Practice Essentials
Adrenal myelolipoma is a rare benign neoplasm composed of mature adipose tissue and a variable amount of hematopoietic elements. The incidence on autopsy has been reported from 0.08-0.4%. Most lesions are small and asymptomatic. An adrenal myelolipoma is consiidered a type of adrenal incidentaloma, which is a clinically unsuspected adrenal mass discovered on imaging studies conducted for reasons other than study of the adrenal glands. [1] Most tumors are unilateral but show no predilection to one particular side. About 12% cases are bilateral. [2, 3, 4]
Myelolipomas are relatively slowly growing tumors. Tumor size varies from several millimeters to more than 30 cm. Tumors exceeding 10 cm in diameter are called giant myelolipomas, and they can become symptomatic. Symptoms may include nonspecific abdominal pain, constipation, vomiting, hematuria, or renovascular hypertension because of intratumoral hemorrhage or compression of peritumoral tissue. Acute hemorrhage, although rare, is the most significant complication, especially in large myelolipomas, and it can be manifested with pain in the back, epigastrium, or flanks and associated with nausea, vomiting, hypotension and anemia. [5, 6, 7, 8, 9, 1, 10, 11]
(Adrenal myelolipoma is shown in the images below.)
 Contrast-enhanced CT in a 64-year-old man confirms the presence of chunky calcification and a large amount of macroscopic fat in the left adrenal mass, which is diagnostic of a myelolipoma. Courtesy of P. Ramchandani, MD.
Contrast-enhanced CT in a 64-year-old man confirms the presence of chunky calcification and a large amount of macroscopic fat in the left adrenal mass, which is diagnostic of a myelolipoma. Courtesy of P. Ramchandani, MD.
 Unenhanced CT in an asymptomatic man reveals a 6-cm right adrenal mass with density measurements that range from -14 to -27 Hounsfield units, consistent with myelolipoma. Courtesy of P. Ramchandani, MD.
Unenhanced CT in an asymptomatic man reveals a 6-cm right adrenal mass with density measurements that range from -14 to -27 Hounsfield units, consistent with myelolipoma. Courtesy of P. Ramchandani, MD.
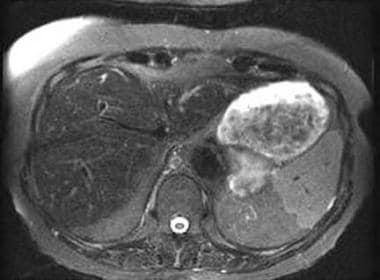
 Coronal fat-saturated gadolinium-enhanced T1-weighted gradient-echo image shows that the left adrenal myelolipoma is avascular, as reflected by its lack of enhancement. Courtesy of S. Adusumilli, MD.
Coronal fat-saturated gadolinium-enhanced T1-weighted gradient-echo image shows that the left adrenal myelolipoma is avascular, as reflected by its lack of enhancement. Courtesy of S. Adusumilli, MD.
Since myelolipomas contain different proportions of fat and myeloid tissue, a definitive diagnosis using computed tomography (CT) scanning or magnetic resonance imaging (MRI) may be difficult, although rarely so, if only a small amount of fat is present.
To distinguish the mass from a well-differentiated liposarcoma, a percutaneous fine-needle aspiration via ultrasonographic or CT guidance can confirm the diagnosis. The presence of mature adipose tissue intermixed with hematopoietic elements, including megakaryocytes on cytology or histology, is diagnostic of myelolipoma.
