Practice Essentials
Craniopharyngioma is a histologically benign, extra-axial, slow-growing tumor that predominantly involves the sella and suprasellar space (see the images below). Despite its histologic appearance, craniopharyngiomas occasionally behave like malignant tumors. They can metastasize, and patients can have severe symptoms that usually require surgery and/or radiation therapy (with intracystic chemotherapy in some pediatric patients). Recurrences, both local and along surgical tracts, have been reported, as has meningeal seeding. Characteristic radiographic findings help differentiate craniopharyngiomas from other tumors that can occur in the same anatomic region. [1, 2, 3, 4, 5, 6, 7]
There are 2 subtypes: adamantinomatous craniopharyngioma(ACP) and papillary craniopharyngioma(PCP). ACPs have a bimodal peak of incidence (5-15 years and 45-60 years), and PCPs occur only in adults primarily during the fifth and sixth decades of life. The incidence of craniopharyngiomas is 0.5-2.0 new cases per million population per year, and approximately 30-50% of cases occur in childhood. Typical manifestations include headache, visual impairment, polyuria or polydypsia, growth retardation, and weight gain. The treatment of choice is total resection in patients in whom there is favorable tumor localization, to maintain hypothalamic-pituitary and optical nerve functions. If localization is not favorable, the recommended treatment is limited resection followed by local irradiation. Overall survival rates are 91-98%, but long-term sequelae can reduce the quality of life in about 50% of survivors, particularly extreme obesity resulting from involvement of the hypothalamus. [8, 9, 10, 11]
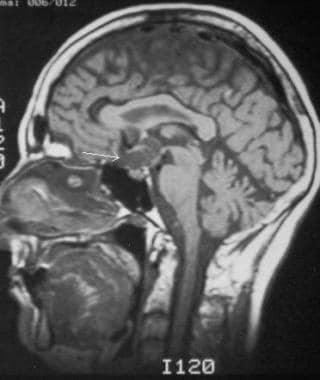
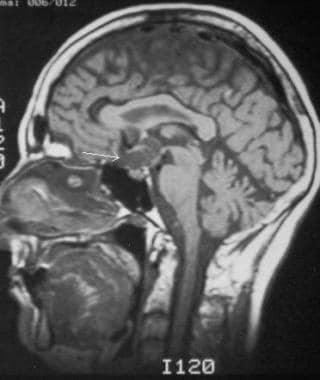
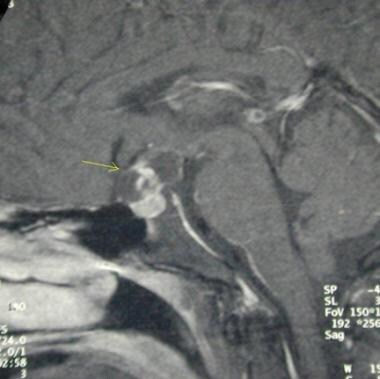
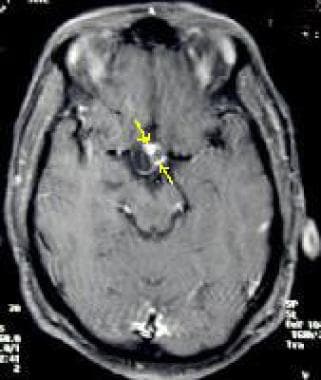
 Contrast-enhanced T1-weighted image demonstrates a complex cystic mass (arrow) in the suprasellar space.
Contrast-enhanced T1-weighted image demonstrates a complex cystic mass (arrow) in the suprasellar space.
