree of pontine hypoplasia is directly related to the degree of cerebellar hypoplasia [18]
-
Thinning and bulging of the occipital bones
Associated central nervous system (CNS) abnormalities of Dandy-Walker malformation are reported in 70% of children and include the following:
-
Dysgenesis of the corpus callosum (20-25%) [7]
-
Lipoma of the corpus callosum
-
Holoprosencephaly (25%)
-
Porencephaly
-
Dysplasia of the cingulate gyrus (25%)
-
Polymicrogyria/gray matter heterotopia (5-10%)
-
Cerebellar heterotopia
-
Occipital encephalocele (7%) [7]
-
Microcephaly
-
Dermoid cysts
-
Malformation of the cerebellar folia (25%)
-
Malformation of the inferior olivary nucleus
-
Hamartoma of the tuber cinereum
-
Lumbosacral meningoceles
-
Spinal lipoma
Non-CNS-associated malformations are reported in 20-33% of children and include the following:
-
Orofacial deformities and cleft palate (6%)
-
Cardiac anomalies [21]
-
Urinary tract abnormalities (polycystic kidneys) [22]
-
Cataracts, retinal dysgenesis, and choroid coloboma
-
Facial hemangioma
-
Hypertelorism
-
Meckel-Gruber syndrome [5]
Imaging modalities
Dandy-Walker malformation is best diagnosed with the help of ultrasonography (US) and magnetic resonance imaging (MRI). US may be the initial examination performed because it can be done portably and without sedation, as well as allowing multiplanar imaging. [24, 25, 26, 27] US, however, is limited because it is heavily operator-dependent. Abnormalities such as the gyral, dural, tentorial, and skull anomalies that accompany Dandy-Walker malformations are not clearly depicted by US.
Measurement of the cisterna magna forms part of the ultrasound evaluation of the fetal brain. A prominent cisterna magna shown on prenatal ultrasound may raise the concern for congenital posterior fossa abnormalities. [1, 28, 29]
The introduction of modern imaging techniques, specifically MRI, has radically changed the evaluation of symptoms related to the posterior fossa. MRI is usually performed for detailed evaluation of Dandy-Walker malformation lesions and complications after the diagnosis is suspected using computed tomography (CT) and US. Distinguishing milder forms of vermian hypoplasia from a mega cisterna magna or an arachnoid cyst on US is difficult in the third trimester, where ossification of the skull can limit sonographic assessment of the posterior fossa structures. With its multiplanar capabilities, fetal MR imaging can better evaluate the morphology of the vermis, as well as the anatomic relationship between a retrocerebellar cyst and the fourth ventricle, which can help differentiate a Dandy-Walker variant from other entities, such as a mega cisterna magna. [30]
MRI allows surgeons to accurately view the cerebellum and associated structures, determine which form the malformation has taken, and gauge the progress of the malformation. MRI also demonstrates which space should be shunted first. MRI has been frequently used for diagnosing fetal craniospinal anomalies.
Since it can distinguish between hydrocephalus associated with Dandy-Walker and hydrocephalus associated with other etiologies, CT scanning is also useful in Dandy-Walker malformation; however, it exposes the infant to ionizing radiation. Clearly distinguishing the subtypes of Dandy-Walker complex on axial CT images is difficult. In addition, evaluating subtle supratentorial pathologies and associated abnormalities on CT scans may not be easy because its routine use is constrained by the axial plane.
The classic abnormal findings of Dandy-Walker malformation described on cranial CT and MRI can also be demonstrated on cranial sonography. US is routinely used during the antenatal period as a screening method, and it is particularly used for postnatal follow-up studies of hydrocephalus. US evaluation of posterior fossa cystic abnormalities in the newborn is best accomplished via a posterolateral fontanelle approach or through the cisterna magna posteriorly.
According to a retrospective MRI study by Whitehead et al of cerebellar development prenatally and postnatally, the Dandy-Walker malformation phenotype is best defined by inferior predominant vermian hypoplasia, an enlarged tegmentovermian angle, inferolateral displacement of the tela choroidea/choroid plexus, an obtuse fastigial recess, and an unpaired caudal lobule. [31]
Measurement of the brainstem-vermian (BV) angle and the brainstem-tentorium (BT) angle helps determine increased size of the cisterna magna. The BV angle increases with severity (ie, angles below 18 degrees are considered normal, angles 18 to 30 degrees suggest Blake pouch malformation, and angles greater than 45 degrees are strongly suggestive of dandy-walker malformation). [1, 29]
Plain radiography has been primarily used in the evaluation of shunt malfunction, as well as for diagnosing associated anomalies.