Yip et al in a study of 196 adrenalectomies in 192 patients found that CT or MRI characteristics predicted the presence of benign lesions with 100% specificity. Histopathology confirmed that all 66 adrenal masses with imaging characteristics suggesting benign adenoma were indeed benign lesions and included 61 benign adrenal adenomas and 5 benign nonadenomatous lesions (3 myelolipomas, 1 composite myelolipoma/adenoma, and 1 ganglioliponeuroma). The authors stated that to exclude malignancy, adrenal masses with nonbenign imaging characteristics should be resected. [12]
Lamas et al reported on 2 cases of large mixed adrenal tumors that had a heterogeneous appearance and areas of fat density on imaging and resulted in autonomous cortisol production leading to Cushing syndrome. The patients underwent adrenalectomy, and histology identified adrenocortical adenomas with widespread myelolipomatous metaplasia. The authors noted that although adrenal myelolipomas are usually asymptomatic, nonfunctioning adrenal incidentalomas, there have been a few reports of myelolipomatous masses that are associated with adrenocortical hypersecretion. [13]
Montone et al presented pathologic and radiographic features of 3 patients with adrenocortical neoplasms. Two patients had imaging findings that were compatible with adrenal myelolipoma. Pathologically, 2 of the lesions were classified as adrenocortical neoplasms of uncertain malignant potential, and 1 lesion was classified as an adrenocortical adenoma. All 3 lesions contained myelolipomatous foci throughout the neoplasm, and 2 of the tumors contained several pure lipomatous foci. The authors noted that imaging studies may result in a false diagnosis of a benign adrenal myelolipoma and, as a result, undertreatment. [14]
Preferred examination
Adrenal myelolipomas can be diagnosed in 90% of cases by ultrasonography, CT, and magnetic resonance imaging. The fatty component of a myelolipoma is macroscopic in most patients and is diagnostic when discovered on cross-sectional imaging. [2, 15, 16, 17, 4, 6, 1]
The preferred imaging modality is CT, which shows focal fatty density within the mass. MRI also accurately depicts both microscopic and macroscopic fat using chemical shift imaging and explicit fat saturation technique, respectively. Myelolipomas may be discovered incidentally on ultrasonography (US), which otherwise is not used routinely to characterize adrenal neoplasms. [18]
Occasionally, myelolipomas can enlarge enough to make the organ of origin difficult to discern on CT, resulting in a differential diagnosis that includes renal angiomyolipoma and retroperitoneal liposarcoma or lipoma. In these patients, the multiplanar capability of MRI can help define the tissue planes and confirm that the mass is adrenal in origin.
On ultrasonography the appearance of an adrenal myelolipoma can be hyperechoic or hypoechoic, depending on the predominance of fat or myeloid cells. Retroperitoneal fat–containing tumors such as teratoma, lipoma, myolipoma, angiomyolipoma, and liposarcoma may mimic adrenal myelolipoma radiologically. Some myelolipomas may have a larger amount of hematopoietic tissue and no recognizable fat, making them impossible to distinguish from well-differentiated retroperitoneal malignancies or other adrenal tumors on CT or MRI. Percutaneous biopsy may be necessary to establish a diagnosis. [2, 15, 4, 6]
Incidental findings algorithm
The American College of Radiology (ACR) has published an algorithm applied to incidental adrenal masses in asymptomatic adult patients (≥18 years of age) referred to imaging for a reason that is unrelated to potential adrenal pathology. This algorithm can be applied to patients with bilateral adrenal masses, with each lesion assessed separately. The basic principles of the algorithm are as follows [19] :
-
In general, an incidental adrenal mass < 1 cm in the short axis need not be pursued. If an adrenal mass has diagnostic features of a myelolipoma (presence of macroscopic fat), no additional workup or follow-up imaging is needed.
-
Incidental masses are primarily categorized by the presence of diagnostic imaging features, adrenal mass size, growth (the determination of which requires the availability of prior imaging), and cancer history.
-
To determine whether an adrenal mass that is ≥1 to < 4 cm and >10 HU qualifies as a benign adenoma, a dedicated adrenal CT protocol is the imaging examination of choice because it permits such characterization using both density measurement and contrast washout.
-
Radiologists should refer to available prior imaging examinations whenever possible to determine the stability of an adrenal mass. Even if not of the same examination type, prior imaging studies that include the adrenal glands (ie, chest CT, PET/CT, abdominal ultrasound, or lumbar spine MRI) can be helpful.
-
Clinical context is a crucial factor for adrenal mass management. Workup of an incidental adrenal mass in a patient unable to receive treatment, or who has serious comorbidities and limited life expectancy, may be unnecessary.
