Practice Essentials
Diverticular disease of the colon begins as diverticulosis (colonic outpouchings), which may develop into diverticulitis (diverticular inflammation and perforation). [1, 2, 3, 4] The cause of diverticulitis is probably mechanical. The stagnation of nonsterile inspissated fecal material, termed a fecalith, within the diverticulum may compromise the blood supply to the thin-walled sac and render it susceptible to invasion by colonic bacteria, causing inflammatory erosion of the mucosal lining and perforation. This sequence of events can involve perforation into the colonic wall, with the formation of an intramural abscess. However, perforation usually occurs into the pericolic fat, leading to fibrinous exudate, abscess formation, local adhesions, or peritonitis. Diverticula usually occur adjacent to the vasa recta, the small vessels that extend into the submucosa, because these are the weakest areas of the colonic wall. Therefore, diverticula usually occur on the mesenteric side of the colon.
Most patients develop sealed-off abscesses or contained sinus tracts and fistulas. Fistulas usually involve adjacent structures, such as the bowel, urinary bladder, vagina, and anterior abdominal wall. Other potential complications include bowel obstruction and peritonitis. [5]
Patients with acute colonic diverticulitis may have severe and prolonged lower abdominal pain due to diverticular inflammation that is usually associated with change in bowel movements, fever, and leukocytosis. [6]
Computed tomography (CT) of the abdomen and pelvis with IV contrast is considered to be the best imaging method because it can confirm the presence of acute colonic diverticulitis, evaluate disease severity and degree, and often differentiate colonic diverticulitis from other diseases. [6]
(The radiologic features of diverticulitis are demonstrated in the images below.)
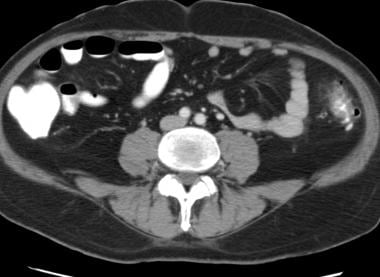 CT scan demonstrates mild diverticulitis of the descending colon, with wall thickening, a diverticulum, and mild stranding of the pericolic fat.
CT scan demonstrates mild diverticulitis of the descending colon, with wall thickening, a diverticulum, and mild stranding of the pericolic fat.
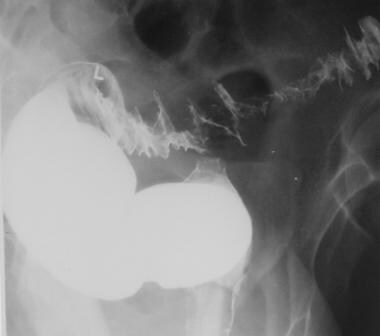
 Single-contrast barium enema study demonstrates diverticulitis of the descending colon with fistula formation in the small bowel.
Single-contrast barium enema study demonstrates diverticulitis of the descending colon with fistula formation in the small bowel.
Diverticula involve the sigmoid colon in as many as 95% of patients with diverticulosis. The cecum is involved in 5% of patients. The sigmoid is the narrowest portion of the colon, and it generates the highest intrasegmental pressures. The combination of numerous haustra and dehydrated stool in the sigmoid colon leads to segmentation, in which the sigmoid colon functions as multiple small compartments. These features account for the high incidence of diverticulosis in the sigmoid colon.
(Diverticulitis involving the sigmoid colon is seen in the images below.)
 Single-contrast barium enema study demonstrates mild sigmoid diverticulitis with thickening of the mucosal folds and luminal narrowing.
Single-contrast barium enema study demonstrates mild sigmoid diverticulitis with thickening of the mucosal folds and luminal narrowing.
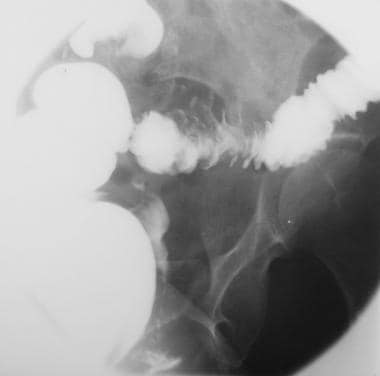
 Single-contrast barium enema study demonstrates sigmoid diverticulitis with a colovesical fistula. Note the contrast material in the bladder.