Salihu et al studied infant mortality in non-Hispanic black and non-Hispanic white neonates with Dandy-Walker syndrome and found that Dandy-Walker syndrome has one of the largest Black-White disparities in postneonatal survival. Neonatal mortality was similar for non-Hispanic Blacks and non-Hispanic Whites, but non-Hispanic Blacks had an 8-fold increased risk for postneonatal mortality. [32]
In another study by Salihu and co-workers, infants with Dandy-Walker syndrome and 2 or more affected organ systems were approximately 6 times as likely to die postneonatally as were patients with isolated Dandy-Walker syndrome. According to the authors, these findings confirm the widely held belief that Dandy-Walker syndrome is a heterogeneous, rather than a homogeneous, disorder. [33]
Radiography
Plain radiographs have diagnostic importance in imaging bony abnormalities and in the evaluation of ventriculoperitoneal shunt malfunction. On conventional radiographs, the posterior fossa is disproportionately enlarged, with characteristic thinning and bulging of the occiput. Increased pressure from the massively dilated fourth ventricle, along with prominent CSF pulsations through the cyst fluid, causes widening of the diastatic lambdoid sutures and erosive scalloping of the occiput. Torcular herophili and lateral sinus grooves are located high above the lambdoid angle (torcular-lambdoid angle inversion). [11]
Computed Tomography
CT is used to diagnose Dandy-Walker malformation and to follow ventricular shunt function in shunted patients. Nonenhanced CT examination successfully delineates multiple components of Dandy-Walker malformation, which includes partial or complete absence of the cerebellar vermis; posterior fossa cyst contiguous with the fourth ventricle; small and widely separated cerebellar hemispheres; anterior and lateral displacement of hypoplastic cerebellar hemispheres; anterior displacement of pons; elevated imprint of the transverse sinuses, with thinning and bulging of the bones of the posterior fossa; scalloping of petrous pyramids; and hydrocephalus.
Three-dimensional (3D) CT and CT angiography studies can be used to evaluate osseous malformation and the relationships between vascular and bony structures. For these studies, 1-mm thickness, an axial plane, and 3D reconstruction are used.
CT scans can depict the malformation relatively well, but a slice may miss the relevant presence of the vermis. Clearly distinguishing Dandy-Walker complex subtypes using axial CT images is difficult. [34]
(See the CT images of Dandy-Walker malformation below.)
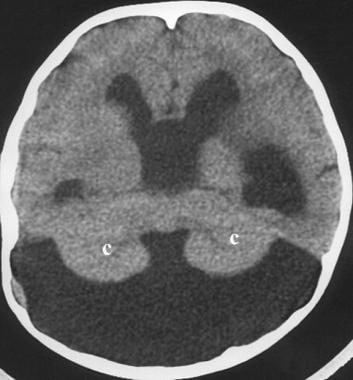 Dandy-Walker malformation. An axial computed tomography (CT) scan in a 7-year-old girl with hydrocephalus showing a large cerebrospinal fluid cyst in the posterior fossa and hypoplastic cerebellar hemispheres with a winged appearance (c).
Dandy-Walker malformation. An axial computed tomography (CT) scan in a 7-year-old girl with hydrocephalus showing a large cerebrospinal fluid cyst in the posterior fossa and hypoplastic cerebellar hemispheres with a winged appearance (c).
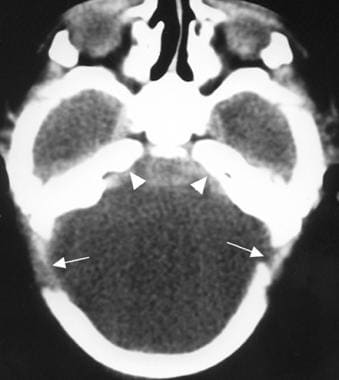 Dandy-Walker malformation. An axial CT scan in a 1-day-old boy that shows a large posterior fossa cyst, separation of the lambdoid sutures (large arrows), and concavity of the petrous ridges (small arrows).