Radiography
If large enough, a suprarenal mass may cause inferior displacement of the kidney. The mass may be radiolucent if it is predominantly fatty and, occasionally, can contain calcifications. Plain radiographs are nonspecific and not part of the imaging workup of these lesions. Perform cross-sectional imaging using CT or MRI to document the presence of fat. Smaller myelolipomas are unlikely to exert enough mass effect to be visible on conventional radiographs, thereby constituting false-negative results. Similarly, inferior displacement of the kidney on radiographs can be a result of other adrenal or extra-adrenal lesions. [20, 21, 22, 23, 24, 25]
(See the images below.)
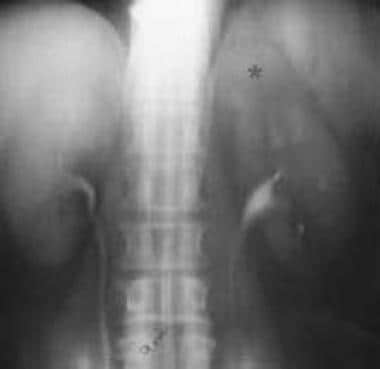
 Intravenous urogram performed in a 64-year-old man reveals inferior displacement of the left kidney by a left suprarenal mass containing a large focus of calcification (indicated by *). Courtesy of P. Ramchandani, MD.
Intravenous urogram performed in a 64-year-old man reveals inferior displacement of the left kidney by a left suprarenal mass containing a large focus of calcification (indicated by *). Courtesy of P. Ramchandani, MD.
 Intravenous urogram performed in a 63-year-old man reveals a round left suprarenal mass (indicated by *) without mass effect on the left kidney. Courtesy of P. Ramchandani, MD.
Intravenous urogram performed in a 63-year-old man reveals a round left suprarenal mass (indicated by *) without mass effect on the left kidney. Courtesy of P. Ramchandani, MD.
Computed Tomography
CT is sensitive in depicting macroscopic fat in myelolipomas. The key to a CT diagnosis is to find a true focal fat collection in the adrenal mass. This modality is specific and diagnostic if the focal fat density is revealed. CT appearance of myelolipomas depends on their histologic composition. Large amounts of fat often are seen interspersed with higher-attenuation myeloid tissue. The attenuation values are low (-20 to -30 Hounsfield units [HU]), reflecting the mixture of adipose and myeloid elements. The density of the mass may be slightly higher than that of the adjacent retroperitoneal fat secondary to the presence of the myeloid tissue. [26, 27, 28, 29, 30, 31, 32, 33, 34, 15]
In almost all myelolipomas, some regions have densities of less than -30 HU and as low as -100 HU. If the mass contains more hematopoietic tissue, it may appear more heterogeneous and mimic a retroperitoneal liposarcoma. A definitive diagnosis requires percutaneous-guided cytologic or histologic sampling.
The masses usually have a recognizable capsule and may contain calcification in as many as 20% of patients. Calcification may be related to previous hemorrhage. After contrast administration, the mass enhances. [35] If intratumoral or peritumoral hemorrhage has occurred, high-attenuation or low-attenuation fluid may be present, depending on the age of the blood.
CT can be problematic if the mass is large and the organ of origin is not obvious using axial imaging. MRI may be warranted for further evaluation as a result of its multiplanar capability. Additionally, if little or no macroscopic fat is present, the lesion has soft tissue attenuation.
(Below are CT images of adrenal myelolipomas.)
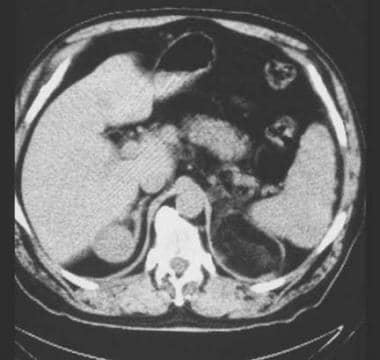
 Contrast-enhanced CT in a 64-year-old man confirms the presence of chunky calcification and a large amount of macroscopic fat in the left adrenal mass, which is diagnostic of a myelolipoma. Courtesy of P. Ramchandani, MD.