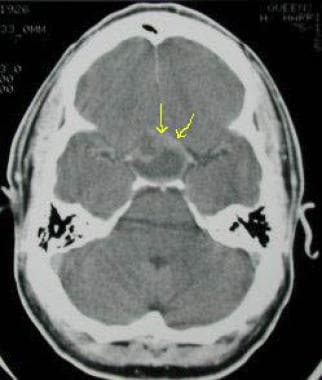
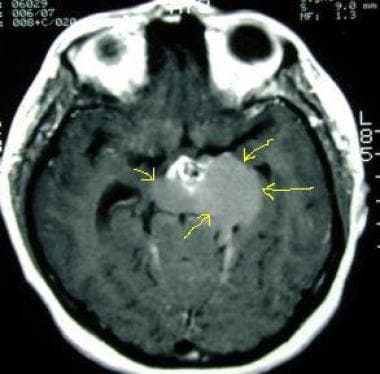
 Axial contrast-enhanced CT scan in a 65-year-old man demonstrates a large, calcified suprasellar mass with anterior displacement of the A1 segment of the anterior cerebral arteries (yellow arrows). The anterior communicating artery is not well depicted.
Axial contrast-enhanced CT scan in a 65-year-old man demonstrates a large, calcified suprasellar mass with anterior displacement of the A1 segment of the anterior cerebral arteries (yellow arrows). The anterior communicating artery is not well depicted.
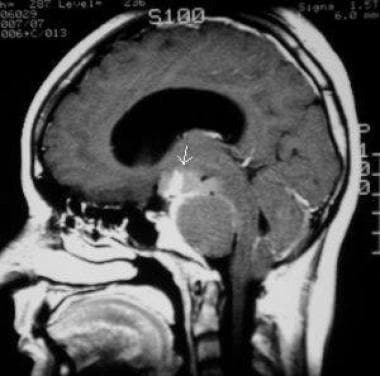
 Contrast-enhanced T1-weighted image in a 66-year-old woman (same patient as in following image) obtained in a slightly lateral parasagittal plane demonstrates irregular enhancement of the solid components (arrow) and the outer rim of the tumor, which has a predominantly cystic composition.
Contrast-enhanced T1-weighted image in a 66-year-old woman (same patient as in following image) obtained in a slightly lateral parasagittal plane demonstrates irregular enhancement of the solid components (arrow) and the outer rim of the tumor, which has a predominantly cystic composition.
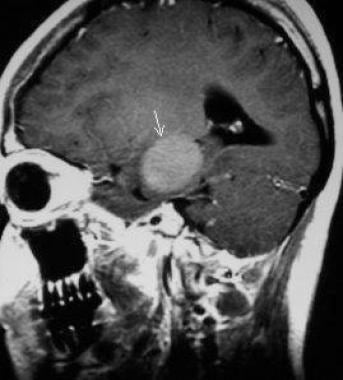
 Sagittal nonenhanced T1-weighted image demonstrates a heterogeneous, cystic mass (arrows) in the suprasellar space (same patient as in previous image).
Sagittal nonenhanced T1-weighted image demonstrates a heterogeneous, cystic mass (arrows) in the suprasellar space (same patient as in previous image).
Preferred examination
CT and MRI are the complementary examinations of choice. [12, 13] The best imaging tool is MRI, both with and without contrast enhancement. CT can clearly demonstrate the characteristic calcifications and size of the tumor, whereas MRI exquisitely demonstrates the size and extent of the tumor and involvement of the third ventricle. MRI results can confirm cystic features of the tumor. Sequences such as fluid-attenuated inversion recovery (FLAIR), [14] gradient-echo (GRE) imaging, and diffusion-weighted imaging, as well as MR spectroscopy, can be used to make a confident and correct diagnosis. [15, 16, 17]
Plain radiography may show abnormalities; however, CT or MRI is still needed regardless of the plain radiographic findings. CT and MRI have supplanted angiography as the primary diagnostic modality; magnetic resonance angiography (MRA) or CT angiography (CTA) may be helpful in differentiating the tumor from an aneurysm of the anterior communicating artery.