Dandy-Walker malformation. An axial CT scan in a 1-day-old boy that shows a large posterior fossa cyst, separation of the lambdoid sutures (large arrows), and concavity of the petrous ridges (small arrows).
 Dandy-Walker malformation. Joubert syndrome in an 8-month-old boy. The axial CT scan obtained near the pontomesencephalic junction shows a batwing configuration of the fourth ventricle and unusual definition of the superior cerebellar peduncles at this level (arrows). The vermis is dysgenetic, and the 2 cerebellar hemispheres appose each other in the midline.
Dandy-Walker malformation. Joubert syndrome in an 8-month-old boy. The axial CT scan obtained near the pontomesencephalic junction shows a batwing configuration of the fourth ventricle and unusual definition of the superior cerebellar peduncles at this level (arrows). The vermis is dysgenetic, and the 2 cerebellar hemispheres appose each other in the midline.
Magnetic Resonance Imaging
Malformations of the CNS are best delineated using MRI. The diagnosis is straightforward when typical MRI findings are present. MRI is usually required for better anatomic resolution prior to surgical intervention. [25, 35, 36]
(See the MRI images of Dandy-Walker malformation below.)
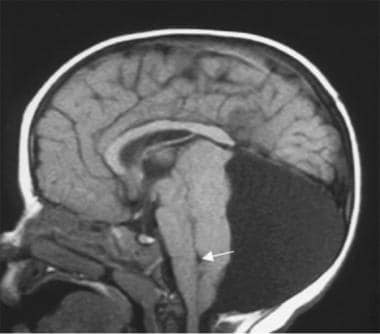
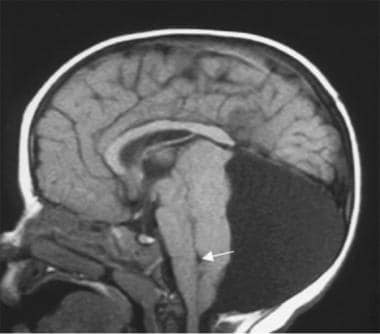
 Dandy-Walker malformation. A sagittal T1-weighted magnetic resonance imaging (MRI) scan in a 5-year-old girl (also see the following 2 images) shows a large posterior fossa cyst elevating the torcular herophili and sinus rectus (short arrow). The hypoplastic vermis is everted over the posterior fossa cyst (long arrow). The cerebellar hemispheres and brainstem (b) are hypoplastic. Thinned occipital squama is seen (arrowheads).
Dandy-Walker malformation. A sagittal T1-weighted magnetic resonance imaging (MRI) scan in a 5-year-old girl (also see the following 2 images) shows a large posterior fossa cyst elevating the torcular herophili and sinus rectus (short arrow). The hypoplastic vermis is everted over the posterior fossa cyst (long arrow). The cerebellar hemispheres and brainstem (b) are hypoplastic. Thinned occipital squama is seen (arrowheads).
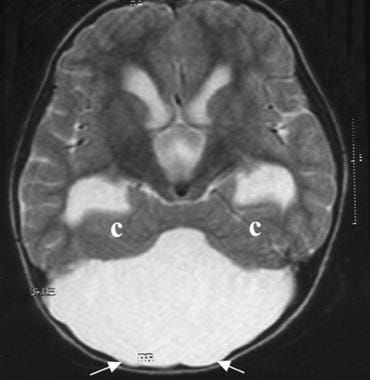 Dandy-Walker malformation. An axial T2-weighted MRI scan that shows hydrocephalus, a large cerebrospinal fluid cyst in the posterior fossa, thinned occipital bone (arrows), and hypoplastic cerebellar hemispheres with a winged appearance (c).
Dandy-Walker malformation. An axial T2-weighted MRI scan that shows hydrocephalus, a large cerebrospinal fluid cyst in the posterior fossa, thinned occipital bone (arrows), and hypoplastic cerebellar hemispheres with a winged appearance (c).
 Dandy-Walker malformation. An axial T1-weighted MRI scan showing ventriculomegaly and a superiorly displaced posterior fossa cyst.
Dandy-Walker malformation. An axial T1-weighted MRI scan showing ventriculomegaly and a superiorly displaced posterior fossa cyst.