Contrast-enhanced CT in a 64-year-old man confirms the presence of chunky calcification and a large amount of macroscopic fat in the left adrenal mass, which is diagnostic of a myelolipoma. Courtesy of P. Ramchandani, MD.
 Contrast-enhanced CT in a 63-year-old man reveals several scattered foci of macroscopic fat in the left adrenal mass, confirming a diagnosis of myelolipoma. Courtesy of P. Ramchandani, MD.
Contrast-enhanced CT in a 63-year-old man reveals several scattered foci of macroscopic fat in the left adrenal mass, confirming a diagnosis of myelolipoma. Courtesy of P. Ramchandani, MD.
 Contrast-enhanced CT in a 72-year-old woman reveals a 6-cm right adrenal mass containing large amounts of macroscopic fat, consistent with an adrenal myelolipoma. The attenuation of the fat is slightly higher than that of the adjacent retroperitoneal fat, likely as a result of the presence of hematopoietic elements in the mass. Courtesy of P. Ramchandani, MD.
Contrast-enhanced CT in a 72-year-old woman reveals a 6-cm right adrenal mass containing large amounts of macroscopic fat, consistent with an adrenal myelolipoma. The attenuation of the fat is slightly higher than that of the adjacent retroperitoneal fat, likely as a result of the presence of hematopoietic elements in the mass. Courtesy of P. Ramchandani, MD.
 Unenhanced CT in an asymptomatic man reveals a 6-cm right adrenal mass with density measurements that range from -14 to -27 Hounsfield units, consistent with myelolipoma. Courtesy of P. Ramchandani, MD.
Unenhanced CT in an asymptomatic man reveals a 6-cm right adrenal mass with density measurements that range from -14 to -27 Hounsfield units, consistent with myelolipoma. Courtesy of P. Ramchandani, MD.
 Contrast-enhanced CT reveals a left adrenal mass with a large deposit of macroscopic fat, measuring -97 Hounsfield units, diagnostic of adrenal myelolipoma.
Contrast-enhanced CT reveals a left adrenal mass with a large deposit of macroscopic fat, measuring -97 Hounsfield units, diagnostic of adrenal myelolipoma.
Magnetic Resonance Imaging
The fat in an adrenal myelolipoma is of high signal intensity on T1- and T2-weighted sequences and is key to diagnosis. The hematopoietic tissue has low signal intensity on T1-weighted images and moderate signal intensity on T2-weighted images. The nonuniform admixture of fat and marrow elements also may result in a heterogeneous appearance on T2-weighted sequences. [27, 36, 37, 38, 39, 40, 41]
Explicit (chemical) fat-suppressed T1-weighted sequences show a focal loss of signal intensity in the fatty part of the mass, which confirms the diagnosis. The presence of myeloid tissue or hemorrhage results in persistent areas of increased signal intensity on fat-suppressed images. A water-saturated T1-weighted sequence shows the fat as high signal intensity on a background of low signal intensity.
Chemical shift gradient-echo imaging depicts microscopic (intracellular) fat that is contained in the same voxel as a water proton. Two scans are obtained through the mass using parameters that are identical except for the echo time (TE), which is selected so that the fat and water protons are either in phase or out of phase. Out-of-phase images show signal loss, since the fat and water protons in the same voxel cancel each other out. This decrease in signal intensity indicates the presence of microscopic fat. Adrenal myelolipomas enhance after gadolinium administration as a result of the presence of hematopoietic tissue.
Elsayes et al described 3 categories of myelolipomas based on their MRI features. [42] These categories are (1) homogeneous, hyperintense masses on T1-weighted imaging indicating that they are composed mainly of fat; (2) heterogeneous masses composed of an admixture of fatty and myeloid elements; and (3) focal enhancing masslike areas composed mainly of myeloid cells.