In the later postoperative period, CT can be performed to establish the baseline for future follow-up scans and to determine the number and size of residual flecks of calcification. In the immediate postoperative period (first 48 hr) and later, gadolinium-enhanced MRI may be performed to establish a baseline appearance and to determine whether residual tumor is present. [18, 19, 20, 21, 22, 23, 24, 25, 26, 27]
Nonenhanced CT may be required to detect calcifications if typical MRI findings are absent. A papillary-type lesion can be missed on MRI or CT when no characteristic cystic component is present or when lesions are not enhanced after the administration of intravenous (IV) contrast material (as occurs in approximately 10% of patients).
Micro-CT imaging can be used to map tumor invasion by non-destructively providing detailed 3D structural information of tumors in volumes with isotropic voxel sizes of 4–6 microns, which can be correlated with traditional histology and immunohistochemistry. [28]
With the wide availability and documented accuracy of CT and MRI, ultrasonography has not been accepted as a universal tool for the evaluation of pituitary masses. A few case reports have described the use of ultrasonography with color Doppler imaging in the antenatal diagnosis of fetal craniopharyngiomas. Adult craniopharyngiomas have also been evaluated with the use of color Doppler and ultrasonographic contrast agents. [21, 23, 26] However, the modality is operator dependent, it can be limited because of beam attenuation by the bony skull vault, and lesions may be missed.
Limitations
MRI cannot be used in patients with pacemakers or implanted ferromagnetic metallic objects or in those with metallic foreign bodies in the brain, spinal cord, or soft tissues near important vascular structures. The use of MRI also is limited in patients with claustrophobia and in those who are unable to remain stationary for the required time. Both CT and MRI evaluations require IV contrast enhancement; therefore, IV access is needed.
Failure to make the diagnosis is a pitfall because tumor calcifications on CT may be misinterpreted as enhancing aneurysms, and correlation with cerebral angiographic findings may be needed to differentiate the 2 entities. In addition, calcifications appear as signal voids on MRI and can be misinterpreted as aneurysms. MRA should be performed in questionable cases.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Radiography
In craniopharyingiomas, lateral radiograph of the skull may demonstrate calcifications in either the sella turcica or suprasellar space (see the first image below), or it may demonstrate sellar expansion or erosion of clinoid process or dorsum sella (see the second image below).
 Digital radiograph in a 23-year-old woman demonstrates characteristic calcifications (arrow) in the suprasellar space. This appearance can easily be misinterpreted as that of an aneurysm.
Digital radiograph in a 23-year-old woman demonstrates characteristic calcifications (arrow) in the suprasellar space. This appearance can easily be misinterpreted as that of an aneurysm.
 Digital radiograph in a 39-year-old man demonstrates characteristic expansion of the sella turcica (arrows).
Digital radiograph in a 39-year-old man demonstrates characteristic expansion of the sella turcica (arrows).
These calcifications can be confused with curvilinear calcifications observed with large aneurysms (occasionally referred to as eggshell calcifications). An aneurysm may be differentiated on contrast-enhanced CT, which demonstrates characteristic enhancement of the remainder of the lumen of the aneurysm, and on MRI, which shows heterogeneity of signal intensity and misregistration artifact from turbulent or pulsatile flow in the aneurysm. MRA further helps elucidate the diagnosis in questionable cases. [4, 19, 20, 21, 23, 29]
The degree of confidence for a negative result is low because small calcifications can be missed easily. When observed, calcifications are a nonspecific finding. Soft tissue visualization on plain radiography is poor; therefore, differentiation of the type of tumor present is not possible without further imaging.
Computed Tomography
On CT, the adamantinomatous-type tumor appears as a predominantly cystic mass (see the image below) with a solid component (>90%). The solid component appears isoattenuating and usually contains calcifications (>80%). The sella may be expansile, and hydrocephalus may be present, depending on the exact location of the tumor. Tumors of the papillary type are usually solid and isoattenuating; they are rarely calcified. Occasionally, craniopharyngioma may appear as an intraventricular, homogeneous soft tissue mass without calcifications but possibly with hypoattenuating regions; this is observed in the papillary subtype. [21]
 Axial CT scan in a 39-year-old man (same patient as in the following image) obtained without contrast enhancement demonstrates a large, cystic mass (arrow) in the suprasellar space that has predominantly fluid attenuation.