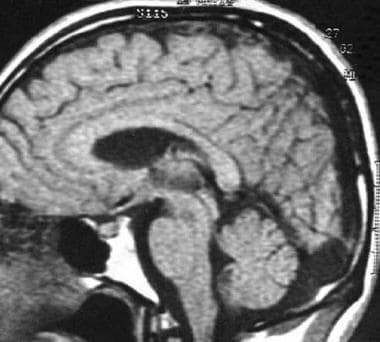
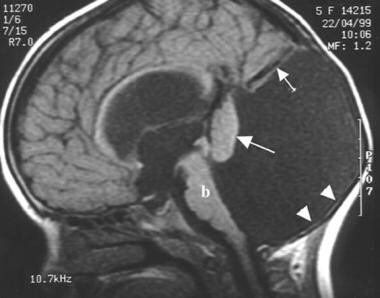
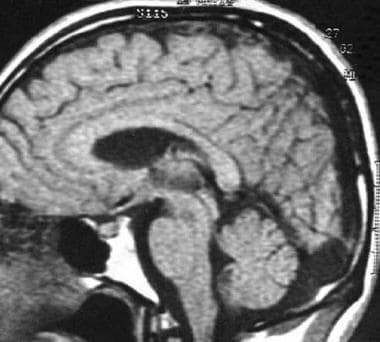
 Dandy-Walker malformation. This sagittal T1-weighted MRI scan in an 11-day-old boy (also see the following image) shows agenesis of the corpus callosum, a hypoplastic brainstem (b), elevation of the torcular herophili (lambdoid-torcular inversion, large arrow), a large fourth ventricle, and a markedly hypoplastic vermis that is rotated superiorly (small arrow).
Dandy-Walker malformation. This sagittal T1-weighted MRI scan in an 11-day-old boy (also see the following image) shows agenesis of the corpus callosum, a hypoplastic brainstem (b), elevation of the torcular herophili (lambdoid-torcular inversion, large arrow), a large fourth ventricle, and a markedly hypoplastic vermis that is rotated superiorly (small arrow).
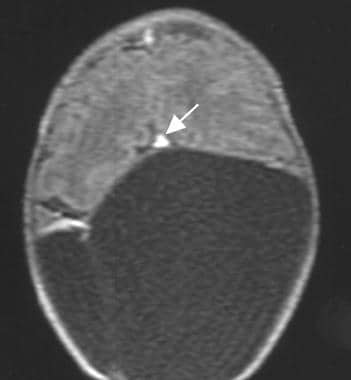 Dandy-Walker malformation. An axial T1-weighted MRI showing an elevated, anteriorly displaced torcular herophili (arrow) and a superiorly displaced posterior fossa cyst.
Dandy-Walker malformation. An axial T1-weighted MRI showing an elevated, anteriorly displaced torcular herophili (arrow) and a superiorly displaced posterior fossa cyst.
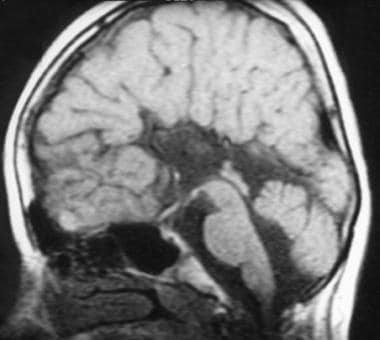 Dandy-Walker malformation. This sagittal T1-weighted MRI shows agenesis of the corpus callosum and a hypoplastic inferior vermis in a 13-year-old girl with thoracal scoliosis and Dandy-Walker variant. The fourth ventricle is slightly enlarged, but the posterior fossa typically is normal in size.
Dandy-Walker malformation. This sagittal T1-weighted MRI shows agenesis of the corpus callosum and a hypoplastic inferior vermis in a 13-year-old girl with thoracal scoliosis and Dandy-Walker variant. The fourth ventricle is slightly enlarged, but the posterior fossa typically is normal in size.
 Dandy-Walker malformation. This sagittal T1-weighted MRI shows a large retrocerebellar cerebrospinal fluid collection and a normal fourth ventricle and vermis in a patient with mega cisterna magna in Dandy-Walker malformation.