(MRI images are provided below that depict adrenal myelolipomas.)
 A 70-year-old asymptomatic man with a left adrenal myelolipoma noted incidentally. Axial T1-weighted in-phase gradient-echo image reveals a left adrenal soft tissue mass with 2 small foci of high signal intensity in the posterior aspect of the mass, which can represent hemorrhage or fat. Courtesy of S. Adusumilli, MD.
A 70-year-old asymptomatic man with a left adrenal myelolipoma noted incidentally. Axial T1-weighted in-phase gradient-echo image reveals a left adrenal soft tissue mass with 2 small foci of high signal intensity in the posterior aspect of the mass, which can represent hemorrhage or fat. Courtesy of S. Adusumilli, MD.
 Axial T1-weighted out-of-phase gradient-echo image. Overall, the mass demonstrates slight loss of signal intensity with respect to the spleen, reflecting the presence of intracellular lipid. The 2 foci of high signal intensity in the posterior aspect of the mass do not lose signal, since they represent macroscopic fat. Courtesy of S. Adusumilli, MD.
Axial T1-weighted out-of-phase gradient-echo image. Overall, the mass demonstrates slight loss of signal intensity with respect to the spleen, reflecting the presence of intracellular lipid. The 2 foci of high signal intensity in the posterior aspect of the mass do not lose signal, since they represent macroscopic fat. Courtesy of S. Adusumilli, MD.
 Axial T1-weighted out-of-phase gradient-echo image with explicit fat saturation. The 2 foci of high signal intensity in the posterior aspect of the mass have completely lost signal because of the fat saturation technique. The loss of signal intensity also proves that these foci do not represent hemorrhage, which remains high in signal intensity. Courtesy of S. Adusumilli, MD.
Axial T1-weighted out-of-phase gradient-echo image with explicit fat saturation. The 2 foci of high signal intensity in the posterior aspect of the mass have completely lost signal because of the fat saturation technique. The loss of signal intensity also proves that these foci do not represent hemorrhage, which remains high in signal intensity. Courtesy of S. Adusumilli, MD.
 Axial fat-saturated T2-weighted fast spin-echo. The left adrenal mass is minimally heterogeneous as a result of the presence of hematopoietic tissue. The 2 foci of dark signal intensity in the posterior aspect of the mass represent macroscopic fat, since an explicit fat saturation technique was used. Courtesy of S. Adusumilli, MD.
Axial fat-saturated T2-weighted fast spin-echo. The left adrenal mass is minimally heterogeneous as a result of the presence of hematopoietic tissue. The 2 foci of dark signal intensity in the posterior aspect of the mass represent macroscopic fat, since an explicit fat saturation technique was used. Courtesy of S. Adusumilli, MD.
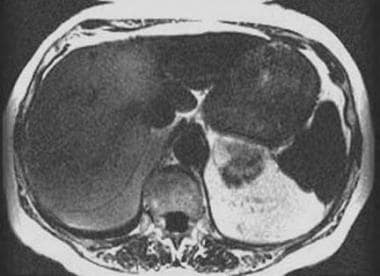
 An 87-year-old woman with a left adrenal myelolipoma. Axial T1-weighted in-phase gradient-echo image reveals a heterogeneous left adrenal mass with a discrete area of high signal intensity in the anterior medial aspect of the mass, which can represent fat or hemorrhage. Courtesy of S. Adusumilli, MD.
An 87-year-old woman with a left adrenal myelolipoma. Axial T1-weighted in-phase gradient-echo image reveals a heterogeneous left adrenal mass with a discrete area of high signal intensity in the anterior medial aspect of the mass, which can represent fat or hemorrhage. Courtesy of S. Adusumilli, MD.
 Axial T1-weighted out-of-phase gradient-echo shows that most of the mass loses signal intensity with respect to the spleen, which is consistent with intracellular or microscopic lipid. A persistent area of high signal intensity is seen in the anterior medial aspect of the mass, which can represent either macroscopic fat or hemorrhage. Courtesy of S. Adusumilli, MD.