Single-contrast barium enema study demonstrates sigmoid diverticulitis with a colovesical fistula. Note the contrast material in the bladder.
 Single-contrast barium enema study demonstrates sigmoid diverticulitis with a colovesical fistula. Note the contrast material in the bladder.
Single-contrast barium enema study demonstrates sigmoid diverticulitis with a colovesical fistula. Note the contrast material in the bladder.
 Single-contrast barium enema study demonstrates sigmoid diverticulitis with an intramural sinus tract. Fistula formation in the small bowel is noted.
Single-contrast barium enema study demonstrates sigmoid diverticulitis with an intramural sinus tract. Fistula formation in the small bowel is noted.
 Single-contrast barium enema study demonstrates sigmoid diverticulitis with fistula formation in the vagina.
Single-contrast barium enema study demonstrates sigmoid diverticulitis with fistula formation in the vagina.
 Single-contrast barium enema study demonstrates sigmoid diverticulitis with fistula formation in the cecum.
Single-contrast barium enema study demonstrates sigmoid diverticulitis with fistula formation in the cecum.
Imaging modalities
The preferred examination for diverticulitis is CT scanning of the abdomen and pelvis. CT findings can help in confirming clinical suspicion of diverticulitis and in excluding other abdominal or pelvic disease. CT can help in evaluating and staging inflammatory disease. The modality can also be used to accurately plan a percutaneous intervention. [7, 8, 9, 10, 11, 12] The major limitation of CT scanning is the potential difficulty in differentiating diverticulitis from colon carcinoma. Other limitations of CT are the high cost of the examination and its limited availability in certain regions of the world.
Ultrasonography is occasionally useful in diagnosing acute diverticulitis. The modality is inexpensive, noninvasive, and readily available. Ultrasonography can be used if CT is not available. Ultrasonography may not be helpful in excluding diverticulosis or diverticulitis because of interference due to bowel gas. [13, 14, 15]
Traditionally, barium enema imaging has been the primary method of examining patients in whom diverticulitis is suspected. Barium studies superbly depict diverticula, the colonic mucosa and lumen, spasm, and muscle hypertrophy. [16]
Scanning with technetium-99m (99mTc)–labeled red blood cells often is performed to locate the site of active gastrointestinal tract bleeding, and it may be helpful in evaluating bleeding due to diverticulosis. Nuclear medicine studies have a limited role in the evaluation of diverticulitis. [17]
Approximately one half of all cases of lower gastrointestinal hemorrhage are caused by colonic diverticulosis. Although most diverticula occur in the left side of the colon, diverticular hemorrhage usually originates from the right side. Angiography may demonstrate diverticular hemorrhage as puddling or staining that persists beyond the capillary and venous phases. Embolization or the intra-arterial infusion of vasopressin may be used to treat gastrointestinal bleeding.
Complicated versus Uncomplicated
The guidelines for acute colonic diverticulitis were examined during a consensus conference of the World Society of Emergency Surgery (WSES), and final guidelines were published by Sartelli et al. [18] The new classification system divided the disease into uncomplicated and complicated. Uncomplicated ACD was defined as only the presence of thickening of the intestinal wall, with increased perivisceral fat density. Complicated disease was divided into the following stages [6, 18] :
-
Stage 1A: Presence of microperforation without abscess and/or peritoneum involvement
-
Stage 1B: Presence of abscess with diameter ≤4 cm
-
Stage 2A: Presence of abscess with diameter >4 cm
-
Stage 2B: Presence of distant air >5 cm from the pathologic loop
-
Stage 3: Presence of diffuse fluid in at least 2 distant abdominal quadrants without distant free air
-
Stage 4: Presence of diffuse fluid and distant free air
Guidelines
Because clinical findings correlate poorly with the severity of the disease, imaging is necessary to confirm the diagnosis of acute diverticulitis. All major guidelines recommend computed tomography (CT) for the initial assessment of suspected diverticulitis. [19, 20, 21] Alternative modalities recommended by the European Society of Coloproctology are ultrasonography and magnetic resonance imaging. [19]
The American College of Radiology (ACR) Appropriateness Criteria for initial imaging of suspected diverticulitis recommends CT with IV contrast because it provides a more comprehensive initial assessment of the clinical progression and aids in treatment selection. [21]
In addition to using CT for the initial diagnosis, the American Gastroenterological Association (AGA) and ACR guidelines recommend CT scanning to identify complications of diverticulitis. [20, 21] The AGA also recommends that imaging be considered prior to prophylactic surgery to confirm the diagnosis and location of disease. [20]
Radiography
Plain radiographs usually do not show any findings in uncomplicated diverticulitis, but a left-sided pelvic mass, localized ileus, or partial bowel obstruction may occasionally be seen. Pneumoperitoneum, portal venous gas, and extraluminal air-fluid levels may be noted in patients with complicated diverticulitis.