Axial CT scan in a 39-year-old man (same patient as in the following image) obtained without contrast enhancement demonstrates a large, cystic mass (arrow) in the suprasellar space that has predominantly fluid attenuation.
The location of the adamantinomatous subtype is characteristic because most are located in the sella or suprasellar region. Contrast enhancement is characteristic of the solid component (see the first image below) and cyst wall (90% cases), and an enhanced study may demonstrate displacement of the A1 segment of the anterior cerebral artery (see the second image below). Displacement of the optic chiasm also may be observed.
 CT scan in a 39-year-old man (same patient as in the previous image) obtained with intravenous contrast agent shows enhancement of the anterior, solid component (arrows).
CT scan in a 39-year-old man (same patient as in the previous image) obtained with intravenous contrast agent shows enhancement of the anterior, solid component (arrows).
 Axial contrast-enhanced CT scan in a 65-year-old man demonstrates a large, calcified suprasellar mass with anterior displacement of the A1 segment of the anterior cerebral arteries (yellow arrows). The anterior communicating artery is not well depicted.
Axial contrast-enhanced CT scan in a 65-year-old man demonstrates a large, calcified suprasellar mass with anterior displacement of the A1 segment of the anterior cerebral arteries (yellow arrows). The anterior communicating artery is not well depicted.
On CT, the cystic component of the tumor extends anteriorly and/or laterally and typically wraps around the solid component. Conversely, the solid component characteristically extends posteriorly and laterally.
The degree of confidence is high because CT is sensitive for calcifications and for visualizing the cystic nature of masses. As with MRI, the noncalcified, papillary variant may sometimes be missed. A Rathke cleft cyst is rarely calcified, whereas more than 90% of craniopharyngiomas are calcified.
Magnetic Resonance Imaging
On MRI, the more common adamantinomatous subtype appears as a predominantly cystic suprasellar mass with a solid component (see the image below). Characteristic calcifications may not be discernible, though gradient-echo (GRE) images may show susceptibility effects from calcified components. Cystic areas appear hyperintense on T2-weighted and fluid-attenuated inversion recovery (FLAIR) images with heterogeneous isointense to hypointense solid components. [14, 15, 19, 21, 23, 25, 30]
 Contrast-enhanced T1-weighted image demonstrates a complex cystic mass (arrow) in the suprasellar space.
Contrast-enhanced T1-weighted image demonstrates a complex cystic mass (arrow) in the suprasellar space.
Changes in signal intensity vary on T1-weighted images, depending on the cystic contents, which can appear hyperintense if they have a high protein, blood product, and/or cholesterol content in the classic adamantinomatous type. In the papillary variety, solid components appear isointense on T1-weighted images.
Magnetic resonance (MR) spectroscopy shows a prominent lipid spectrum (around 1 ppm) in terms of the cystic contents. Diffusion-weighted images demonstrate variable signal intensity, which reflects the cystic contents.
The sella may be expansile, and hydrocephalus may be present, depending on the exact location of the tumor. Compression of the third ventricle may occur; when present, such compression helps distinguish craniopharyingioma from Rathke cleft cyst or pituitary adenoma. Occasionally, craniopharyngiomas appear as intraventricular, homogeneous, soft tissue masses without calcifications. They may contain regions of low signal intensity; this is observed in the papillary subtype.
Some craniopharyingiomas can be both intrasellar and suprasellar, having a "snowman" appearance. [15] The location of the adamantinomatous subtype is characteristic, with most tumors located in the sellar or suprasellar region (see the images below).
