Practice Essentials
Cystic hygroma belongs to a group of diseases recognized as lymphatic malformations and is also known as macrocystic lymphatic malformation or cystic lymphangioma. In cystic hygroma (shown in the ultrasonograms below), cavernous lymphatic spaces communicate and grow to form large cysts that can infiltrate the surrounding tissue. Cystic hygromas can be discovered before birth or during the neonatal period. [1, 2, 3, 4, 5, 6] Occasionally, the cystic hygroma may not be discovered until the patient is older. The majority of cystic hygromas are found in the neck, followed by the axillary region, including the chest wall. [7] Rarely, cystic hygromas are located in intra-abdominal organs, limbs, bones, and mediastinum. [8]
Lymphatic malformations are rare malformations of segregated lymphatic tissues that have not developed into lymphatic tissues with normal connections of regional lymphatic drainage and have resulted in dilatation of abnormal channels. They are divided into 3 types: microcystic, macrocystic, and combined. The macrocystic lymphatic malformations were historically known as cystic hygromas, and microcystic malformations were known as capillary and cavernous lymphangioma. [5]
The effect and prognosis of cystic hygromas vary, depending on whether they are discovered during the prenatal or postnatal period. [9] Prenatal monitoring includes serial ultrasound serveillence of lesion growth; MRI may also be helpful to assess the size. Intrauterine sclerotherapy may be indicated in select patients. [8]
 Oblique longitudinal ultrasonogram obtained through the fetal head and thorax. The red arrowindicates cystic hygroma. Note the normal pocket of amniotic fluid.
Oblique longitudinal ultrasonogram obtained through the fetal head and thorax. The red arrowindicates cystic hygroma. Note the normal pocket of amniotic fluid.
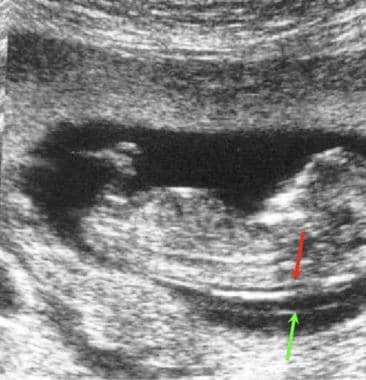 Normal nuchal translucency (red arrow) on a sagittal section in a fetus. The amniotic membrane is depicted separately (green arrow).
Normal nuchal translucency (red arrow) on a sagittal section in a fetus. The amniotic membrane is depicted separately (green arrow).
 Oblique transverse ultrasonogram of the fetal skull shows posterior cystic hygroma (same patient as in previous image).
Oblique transverse ultrasonogram of the fetal skull shows posterior cystic hygroma (same patient as in previous image).
Imaging modalities
Ultrasonography (US) is the modality of choice for diagnosing fetal cystic hygromas. [10] US is readily available and noninvasive, and it is used extensively during pregnancy for fetal monitoring and diagnosis. Fetal positioning, maternal body habitus, and operator dependence can make the diagnosis of cystic hygroma with US difficult at times. [11, 12, 13] Moreover, the diagnosis can be missed, even with large fetal cystic hygromas, when severe oligohydramnios is present; the hygromas can be mistaken for pockets of amniotic fluid (as demonstrated in the image below).
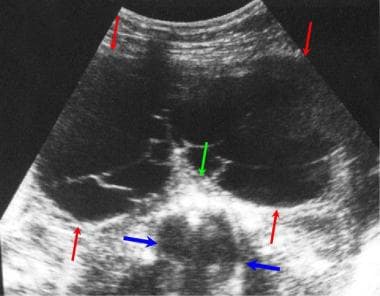 Ultrasonogram shows a massive posterior cystic hygroma (red arrows) behind the thorax (blue arrows). Image illustrates the potential for mistaking hygromas for pockets of amniotic fluid. Note the internal septa. The green arrowindicates the spine.
Ultrasonogram shows a massive posterior cystic hygroma (red arrows) behind the thorax (blue arrows). Image illustrates the potential for mistaking hygromas for pockets of amniotic fluid. Note the internal septa. The green arrowindicates the spine.
Computed tomography (CT) scanning uses ionizing radiation and is contraindicated in pregnancy unless overriding considerations are involved.
Plain radiography also uses ionizing radiation and is contraindicated. Moreover, the findings from plain radiographs are not helpful; cystic hygroma affects the soft tissue, so the images are unlikely to have good contrast.