Axial T1-weighted out-of-phase gradient-echo shows that most of the mass loses signal intensity with respect to the spleen, which is consistent with intracellular or microscopic lipid. A persistent area of high signal intensity is seen in the anterior medial aspect of the mass, which can represent either macroscopic fat or hemorrhage. Courtesy of S. Adusumilli, MD.
 Axial T1-weighted in-phase gradient-echo image with water saturation. This water saturation sequence detects macroscopic fat that remains high in signal intensity, while the rest of the abdominal structures lose signal intensity, since they contain water protons. A part of the left adrenal mass loses signal intensity as a result of the presence of hematopoietic tissue; however, a persistent focus of high signal intensity is seen in the anterior medial aspect of the mass, which represents macroscopic fat. Courtesy of S. Adusumilli, MD.
Axial T1-weighted in-phase gradient-echo image with water saturation. This water saturation sequence detects macroscopic fat that remains high in signal intensity, while the rest of the abdominal structures lose signal intensity, since they contain water protons. A part of the left adrenal mass loses signal intensity as a result of the presence of hematopoietic tissue; however, a persistent focus of high signal intensity is seen in the anterior medial aspect of the mass, which represents macroscopic fat. Courtesy of S. Adusumilli, MD.
 Axial T1-weighted gradient-echo image with explicit fat saturation demonstrates that the entire mass loses signal intensity, which is reflective of the presence of macroscopic fat throughout the mass. Courtesy of S. Adusumilli, MD.
Axial T1-weighted gradient-echo image with explicit fat saturation demonstrates that the entire mass loses signal intensity, which is reflective of the presence of macroscopic fat throughout the mass. Courtesy of S. Adusumilli, MD.
 Axial fat-saturated T2-weighted fast spin-echo image shows areas of brighter signal intensity in the mass that reflects the presence of hematopoietic tissue. Courtesy of S. Adusumilli, MD.
Axial fat-saturated T2-weighted fast spin-echo image shows areas of brighter signal intensity in the mass that reflects the presence of hematopoietic tissue. Courtesy of S. Adusumilli, MD.
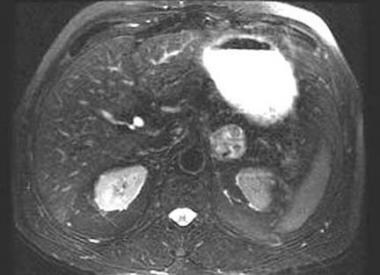
 Coronal fat-saturated gadolinium-enhanced T1-weighted gradient-echo image shows that the left adrenal myelolipoma is avascular, as reflected by its lack of enhancement. Courtesy of S. Adusumilli, MD.
Coronal fat-saturated gadolinium-enhanced T1-weighted gradient-echo image shows that the left adrenal myelolipoma is avascular, as reflected by its lack of enhancement. Courtesy of S. Adusumilli, MD.
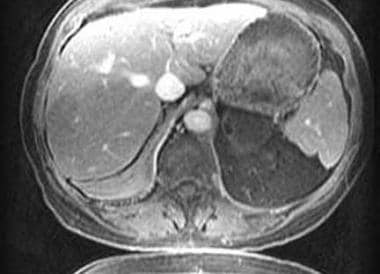 Axial fat-saturated gadolinium-enhanced T1-weighted gradient-echo image shows low signal intensity (reflecting the presence of macroscopic fat) and lack of contrast enhancement in the left adrenal myelolipoma. Courtesy of S. Adusumilli, MD.
Axial fat-saturated gadolinium-enhanced T1-weighted gradient-echo image shows low signal intensity (reflecting the presence of macroscopic fat) and lack of contrast enhancement in the left adrenal myelolipoma. Courtesy of S. Adusumilli, MD.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Degree of confidence
MRI is as sensitive and specific as CT in depicting macroscopic fat and confirming the diagnosis. In evaluating an adrenal myelolipoma, explicit (chemically selective) fat saturation sequences show more signal loss than chemical shift imaging, since the presence of macroscopic fat is typical of a myelolipoma. In contrast, a lipid-rich adrenal adenoma would reveal greater loss of signal intensity on chemical shift imaging, as it contains intracellular (microscopic) fat. An added advantage of MRI is the ability to image directly in the coronal and sagittal planes, confirming that the origin of a large mass is adrenal and not hepatic or renal.