 Coronal T1-weighted image in a 65-year-old man obtained through the sella turcica. Image demonstrates a predominantly sellar lesion (arrows) with some suprasellar extension.
Coronal T1-weighted image in a 65-year-old man obtained through the sella turcica. Image demonstrates a predominantly sellar lesion (arrows) with some suprasellar extension.
 Contrast-enhanced T1-weighted image in a 66-year-old woman (same patient as in following image) obtained in a slightly lateral parasagittal plane demonstrates irregular enhancement of the solid components (arrow) and the outer rim of the tumor, which has a predominantly cystic composition.
Contrast-enhanced T1-weighted image in a 66-year-old woman (same patient as in following image) obtained in a slightly lateral parasagittal plane demonstrates irregular enhancement of the solid components (arrow) and the outer rim of the tumor, which has a predominantly cystic composition.
 Sagittal nonenhanced T1-weighted image demonstrates a heterogeneous, cystic mass (arrows) in the suprasellar space (same patient as in previous image).
Sagittal nonenhanced T1-weighted image demonstrates a heterogeneous, cystic mass (arrows) in the suprasellar space (same patient as in previous image).
Contrast enhancement is characteristic (see the images below). MR angiography may demonstrate displacement of the A1 segment of the anterior cerebral artery; displacement of the optic chiasm may also be observed.
 Sagittal contrast-enhanced T1-weighted MRI demonstrates a complex cystic, suprasellar mass that is heterogeneously enhancing (arrow).
Sagittal contrast-enhanced T1-weighted MRI demonstrates a complex cystic, suprasellar mass that is heterogeneously enhancing (arrow).
 Gadolinium-enhanced parasagittal T1-weighted MRI in a 23-year-old woman (same patient as in the previous image) demonstrates the characteristic enhancement of the solid component (arrow) of craniopharyngioma.
Gadolinium-enhanced parasagittal T1-weighted MRI in a 23-year-old woman (same patient as in the previous image) demonstrates the characteristic enhancement of the solid component (arrow) of craniopharyngioma.
On MRI, the cystic component of the tumor extends anteriorly and/or laterally and typically wraps around the solid component (see the images below).
 T1-weighted MRI of a 23-year-old woman (same patient as in the following 2 images) demonstrates a suprasellar mass with characteristic intermediate- to high-signal material in the cystic material (arrows).
T1-weighted MRI of a 23-year-old woman (same patient as in the following 2 images) demonstrates a suprasellar mass with characteristic intermediate- to high-signal material in the cystic material (arrows).
 Sagittal T1-weighted MRI in a 23-year-old woman (same patient as in the following image) demonstrates the high signal intensity of the cystic material (yellow arrow).
Sagittal T1-weighted MRI in a 23-year-old woman (same patient as in the following image) demonstrates the high signal intensity of the cystic material (yellow arrow).
Conversely, the solid component of the tumor characteristically extends posteriorly and laterally (see the image below).
 Axial contrast-enhanced T1-weighted MRI demonstrates enhancement of the solid component (arrows) of the lesion.
Axial contrast-enhanced T1-weighted MRI demonstrates enhancement of the solid component (arrows) of the lesion.
Adjacent brain parenchyma may show hyperintensity on T2-weighted or FLAIR images, which indicates edema from compression of optic chiasm and/or tracts, gliosis, or tumor invasion. Recurrence in both the local tumor bed and along surgical tracts may the result of implantation of craniopharyngioma tissue. Therefore, post-treatment MRI has been recommended, even in patients whose primary tumor was resected completely. [25, 15]
The degree of confidence is high. Although MRI without a GRE sequence can be insensitive for calcifications, it is sensitive for determining the fluid or soft tissue content of a given area. False-positive results may occur as a result of misidentification of a similar lesion in the differential diagnosis.