Barium study
Prior to the advent of abdominal CT scanning, barium enema evaluation was the examination of choice for the diagnosis of diverticulitis. A single-contrast examination is the preferred method in patients in whom diverticulitis is suspected.
The appearance of diverticula varies with the projection in which they are viewed and with the amount of air and barium they contain. In profile, a diverticulum appears as a protrusion outside of the colon that is joined to the colonic wall by a neck. En face, a diverticulum may appear as a well-defined collection of barium or as a ring shadow. It may resemble a bowler hat.
On barium enema examination, diverticulitis can be diagnosed by recognizing a perforated diverticulum. Barium may track through a perforated diverticulum into a sinus tract, fistula, or abscess (see the images below). Less commonly, it may extravasate freely into the peritoneum. A diverticular abscess may cause extrinsic compression of the colonic lumen. Initially, this compression occurs on the mesenteric side of the colon, but it may spread to encircle the lumen.
 Single-contrast barium enema study in a patient with diverticulitis demonstrates tethering of the sigmoid colon as a result of a diverticular abscess.
Single-contrast barium enema study in a patient with diverticulitis demonstrates tethering of the sigmoid colon as a result of a diverticular abscess.
 Single-contrast barium enema study in a patient with diverticulitis demonstrates an intramural abscess filling with barium.
Single-contrast barium enema study in a patient with diverticulitis demonstrates an intramural abscess filling with barium.
 Single-contrast barium enema study demonstrates sigmoid diverticulitis with an intramural sinus tract. Fistula formation in the small bowel is noted.
Single-contrast barium enema study demonstrates sigmoid diverticulitis with an intramural sinus tract. Fistula formation in the small bowel is noted.
Many other features of diverticulitis are depicted on barium enema images. Narrowing, deformity, or displacement of the bowel lumen is commonly seen. The colon may have an abnormal mucosal pattern. A soft-tissue mass may be found, and this mass may contain gas or air-fluid levels.
(Luminal narrowing is seen on the image below.)
 Single-contrast barium enema study demonstrates mild sigmoid diverticulitis with thickening of the mucosal folds and luminal narrowing.
Single-contrast barium enema study demonstrates mild sigmoid diverticulitis with thickening of the mucosal folds and luminal narrowing.
Extraluminal tracts filled with barium may end blindly as sinus tracts or may connect with an adjacent organ (most comonly the bladder or bowel) as a fistula. Fistulas also may involve the vagina, ureter, or hip or the soft tissues of the thigh. (A vaginal fistula is shown below.) Occasionally, plain radiographs demonstrate colovesical fistulas with the presence of air in the bladder. Additional manifestations of diverticulitis include localized ileus and intestinal obstruction. Fistula formation to the anterior abdominal wall can be evaluated with a fistulogram.
 Single-contrast barium enema study demonstrates sigmoid diverticulitis with fistula formation in the vagina.
Single-contrast barium enema study demonstrates sigmoid diverticulitis with fistula formation in the vagina.
Degree of confidence
Stefansson et al reported a sensitivity of 82% and a specificity of 81% for the use of barium enema in a group of 88 patients in whom diverticulitis was suspected. [16] The primary disadvantage of barium enema examination in the evaluation of diverticulitis is its limited ability in cases of extraluminal disease. Abscesses that do not communicate with the colon may not be detected. Although communication with the urinary bladder may be demonstrated, only 20% of colovesical fistulas are revealed on barium enema evaluation. Alternative conditions, such as appendicitis, epiploic appendagitis, gynecologic pathology, and renal colic, may not be depicted.