Lesions such as adrenal adenomas, metastases, and primary cortical carcinomas rarely have been reported to contain focal fat and can be misdiagnosed as myelolipoma. However, these lesions are rare enough that the detection of macroscopic fat should not prevent the diagnosis in almost all patients. Conversely, some adrenal myelolipomas (eg, giant myelolipomas) have been shown to contain minimal fat, resulting in difficulty in making a definitive diagnosis by MRI. As with CT, markedly heterogeneous masses may not be distinguished easily from well-differentiated retroperitoneal malignancies, such as liposarcoma, and require tissue sampling for definitive diagnosis.
Ultrasonography
Sonographic appearance varies with the composition of the neoplasm. If the tumor contains predominantly fatty components, it appears uniformly hyperechoic. If the tumor contains a predominance of myeloid cells, it may appear heterogeneous or hypoechoic. [43, 44]
The classic appearance is an echogenic suprarenal mass, which suggests the diagnosis. The ipsilateral hemidiaphragm artifactually appears as a disrupted line, a finding unique to fat-containing masses. The margins of the lesion are difficult to define because of the lack of contrast with the adjacent retroperitoneal fat.
Although a predominantly hyperechoic adrenal mass strongly suggests the diagnosis of myelolipoma, US is not as specific as CT or MRI, either of which should be obtained for further evaluation. US is more nonspecific if the tumor contains only a small quantity of fat and appears hypoechoic, thus mimicking other benign or malignant adrenal neoplasms.
Small lesions are more difficult to diagnose by US, since they may be masked by adjacent echogenic retroperitoneal fat. The finding of apparent disruption of the diaphragmatic echoes is appreciated only for tumors larger than 4 cm; however, the absence of this finding does not mean that a hyperechoic mass does not contain fat.
Lesions containing a predominance of myeloid cells appear more hypoechoic and mimic an adenoma, hematoma, metastasis, or primary cortical carcinoma. The presence of hemorrhage or calcification within the tumor alters the sonographic appearance and further confounds the issue.
Angiography
As a result of vascular specificity, an angiogram can confirm that a mass is adrenal in origin rather than arising from the liver or kidney. The mass is predominantly avascular, with a peripheral rim of vascularity from branching vessels. [45]
The procedure is fairly specific in determining the organ of mass's origin but is otherwise nonspecific regarding its tissue characteristic. With the advent of cross-sectional imaging modalities, little indication exists for routine angiography.
Other adrenal masses, such as adenomas, lipomas, cysts, and metastases, can have a similar angiographic appearance.
-
Contrast-enhanced CT in a 64-year-old man confirms the presence of chunky calcification and a large amount of macroscopic fat in the left adrenal mass, which is diagnostic of a myelolipoma. Courtesy of P. Ramchandani, MD.
-
Intravenous urogram performed in a 64-year-old man reveals inferior displacement of the left kidney by a left suprarenal mass containing a large focus of calcification (indicated by *). Courtesy of P. Ramchandani, MD.
-
Intravenous urogram performed in a 63-year-old man reveals a round left suprarenal mass (indicated by *) without mass effect on the left kidney. Courtesy of P. Ramchandani, MD.
-
Contrast-enhanced CT in a 63-year-old man reveals several scattered foci of macroscopic fat in the left adrenal mass, confirming a diagnosis of myelolipoma. Courtesy of P. Ramchandani, MD.
-
Contrast-enhanced CT in a 72-year-old woman reveals a 6-cm right adrenal mass containing large amounts of macroscopic fat, consistent with an adrenal myelolipoma. The attenuation of the fat is slightly higher than that of the adjacent retroperitoneal fat, likely as a result of the presence of hematopoietic elements in the mass. Courtesy of P. Ramchandani, MD.