A Rathke cleft cyst (RCC) can usually be differentiated because it is rarely calcified, whereas 64-92% of craniopharyngiomas are calcified. An RCC is also usually associated with anterior infundibular displacement and does not have a solid component. In addition, it shows contrast enhancement less frequently than other tumors do. Small RCCs may be indistinguishable from the rare intrasellar craniopharyngiomas.
A suprasellar arachnoid cyst has angular margins and is entirely cystic, with no solid component or enhancement.
Hypothalamic or chiasmatic astrocytomas arise at their respective locations and appear solid with areas of necrosis. The pilocytic variety may show cystic changes; however, calcification is less common with this tumor than with others. A moderate degree of enhancement may be seen.
Meningiomas demonstrate the dural tail sign, which is absent with craniopharyngiomas. Meningiomas also have a wide dural base and densely adhere to the dura. A craniopharyngioma can grow to more than 5 cm, but most are smaller. Conversely, a germinoma is almost always large, and its signal intensity and enhancement are homogeneous. A cystic component rarely is observed, and a pineal satellite lesion may be present.
Pituitary adenoma is rare in children; it is mostly intrasellar in the microadenoma variety. Macroadenomas may have suprasellar components with cystic, hemorrhagic, and enhancing areas; findings closely mimic those of a craniopharyngioma. However, calcification is rare.
Teratomas contain mixed solid and cystic components, as do craniopharyngiomas, but teratomas typically contain some fat.
Epidermoids can be distinguished by their characteristic scalloped margins and by the fact that, with epidermoids, there is minimal or no peripheral enhancement. Epidermoids are typically strongly hyperintense on diffusion-weighted images. Dermoids also contain a fatty component.
Preoperative MRI
Some preoperative conventional MRI findings have been found to have predictive value. For example, craniopharyngioma adherence is a heterogeneous pathologic feature that may critically influence radical resection. Prieto and colleagues, in a retrospective study of 200 surgically treated craniopharyngiomas, reported that a position of the hypothalamus around the middle portion of the tumor, an amputated or infiltrated appearance of the pituitary stalk, and the elliptical shape of the tumor were reliable predictors of strong and extensive craniopharyngioma adhesions to the hypothalamus. [31]
In another study by Prieto et al, topography of craniopharyngiomas proved fundamental in predicting the involvement of vital brain structures and the possibility of achieving a safe radical resection by comparing preoperative midsagittal and coronal conventional T1- and T2-weighted MR images to detailed descriptions of the surgical findings. Five major craniopharyngioma topographies were defined according to the degree of hypothalamic distortion caused by the tumor: sellar-suprasellar, pseudointraventricular, secondary intraventricular, not strictly intraventricular, and strictly intraventricular. Seven key radiologic variables identified on preoperative MRI allowed a correct overall prediction of craniopharyngioma topography in 86% of cases: (1) third ventricle occupation, (2) pituitary stalk distortion, (3) relative level of the hypothalamus in relation to the tumor, (4) chiasmatic cistern occupation, (5) mammillary body angle, (6) type of chiasm distortion, and (7) tumor shape. [32]
Angiography
CTA and MRA have supplanted angiography as the primary diagnostic techniques, and angiography is now rarely needed to differentiate the tumor from an aneurysm of the anterior communicating artery. On angiography, most of the findings of craniopharyngiomas relate to displacement of the cerebral vasculature secondary to mass effect. Specifically, the position of the anterior cerebral artery is well correlated with the location of the tumor. When the A1 segment of the anterior cerebral artery and the anterior communicating artery are in the usual position, the tumor is contained entirely or almost entirely within the sella.