Although barium enema evaluation is excellent for differentiating diverticulitis from colon carcinoma, this differentiation is occasionally difficult. In diverticulitis, the diverticula usually are seen along with a gradual zone of transition and preservation of the mucosal folds. In carcinoma, a much sharper zone of transition is seen, with destruction of the mucosal folds. However, because diverticulosis is common, diverticula often are seen in patients with colon carcinoma. If the lesion completely obstructs the passage of contrast material during the barium enema test, the differentiation of diverticulitis from carcinoma is usually not possible.
Computed Tomography
Diverticula are identified on CT scans as outpouchings of the colonic wall. These outpouchings may contain air, barium, or fecal material. The diagnosis of diverticulitis with CT scanning is based on the detection of colonic and paracolic inflammation in the presence of underlying diverticula. [22, 23, 24]
Techniques for the CT evaluation of diverticulitis vary from institution to institution. At the authors' institution, oral contrast material is administered to opacify the small bowel. The oral contrast agent usually does not reach the sigmoid colon, but colonic opacification usually is not necessary for the evaluation of diverticulitis. [25] Occasionally, the rectal administration of contrast material may help in difficult cases.
CT with rectal contrast enhancement or CT cystography may help in diagnosing fistulas. At the authors' institution, the intravenous contrast material is administered routinely, although it usually is not essential for diagnosis. Intravenous contrast material may help in revealing diverticular abscesses and fistulas and in demonstrating the enhancement pattern of the colonic wall. However, it is probably more helpful in the diagnosis of alternative diseases that may mimic diverticulitis. [26]
(Diverticulitis-associated abscesses are presented in the images below.)
 CT scan in a patient with diverticulitis demonstrates an intramural abscess in the sigmoid colon and an abscess adjacent to the rectosigmoid that fills with contrast material.
CT scan in a patient with diverticulitis demonstrates an intramural abscess in the sigmoid colon and an abscess adjacent to the rectosigmoid that fills with contrast material.
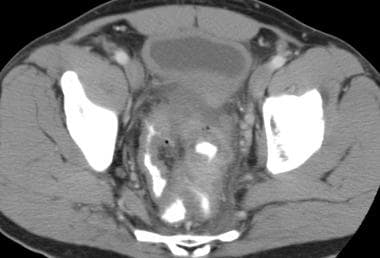 CT scan in a patient with diverticulitis demonstrates an intramural abscess in the sigmoid and an abscess adjacent to the rectosigmoid that fills with contrast material.
CT scan in a patient with diverticulitis demonstrates an intramural abscess in the sigmoid and an abscess adjacent to the rectosigmoid that fills with contrast material.
Linear stranding in the fat of the root of the sigmoid mesentery is a common finding in patients with diverticulitis. The appearance of diverticulitis may vary from minimal stranding of the mesenteric fat and small extraluminal collections of fluid or air in mild cases to extensive stranding and increased attenuation of the fat along with fistulas or large abscesses in more severe cases.
(Stranding is demonstrated in the images below.)
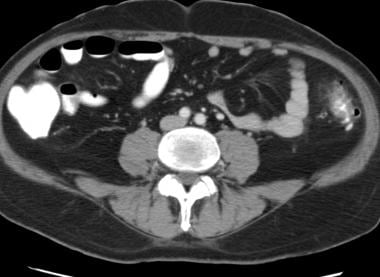 CT scan demonstrates mild diverticulitis of the descending colon, with wall thickening, a diverticulum, and mild stranding of the pericolic fat.
CT scan demonstrates mild diverticulitis of the descending colon, with wall thickening, a diverticulum, and mild stranding of the pericolic fat.
 CT scan demonstrates typical sigmoid diverticulitis with wall thickening, diverticulosis, and stranding at the root of the sigmoid mesentery.
CT scan demonstrates typical sigmoid diverticulitis with wall thickening, diverticulosis, and stranding at the root of the sigmoid mesentery.
 CT scan demonstrates typical sigmoid diverticulitis with wall thickening, diverticulosis, and stranding at the root of the sigmoid mesentery.