Magnetic resonance imaging (MRI) can be used to assess the extent of infiltration of the cysts into the surrounding structures, but special fast MRI sequences must be used to overcome normal fetal movement. In addition, MRI requires a long acquisition time, the modality is expensive, and it is not readily available in all settings. [14, 15, 13]
Magnetic Resonance Imaging
The long acquisition times inherent in most MRI acquisition sequences make the use of MRI impractical unless special fast sequences are performed. In optimal settings, MRI can provide exquisite anatomic detail, and it can be especially helpful in identifying additional pathology, as well as in determining the extent of the disease.
On T1-weighted sequences, cystic hygromas present a low signal intensity; on T2-weighted sequences, they demonstrate a high signal intensity with low-signal septations of variable thickness. Hemorrhagic cysts or cysts possessing chylous lipid contents may demonstrate a high signal intensity on T1-weighted sequences. A fluid-fluid level has been recorded with hemorrhagic cysts. [14]
MRI can be used with a high degree of confidence in the diagnosis of cystic hygroma. Usually, further imaging modalities are not needed if good-quality MRI studies are obtained. [15]
Although a hemangioma can appear similar to a cystic hygroma, the hemangioma usually is found in a different location, and after contrast is administered, feeding vessels may be seen, in addition to tumor enhancement.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). NSF/NFD has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or magnetic resonance angiography (MRA) scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Ultrasonography
It has been suggested that the prenatal diagnosis of cystic hygromas is particularly aided by transvaginal ultrasonography. In fact, the condition is most often diagnosed by using prenatal US, and the findings can be striking and unmistakable. [11]
(The ultrasonographic characteristics of cystic hygromas are demonstrated in the images below.)
 Oblique longitudinal ultrasonogram obtained through the fetal head and thorax. The red arrowindicates cystic hygroma. Note the normal pocket of amniotic fluid.
Oblique longitudinal ultrasonogram obtained through the fetal head and thorax. The red arrowindicates cystic hygroma. Note the normal pocket of amniotic fluid.
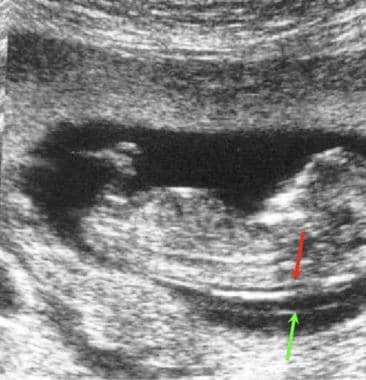 Normal nuchal translucency (red arrow) on a sagittal section in a fetus. The amniotic membrane is depicted separately (green arrow).
Normal nuchal translucency (red arrow) on a sagittal section in a fetus. The amniotic membrane is depicted separately (green arrow).
 Oblique transverse ultrasonogram of the fetal skull shows posterior cystic hygroma (same patient as in previous image).
Oblique transverse ultrasonogram of the fetal skull shows posterior cystic hygroma (same patient as in previous image).
 Longitudinal ultrasonogram through the fetal head and thorax shows huge cystic hygromas extending to the top of the skull (arrows).
Longitudinal ultrasonogram through the fetal head and thorax shows huge cystic hygromas extending to the top of the skull (arrows).
The classic finding in cystic hygroma is a cystic mass with multiple septa (see the image below) that appears as multiple, asymmetrical, thin-walled cysts related to the posterior aspect of the neck. These masses are associated with aneuploidy.
 Transverse ultrasonogram of the thorax in a fetus with hydrops. Note the thickened skin and subcutaneous tissue with multiple small cystic spaces. A fetal pleural collection is noted.
Transverse ultrasonogram of the thorax in a fetus with hydrops. Note the thickened skin and subcutaneous tissue with multiple small cystic spaces. A fetal pleural collection is noted.
If the hygroma is large, the cysts can extend to the lateral or even to the anterior aspects of the neck (as in the first image below). The presence of a nuchal ligament (see the second image below), which is demonstrated as a posterior midline band extending through the cyst, is a characteristic finding. [14, 16]
 Transverse ultrasonogram through the fetal neck shows posterior cystic hygromas extending around the neck to the anterior aspect.
Transverse ultrasonogram through the fetal neck shows posterior cystic hygromas extending around the neck to the anterior aspect.
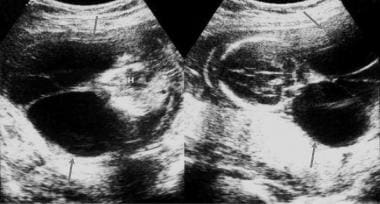 Ultrasonograms show large posterior cystic hygromas (arrows) behind the thorax on the left and the skull on the right. Note the nuchal ligament extending backwards from the spine in both images. H indicates the heart.