-
Unenhanced CT in an asymptomatic man reveals a 6-cm right adrenal mass with density measurements that range from -14 to -27 Hounsfield units, consistent with myelolipoma. Courtesy of P. Ramchandani, MD.
-
Contrast-enhanced CT reveals a left adrenal mass with a large deposit of macroscopic fat, measuring -97 Hounsfield units, diagnostic of adrenal myelolipoma.
-
An inferior axial image shows areas of soft tissue density and discrete foci of macroscopic fat, measuring approximately -90 Hounsfield units. Courtesy of P. Ramchandani, MD.
-
A 70-year-old asymptomatic man with a left adrenal myelolipoma noted incidentally. Axial T1-weighted in-phase gradient-echo image reveals a left adrenal soft tissue mass with 2 small foci of high signal intensity in the posterior aspect of the mass, which can represent hemorrhage or fat. Courtesy of S. Adusumilli, MD.
-
Axial T1-weighted out-of-phase gradient-echo image. Overall, the mass demonstrates slight loss of signal intensity with respect to the spleen, reflecting the presence of intracellular lipid. The 2 foci of high signal intensity in the posterior aspect of the mass do not lose signal, since they represent macroscopic fat. Courtesy of S. Adusumilli, MD.
-
Axial T1-weighted out-of-phase gradient-echo image with explicit fat saturation. The 2 foci of high signal intensity in the posterior aspect of the mass have completely lost signal because of the fat saturation technique. The loss of signal intensity also proves that these foci do not represent hemorrhage, which remains high in signal intensity. Courtesy of S. Adusumilli, MD.
-
Axial fat-saturated T2-weighted fast spin-echo. The left adrenal mass is minimally heterogeneous as a result of the presence of hematopoietic tissue. The 2 foci of dark signal intensity in the posterior aspect of the mass represent macroscopic fat, since an explicit fat saturation technique was used. Courtesy of S. Adusumilli, MD.
-
An 87-year-old woman with a left adrenal myelolipoma. Axial T1-weighted in-phase gradient-echo image reveals a heterogeneous left adrenal mass with a discrete area of high signal intensity in the anterior medial aspect of the mass, which can represent fat or hemorrhage. Courtesy of S. Adusumilli, MD.
-
Axial T1-weighted out-of-phase gradient-echo shows that most of the mass loses signal intensity with respect to the spleen, which is consistent with intracellular or microscopic lipid. A persistent area of high signal intensity is seen in the anterior medial aspect of the mass, which can represent either macroscopic fat or hemorrhage. Courtesy of S. Adusumilli, MD.
-
Axial T1-weighted in-phase gradient-echo image with water saturation. This water saturation sequence detects macroscopic fat that remains high in signal intensity, while the rest of the abdominal structures lose signal intensity, since they contain water protons. A part of the left adrenal mass loses signal intensity as a result of the presence of hematopoietic tissue; however, a persistent focus of high signal intensity is seen in the anterior medial aspect of the mass, which represents macroscopic fat. Courtesy of S. Adusumilli, MD.
-
Axial T1-weighted gradient-echo image with explicit fat saturation demonstrates that the entire mass loses signal intensity, which is reflective of the presence of macroscopic fat throughout the mass. Courtesy of S. Adusumilli, MD.
-
Axial fat-saturated T2-weighted fast spin-echo image shows areas of brighter signal intensity in the mass that reflects the presence of hematopoietic tissue. Courtesy of S. Adusumilli, MD.
-
Coronal fat-saturated gadolinium-enhanced T1-weighted gradient-echo image shows that the left adrenal myelolipoma is avascular, as reflected by its lack of enhancement. Courtesy of S. Adusumilli, MD.
-
Axial fat-saturated gadolinium-enhanced T1-weighted gradient-echo image shows low signal intensity (reflecting the presence of macroscopic fat) and lack of contrast enhancement in the left adrenal myelolipoma. Courtesy of S. Adusumilli, MD.