Dandy-Walker malformation. This sagittal T1-weighted MRI shows a large retrocerebellar cerebrospinal fluid collection and a normal fourth ventricle and vermis in a patient with mega cisterna magna in Dandy-Walker malformation.
 Dandy-Walker malformation. A posterior fossa arachnoid cyst in a 15-month-old girl with a lumbar pilonidal sinus. The sagittal T1-weighted MRI shows a large posterior fossa cyst that is compressing the cerebellar hemispheres, vermis, fourth ventricle (arrow), and brainstem.
Dandy-Walker malformation. A posterior fossa arachnoid cyst in a 15-month-old girl with a lumbar pilonidal sinus. The sagittal T1-weighted MRI shows a large posterior fossa cyst that is compressing the cerebellar hemispheres, vermis, fourth ventricle (arrow), and brainstem.
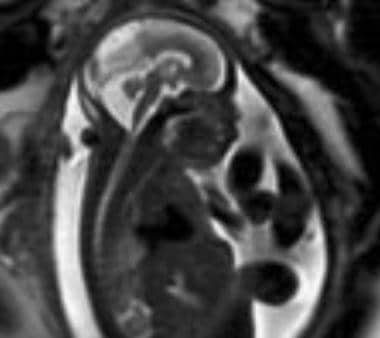 Dandy-Walker malformation. An antenatal MRI showing Dandy-Walker malformation in a fetus. Courtesy of Umit Aksoy, MD, Uludag University, Bursa, Turkey.
Dandy-Walker malformation. An antenatal MRI showing Dandy-Walker malformation in a fetus. Courtesy of Umit Aksoy, MD, Uludag University, Bursa, Turkey.
Nonenhanced routine cranial MRI can image the altered anatomy and provide excellent images in all projections (sagittal, axial, coronal), of which the sagittal view is one of the most useful.
Hypoplasia or absence of the cerebellar vermis is best detected using thin-sectioned midline sagittal T1-weighted images. Wide separation of the cerebellar hemispheres without intervening vermis can be seen in axial or coronal images. In some patients, the inferior lobules of the vermis appear to be hypoplastic, while in others, they appear to be intact. Remnants of the dysplastic upper vermis are rotated anterosuperiorly, compressed, and attached to the tentorium. Axial images alone may be misleading in revealing the upwardly rotated vermis.
An enlarged posterior fossa, cyst formation in the posterior fossa, anterolaterally winged cerebellar hemispheres (winged outward), absence of falx cerebelli, and scalloping of petrous pyramids are well-demonstrated on T1-weighted images.
Sagittal MRI can help evaluate an abnormally high position of the straight sinus, torcular herophili, tentorium, high tentorial insertion (lambdoid-torcular inversion), hypoplastic and compressed brainstem, and obstructive hydrocephalus secondary to cystic dilatation of the fourth ventricle in patients with Dandy-Walker malformation. [18]
CSF flow and cine MRI techniques are valuable imaging methods for demonstrating patency of the CSF pathways at the level of the incisura or aqueduct of Sylvius. Shunting of the cyst alone in the presence of aqueductal obstruction may result in downward transincisural herniation of the cerebrum and atria of the lateral ventricles; however, shunting of the lateral ventricles alone when the aqueduct is obstructed may lead to an upward herniation of the posterior fossa cyst, resulting in a characteristic "snowman" appearance in the sagittal plane in the absence of communication. The hydrocephalus in patients with Dandy-Walker malformation is frequently communicating in type with patency of the aqueduct. [37]
Assessing the presence of associated supratentorial anomalies is important, since the prognosis for patients is much better in the absence of the anomalies. MRI affords an accurate, objective, and detailed identification of supratentorial anomalies.