CT scan demonstrates typical sigmoid diverticulitis with wall thickening, diverticulosis, and stranding at the root of the sigmoid mesentery.
Symmetrical thickening of the colonic wall of approximately 4-5 mm is common. With distention, the luminal diameter of the involved segments usually measures less than 1 cm.
Enhancement of the colonic wall is commonly noted. This usually has inner and outer high-attenuation layers, with a thick middle layer of low attenuation. Small fluid collections in the colon wall may be present; they represent intramural abscesses.
Free diverticular perforation results in the extravasation of air and fluid into the pelvis and peritoneal cavity.
Peritoneal fluid containing air bubbles may be seen, often adjacent to the sigmoid colon. These findings indicate peritonitis caused by free perforation of a diverticulum.
On CT scans, fistulas and sinus tracts appear as linear or branching structures in the pericolic fat.
Fistulas may communicate with an abscess or another hollow viscus, most commonly the bladder.
Air in the bladder in the presence of a nearby segment of diverticulitis is suggestive of a colovesical fistula. If this type of fistula is suspected, the administration of rectal contrast material may be helpful. In this case, intravenous contrast agent should not be used, so that the presence of contrast enhancement in the bladder can allow definitive diagnosis of a fistulous connection. Alternatively, a CT cystogram may be obtained with the intravesical administration of contrast material via a Foley catheter, without the use of an oral or rectal contrast agent.
Rao et al described an arrowhead-shaped collection of contrast medium between thickened folds as a specific sign of diverticulitis in regions other than the cecum. [27] However, this finding was noted only in approximately one quarter of patients. The study was performed by using rectal contrast enhancement. The arrowhead sign is caused by contiguous spread of inflammation from the diverticulum to the colonic wall, resulting in a triangular space between the thickened colonic folds. This sign is seen more commonly with rectal contrast material than with oral contrast material. In the cecum, another arrowhead sign has been described as being specific for appendicitis.
Other nonspecific CT findings in diverticulitis include collections of fluid at the root of the mesocolon and engorgement of mesocolic vessels.
Degree of confidence
Cho demonstrated that CT has a sensitivity of 93% for the diagnosis of diverticulitis, which is higher than the 82% sensitivity reported for barium enema studies. [28] Often, CT is the only radiologic test needed to establish the diagnosis and to direct medical or surgical therapy or radiologic intervention. False-negative CT scans result from the difficulty in detecting early-stage diverticulitis with only minor changes in the pericolic fat.
Increased attenuation in the pericolic fat is not specific for diverticulitis, and false-positive findings occur. The differential diagnosis includes neoplasm, inflammatory bowel disease, appendicitis, and epiploic appendagitis (seen in the image below). The presence of fluid in the root of the mesentery and the engorgement of adjacent sigmoid mesenteric vasculature suggest an inflammatory process, and the absence of stranding of the pericolic fat is typical of carcinoma.
 The CT image demonstrates a pericolic fat-attenuation mass with surrounding infiltration of the fat, which is characteristic of epiploic appendagitis.
The CT image demonstrates a pericolic fat-attenuation mass with surrounding infiltration of the fat, which is characteristic of epiploic appendagitis.
Eccentric colonic wall thickening or marked concentric wall thickening is suggestive of colon carcinoma. The wall in carcinoma is frequently thicker than 2 cm, whereas it is usually thinner than 1 cm in cases of diverticulitis. Although most cases of diverticulitis involve a segment of less than 10 cm, involvement of a segment greater than 10 cm is specific for diverticulitis.
As with barium enema results, findings of overhanging edges or shoulder formation with a rigid lumen are typical of a carcinoma. The presence of pericolic lymph nodes also suggests colon cancer rather than diverticulitis. [29]
A layered pattern of enhancement of the colonic wall is typical of an inflammatory process, such as diverticulitis, and is not usually seen in carcinomas.
In some patients, distinguishing diverticulitis from colon cancer by using CT alone may not be possible, and follow-up examination after resolution of the acute episode may be necessary. Biopsy may also be required.