Ultrasonograms show large posterior cystic hygromas (arrows) behind the thorax on the left and the skull on the right. Note the nuchal ligament extending backwards from the spine in both images. H indicates the heart.
US remains an operator-dependent modality and must be performed by a trained individual who is skilled in evaluating fetal anomalies. A thorough fetal examination results in a high confidence level. Most often, US is the only technique that is necessary for prenatal diagnosis.
Fetal cystic hygromas should be differentiated from posterior encephaloceles (demonstrated in the image below), in which an underlying skull defect is present, and from cervical myelomeningoceles, in which an underlying vertebral defect is present.
 Large, posterior encephalocele. Note the underlying skull defect demonstrated on this ultrasonogram in a fetus with cystic hygroma.
Large, posterior encephalocele. Note the underlying skull defect demonstrated on this ultrasonogram in a fetus with cystic hygroma.
Oligohydramnios can occur, but this is not a typical finding. When it does arise, it can limit the discovery of cardiac or other visceral abnormalities that can coexist with cystic hygroma. These abnormalities should be investigated. Some patients have features of hydrops, which may be diagnosed by identifying body wall edema, pleural effusions, and/or fetal ascites. [17]
As previously mentioned, the diagnosis of cystic hygroma can be missed, even with large fetal cystic hygromas, when severe oligohydramnios is present; the hygromas can be mistaken for pockets of amniotic fluid (as demonstrated in the image below).
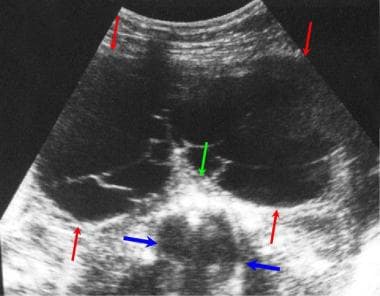 Ultrasonogram shows a massive posterior cystic hygroma (red arrows) behind the thorax (blue arrows). Image illustrates the potential for mistaking hygromas for pockets of amniotic fluid. Note the internal septa. The green arrowindicates the spine.
Ultrasonogram shows a massive posterior cystic hygroma (red arrows) behind the thorax (blue arrows). Image illustrates the potential for mistaking hygromas for pockets of amniotic fluid. Note the internal septa. The green arrowindicates the spine.
A common artifact is caused by the presence of loops of umbilical cord near the cervical spine of the fetus. On occasion, these loops can simulate cervical cysts. A Doppler ultrasound evaluation demonstrates characteristic umbilical flow signals from this area. Fetal cystic hygroma must also be differentiated from other neck masses and cysts, such as anterior cystic hygromas, goiters, and cervical teratomas.
Compared with other masses, purely anterior cystic masses in the fetal neck have a different and better prognosis, and many resolve spontaneously.
-
Oblique longitudinal ultrasonogram obtained through the fetal head and thorax. The red arrowindicates cystic hygroma. Note the normal pocket of amniotic fluid.
-
Normal nuchal translucency (red arrow) on a sagittal section in a fetus. The amniotic membrane is depicted separately (green arrow).
-
Oblique transverse ultrasonogram of the fetal skull shows posterior cystic hygroma (same patient as in previous image).
-
Ultrasonogram shows a massive posterior cystic hygroma (red arrows) behind the thorax (blue arrows). Image illustrates the potential for mistaking hygromas for pockets of amniotic fluid. Note the internal septa. The green arrowindicates the spine.
-
Longitudinal ultrasonogram through the fetal head and thorax shows huge cystic hygromas extending to the top of the skull (arrows).
-
Transverse ultrasonogram through the fetal neck shows posterior cystic hygromas extending around the neck to the anterior aspect.
-
Ultrasonograms show large posterior cystic hygromas (arrows) behind the thorax on the left and the skull on the right. Note the nuchal ligament extending backwards from the spine in both images. H indicates the heart.
-
Coronal ultrasonogram of a fetal thorax showing axillary cystic hygromas (arrow) and the heart.
-
Large, posterior encephalocele. Note the underlying skull defect demonstrated on this ultrasonogram in a fetus with cystic hygroma.
-
Transverse ultrasonogram of the thorax in a fetus with hydrops. Note the thickened skin and subcutaneous tissue with multiple small cystic spaces. A fetal pleural collection is noted.