MRI and US have been used as diagnostic tools in the antenatal period. Fetal MRI at younger gestational age (such as < 20 wk) may have a reduced specificity. This may be related to small size, fetal motion, volume averaging, and difficulty in obtaining a true mid-sagittal image. Follow-up MR imaging, either at a later gestational age or postnatally, is recommended. [30]
Use of a novel 3D MRI technique to image the fetal posterior fossa has been reported. In a comparison of standard 2D MRI images to 3D reconstructed MRI images, lengths of the transcerebellar diameter measured within a 3D reconstruction were more concordant between imaging planes, as they correct for fetal motion and orthogonal slice acquisition. [38]
A systematic review of 217 fetuses diagnosed with Dandy-Walker malformation found that the prenatal diagnosis was not confirmed after birth in 28.2% (95% CI, 8.5-53.9%) of cases. [39]
In a study by Akiyama et al, volumetric analysis of fetal MRI showed that regardless of heterogeneous etiologies, fetuses with Dandy-Walker malformation had a larger cortical plate volume than control fetuses. In addition, after excluding fetuses with agenesis of the corpus callosum (ACC), fetuses with Dandy-Walker malformation were shown to have larger subcortical parenchyma, whole cerebrum, and cerebellar hemispheres than control fetuses. [40]
Ultrasonography
Classic abnormal findings described on cranial CT and MRI scans can also be demonstrated on cranial sonography. Commercially available equipment is used, with transducers of 3-7.5 MHz (depending on the size of the patient's head). Transducers of 5-7.5 MHz are used for newborns, and transducers of 3-5 MHz are used for older infants.
(See the US images of Dandy-Walker malformation below.)
 Dandy-Walker malformation. An in utero sonogram of Dandy-Walker malformation; note the abnormal cerebellar vermis in association with a posterior fossa cyst (arrow) and splaying of the cerebellar hemispheres. Image courtesy of Ecker et al.
Dandy-Walker malformation. An in utero sonogram of Dandy-Walker malformation; note the abnormal cerebellar vermis in association with a posterior fossa cyst (arrow) and splaying of the cerebellar hemispheres. Image courtesy of Ecker et al.
 Dandy-Walker malformation. An antenatal sonogram that shows Dandy-Walker malformation (arrow) in a fetus. Courtesy of Umit Aksoy, MD, Uludag University, Bursa, Turkey.
Dandy-Walker malformation. An antenatal sonogram that shows Dandy-Walker malformation (arrow) in a fetus. Courtesy of Umit Aksoy, MD, Uludag University, Bursa, Turkey.
On US, a large posterior fossa midline cyst that communicates with the fourth ventricle is best demonstrated on midline sagittal sections. The anterolaterally displaced hypoplastic cerebellar hemispheres are best seen in the coronal projection. Sagittal and coronal sections can demonstrate enlargement of the posterior fossa, high position of the tentorium, and dilated third and lateral ventricles.
Scans performed with the transducer can show a large posterior fossa cyst and hypoplastic cerebellar hemispheres. This is accomplished by using the transfontanel approach, as well as by placing the transducer directly over the posterior or posterolateral fontanelle.
In these patients, it is important to assess the supratentorial compartment for associated anomalies, such as callosal agenesis.
Using US, Dandy-Walker malformation is usually discovered before birth, although prominence of the cisterna magna is often confused with Dandy-Walker malformation in utero.
Prenatal diagnosis of Dandy-Walker malformation should not be made before the 18th week of gestation, because development of the cerebellar vermis may be incomplete at that time. Although great variability exists in intracranial findings in fetuses, sagittal measurements exceeding 10 mm help confirm the presence of a Dandy-Walker cyst.
However, a study of the feasiblity of US visualization and measurement of the fetal posterior fossa anatomy at 11-14 weeks' gestation found that a large brainstem‐to‐occipital bone (BSOB) diameter and a decreased brainstem:BSOB ratio, particularly in combination with the presence of only 2 brain spaces, is an important risk factor for cystic posterior fossa malformations, most frequently Dandy-Walker malformation. [41]
US examination, including fetal echocardiography, should be directed toward identifying additional supratentorial and extracranial anomalies. Follow-up sonograms are useful for monitoring cyst size and ventriculomegaly. Three-dimensional US reportedly proved most helpful in delineating the exact nature and anatomic level of the anomaly in utero. [24, 21, 42, 43, 44]
US is heavily operator-dependent. Associated findings of Dandy-Walker malformation, such as pachygyria, polymicrogyria, heterotopias, and dural abnormalities, may be missed. Fetal US can demonstrate Dandy-Walker malformation and variant, but caution should be exercised because the normal developing cerebellum can mimic hypoplasia.