The presence of diverticula in the involved segment is helpful in distinguishing diverticulitis from other inflammatory conditions of the colon. Epiploic appendagitis may result from torsion of an epiploic appendage or thrombosis of an appendageal vein, and patients present with localized abdominal pain with a sudden onset. CT scans typically demonstrate an ovoid fat-attenuation mass with surrounding stranding. The colonic wall usually is not thickened. These findings help differentiate epiploic appendagitis from diverticulitis.
Ultrasonography
Ultrasonography in patients with diverticulitis is performed transabdominally with a 2- to 4-MHz convex-array transducer and compression. [30, 31, 32]
In diverticulitis, ultrasonographic findings include thickening of the bowel wall by more than 4 mm. Inflamed diverticula appear as round or ovoid, highly echogenic structures with a ring-down artifact. Inflammation of the pericolic fat is revealed as an area of increased echogenicity adjacent to the colonic wall.
Abscess formation appears as a well-defined hypoechoic mass near the colon, and it may demonstrate shadowing because of the presence of air. The absence of peristalsis is helpful for differentiating abscess from adjacent loops of bowel. Intramural sinus tracts appear as linear, echogenic foci, often with ring-down artifacts. In addition, the patient may experience pain with compression of the affected region.
According to Pradel et al, the sensitivity of ultrasonography is 85% and its specificity is 84% in the diagnosis of diverticulitis. [33] In a prospective study by Ripolles et al of 240 patients with clinical suspicion of acute colonic diverticulitis who underwent ultrasound examination, the sensitivity of US was 84% and specificity was 95.8% for diagnosing complicated ACD. Using the WSES (World Society for Emergent Surgery) classification of diverticulitis, 71 (29.6%) were stage 0, 127 (53%) were stage 1A, and 42 (17.5%) were rated moderate-to-severe (stages 1B, 2A, 2B, 3 and 4). [13]
In a retrospective study by Roson et al of 311 patients with acute diverticulitis of the left colon, the diagnosis was reached by US alone in 98 patients, by CT alone in 77, and by combined US and CT in 8. The primary reason for using CT as the first-line technique, according to the authors, was a lack of experience with abdominal ultrasonography. [14]
However, ultrasonography is operator dependent, and technologists at most centers in the United States have little experience with its use in the evaluation of diverticulitis. Ultrasonography may be totally unsuccessful, and sonograms may not show the colon in obese patients or in patients with bowel gas.
False-positive findings result from the presence of neoplasms, inflammatory or ischemic colonic diseases, and adjacent extracolonic inflammatory conditions.
-
CT scan demonstrates mild diverticulitis of the descending colon, with wall thickening, a diverticulum, and mild stranding of the pericolic fat.
-
CT scan demonstrates typical sigmoid diverticulitis with wall thickening, diverticulosis, and stranding at the root of the sigmoid mesentery.
-
CT scan demonstrates typical sigmoid diverticulitis with wall thickening, diverticulosis, and stranding at the root of the sigmoid mesentery.
-
Single-contrast barium enema study demonstrates mild sigmoid diverticulitis with thickening of the mucosal folds and luminal narrowing.
-
CT scan in a patient with diverticulitis demonstrates an intramural abscess in the sigmoid colon and an abscess adjacent to the rectosigmoid that fills with contrast material.
-
CT scan in a patient with diverticulitis demonstrates an intramural abscess in the sigmoid and an abscess adjacent to the rectosigmoid that fills with contrast material.
-
CT scan in a patient with diverticulitis demonstrates an abscess adjacent to the sigmoid colon.
-
Single-contrast barium enema study in a patient with diverticulitis demonstrates tethering of the sigmoid colon as a result of a diverticular abscess.
-
Single-contrast barium enema study in a patient with diverticulitis demonstrates an intramural abscess filling with barium.
-
Single-contrast barium enema study demonstrates sigmoid diverticulitis with a colovesical fistula.
-
Single-contrast barium enema study demonstrates sigmoid diverticulitis with a colovesical fistula. Note the contrast material in the bladder.
-
Single-contrast barium enema study demonstrates sigmoid diverticulitis with a colovesical fistula. Note the contrast material in the bladder.