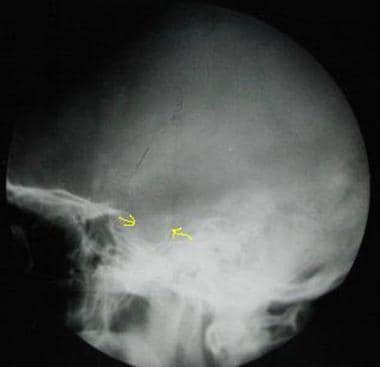
When the A1 segment and the anterior communicating artery are elevated (see the image below) but the basilar artery is in the usual position, the tumor protrudes anteriorly and projects between the optic nerves, deviating the chiasm posteriorly. When the A1 segment and the anterior communicating artery are elevated and the basilar artery is displaced posteriorly, the tumor protrudes posteriorly and pushes the chiasm anteriorly. Stretching of the posterior communicating arteries also may be noted. An unreliable finding is a small, vascular blush in the region of the tumor.
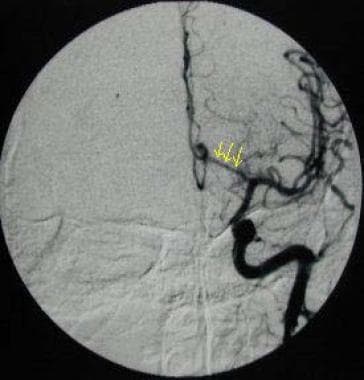 Angiogram obtained in the anteroposterior projection clearly shows elevations of the A1 segment of the anterior cerebral artery (arrows) and anterior communicating artery.
Angiogram obtained in the anteroposterior projection clearly shows elevations of the A1 segment of the anterior cerebral artery (arrows) and anterior communicating artery.
-
Contrast-enhanced T1-weighted image demonstrates a complex cystic mass (arrow) in the suprasellar space.
-
Sagittal contrast-enhanced T1-weighted MRI demonstrates a complex cystic, suprasellar mass that is heterogeneously enhancing (arrow).
-
Axial contrast-enhanced T1-weighted MRI demonstrates enhancement of the solid component (arrows) of the lesion.
-
T1-weighted MRI of a 23-year-old woman (same patient as in the following 2 images) demonstrates a suprasellar mass with characteristic intermediate- to high-signal material in the cystic material (arrows).
-
Sagittal T1-weighted MRI in a 23-year-old woman (same patient as in the following image) demonstrates the high signal intensity of the cystic material (yellow arrow).
-
Gadolinium-enhanced parasagittal T1-weighted MRI in a 23-year-old woman (same patient as in the previous image) demonstrates the characteristic enhancement of the solid component (arrow) of craniopharyngioma.
-
Digital radiograph in a 23-year-old woman demonstrates characteristic calcifications (arrow) in the suprasellar space. This appearance can easily be misinterpreted as that of an aneurysm.
-
Axial CT scan in a 39-year-old man (same patient as in the following image) obtained without contrast enhancement demonstrates a large, cystic mass (arrow) in the suprasellar space that has predominantly fluid attenuation.
-
CT scan in a 39-year-old man (same patient as in the previous image) obtained with intravenous contrast agent shows enhancement of the anterior, solid component (arrows).
-
Digital radiograph in a 39-year-old man demonstrates characteristic expansion of the sella turcica (arrows).
-
Angiogram obtained in the anteroposterior projection clearly shows elevations of the A1 segment of the anterior cerebral artery (arrows) and anterior communicating artery.
-
Axial contrast-enhanced CT scan in a 65-year-old man demonstrates a large, calcified suprasellar mass with anterior displacement of the A1 segment of the anterior cerebral arteries (yellow arrows). The anterior communicating artery is not well depicted.
-
Coronal T1-weighted image in a 65-year-old man obtained through the sella turcica. Image demonstrates a predominantly sellar lesion (arrows) with some suprasellar extension.
-
Contrast-enhanced T1-weighted image in a 66-year-old woman (same patient as in following image) obtained in a slightly lateral parasagittal plane demonstrates irregular enhancement of the solid components (arrow) and the outer rim of the tumor, which has a predominantly cystic composition.
-
Sagittal nonenhanced T1-weighted image demonstrates a heterogeneous, cystic mass (arrows) in the suprasellar space (same patient as in previous image).