Angiography
Radiographic angiography can demonstrate angiographic features of Dandy-Walker malformation. In the arterial phase, the posterior cerebral vessels are elevated. The superior cerebellar arteries are displaced anterosuperiorly above the posterior cerebral arteries. The posterior inferior cerebellar arteries (PICAs) are shortened, with high tonsillar loop. The inferior vermian branches of the PICA are absent. In some patients, the entire PICA is absent or hypoplastic. In the venous phase, arteriography shows absence of the inferior vermian veins, elevation of the great vein of Galen, and high position of the transverse sinuses. [45]
-
Dandy-Walker malformation. A sagittal T1-weighted magnetic resonance imaging (MRI) scan in a 5-year-old girl (also see the following 2 images) shows a large posterior fossa cyst elevating the torcular herophili and sinus rectus (short arrow). The hypoplastic vermis is everted over the posterior fossa cyst (long arrow). The cerebellar hemispheres and brainstem (b) are hypoplastic. Thinned occipital squama is seen (arrowheads).
-
Dandy-Walker malformation. An axial T2-weighted MRI scan that shows hydrocephalus, a large cerebrospinal fluid cyst in the posterior fossa, thinned occipital bone (arrows), and hypoplastic cerebellar hemispheres with a winged appearance (c).
-
Dandy-Walker malformation. An axial T1-weighted MRI scan showing ventriculomegaly and a superiorly displaced posterior fossa cyst.
-
Dandy-Walker malformation. This sagittal T1-weighted MRI scan in an 11-day-old boy (also see the following image) shows agenesis of the corpus callosum, a hypoplastic brainstem (b), elevation of the torcular herophili (lambdoid-torcular inversion, large arrow), a large fourth ventricle, and a markedly hypoplastic vermis that is rotated superiorly (small arrow).
-
Dandy-Walker malformation. An axial T1-weighted MRI showing an elevated, anteriorly displaced torcular herophili (arrow) and a superiorly displaced posterior fossa cyst.
-
Dandy-Walker malformation. An axial computed tomography (CT) scan in a 7-year-old girl with hydrocephalus showing a large cerebrospinal fluid cyst in the posterior fossa and hypoplastic cerebellar hemispheres with a winged appearance (c).
-
Dandy-Walker malformation. An axial CT scan in a 1-day-old boy that shows a large posterior fossa cyst, separation of the lambdoid sutures (large arrows), and concavity of the petrous ridges (small arrows).
-
Dandy-Walker malformation. This sagittal T1-weighted MRI shows agenesis of the corpus callosum and a hypoplastic inferior vermis in a 13-year-old girl with thoracal scoliosis and Dandy-Walker variant. The fourth ventricle is slightly enlarged, but the posterior fossa typically is normal in size.
-
Dandy-Walker malformation. This sagittal T1-weighted MRI shows a large retrocerebellar cerebrospinal fluid collection and a normal fourth ventricle and vermis in a patient with mega cisterna magna in Dandy-Walker malformation.
-
Dandy-Walker malformation. A posterior fossa arachnoid cyst in a 15-month-old girl with a lumbar pilonidal sinus. The sagittal T1-weighted MRI shows a large posterior fossa cyst that is compressing the cerebellar hemispheres, vermis, fourth ventricle (arrow), and brainstem.
-
Dandy-Walker malformation. Joubert syndrome in an 8-month-old boy. The axial CT scan obtained near the pontomesencephalic junction shows a batwing configuration of the fourth ventricle and unusual definition of the superior cerebellar peduncles at this level (arrows). The vermis is dysgenetic, and the 2 cerebellar hemispheres appose each other in the midline.
-
Dandy-Walker malformation. An in utero sonogram of Dandy-Walker malformation; note the abnormal cerebellar vermis in association with a posterior fossa cyst (arrow) and splaying of the cerebellar hemispheres. Image courtesy of Ecker et al.
-
Dandy-Walker malformation. An antenatal sonogram that shows Dandy-Walker malformation (arrow) in a fetus. Courtesy of Umit Aksoy, MD, Uludag University, Bursa, Turkey.
-
Dandy-Walker malformation. An antenatal MRI showing Dandy-Walker malformation in a fetus. Courtesy of Umit Aksoy, MD, Uludag University, Bursa, Turkey.
-
A CT scan depicting Dandy-Walker malformation.
-
Dandy-Walker malformation. An axial CT scan showing the sinus confluence (large arrow) and sinus transversus (small arrows) displaced superiorly in Dandy-Walker malformation (lambdoid-torcular inversion).