-
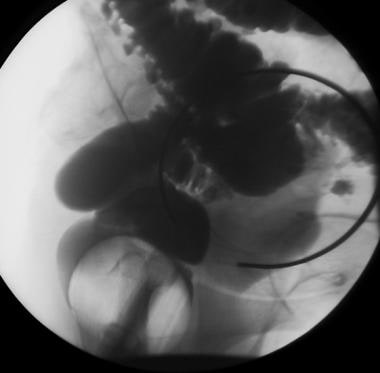
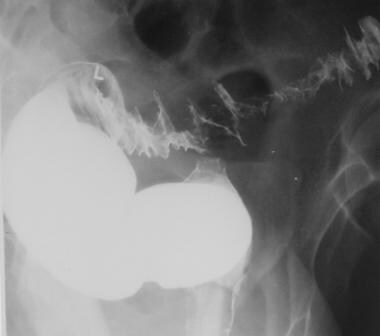
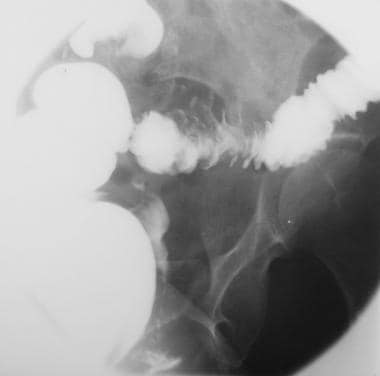
Diverticulitis with fistula in the soft tissues of the thigh. The patient presented with air in the soft tissues surrounding the hip; this was interpreted as necrotizing fasciitis. Gastrografin enema performed 8 days later demonstrated diverticulosis and extravasation from the colon into the thigh. CT scan obtained 8 days later demonstrated diverticulitis of the descending colon with extension into the soft tissues of the abdominal wall and thigh.
-
Diverticulitis with fistula in the soft tissues of the thigh (same patient as in the previous image). The patient presented with air in the soft tissues surrounding the hip; this was interpreted as necrotizing fasciitis. Gastrografin enema performed 8 days later demonstrated diverticulosis (this image) and extravasation from the colon into the thigh. CT scan obtained 8 days later demonstrated diverticulitis of the descending colon with extension into the soft tissues of the abdominal wall and thigh.
-
Diverticulitis with fistula in the soft tissues of the thigh (same patient as in previous 2 images). The patient presented with air in the soft tissues surrounding the hip; this was interpreted as necrotizing fasciitis. Gastrografin enema performed 8 days later demonstrated diverticulosis and extravasation from the colon into the thigh (this image). CT scan obtained 8 days later demonstrated diverticulitis of the descending colon with extension into the soft tissues of the abdominal wall and thigh.
-
Diverticulitis with fistula in the soft tissues of the thigh (same patient as in the previous 3 images). The patient presented with air in the soft tissues surrounding the hip; this was interpreted as necrotizing fasciitis. Gastrografin enema performed 8 days later demonstrated diverticulosis and extravasation from the colon into the thigh. CT scan obtained 8 days later (this image) demonstrated diverticulitis of the descending colon with extension into the soft tissues of the abdominal wall and thigh.
-
Diverticulitis with fistula in the soft tissues of the thigh (same patient as in the previous 4 images). The patient presented with air in the soft tissues surrounding the hip; this was interpreted as necrotizing fasciitis. Gastrografin enema examination performed 8 days later demonstrated diverticulosis and extravasation from the colon into the thigh. CT scan obtained 8 days later (this image and image immediately previous to it) demonstrated diverticulitis of the descending colon with extension into the soft tissues of the abdominal wall and thigh.
-
Single-contrast barium enema study demonstrates sigmoid diverticulitis with an intramural sinus tract. Fistula formation in the small bowel is noted.
-
Single-contrast barium enema study demonstrates diverticulitis of the descending colon with fistula formation in the small bowel.
-
Single-contrast barium enema study demonstrates sigmoid diverticulitis with fistula formation in the vagina.
-
Single-contrast barium enema study demonstrates sigmoid diverticulitis with fistula formation in the cecum.
-
CT scan demonstrates diverticulosis in a patient with colon carcinoma. Although the mass is somewhat eccentric, this type of case is difficult to differentiate from diverticulitis, and follow-up imaging is often necessary.
-
The CT image demonstrates a pericolic fat-attenuation mass with surrounding infiltration of the fat, which is characteristic of epiploic appendagitis.








