Practice Essentials
Chondrosarcoma is the second most frequent primary malignant tumor of bone, representing approximately 20-25% of all primary osseous neoplasms. Chondrosarcomas are a group of tumors with highly diverse features and behavior patterns, ranging from slow-growing nonmetastasizing lesions to highly aggressive metastasizing sarcomas. [1, 2, 3, 4] The pelvis and proximal femur are the most common sites. [5, 6, 7, 8, 9]
Primary (conventional) chondrosarcomas (85-90%) occur in preexisting normal bone, whereas secondary tumors occur in preexisting enchondromas and osteochondromas. Primary chondrosarcomas are divided into central, periosteal, and peripheral types. Secondary chondrosarcomas include clear cell, mesenchymal, and dedifferentiated chondrosarcomas. [7]
Chondrosarcomas typically present in adults during the fifth to seventh decades and are rare in young patients. Less than 7% of chondrosarcomas occur in patients younger than 21 years. [10]
(See the image below.)
 Frontal radiograph of the left fibula head demonstrates a lucent lesion that contains the typical chondroid matrix calcification. Low-grade tumor.
Frontal radiograph of the left fibula head demonstrates a lucent lesion that contains the typical chondroid matrix calcification. Low-grade tumor.
Imaging modalities
Radiographs are essential for the initial diagnosis of chondrosarcoma; radiography is sometimes supplemented with computed tomography (CT) scanning, which is more sensitive for detecting matrix calcification and for confirming deep endosteal cortical scalloping in intramedullary tumors. Magnetic resonance imaging (MRI) is the preferred modality for evaluating the extent of intramedullary tumors and for demonstrating extraosseous extension. MRI is useful in evaluating the thickened cartilage cap in an osteochondroma in which a secondary chondrosarcoma develops. MRI is less sensitive than CT in identifying small amounts of matrix calcification within a tumor. [11, 12, 13, 14, 15]
The imaging appearances of chondrosarcoma may overlap with those of other lesions, especially other cartilaginous tumors such as enchondroma. The presence of pain with any lesion (without a pathologic fracture in lesions of the hands and feet) is highly suggestive of malignancy.
Other findings suggestive of malignancy in a cartilaginous tumor include endosteal cortical scalloping of more than two thirds of the thickness of the cortex, ill-defined border and/or zone of transition, and a large soft-tissue mass. Both benign and malignant cartilaginous tumors may show central lucency; however, lucency of an area that previously showed matrix calcification is highly suggestive of chondrosarcoma.
Ultrasonography has no role in the evaluation of intramedullary lesions confined to the bone. It may demonstrate soft-tissue extension; therefore, it may be useful in guiding percutaneous biopsy. Ultrasonography is useful as a means of assessing the thickness of the cartilage cap overlying an osteochondroma, although access to the lesion may be difficult in certain areas. If the cap measures more than 1.5 cm in a skeletally mature patient, transformation to chondrosarcoma may have occurred.
Guidelines
Both the National Comprehensive Cancer Network (NCCN) guidelines and the American College of Radiology (ACR) Appropriateness Criteria recommend radiographs for the initial imaging of suspected primary bone tumors. [5, 16] Following abnormal radiography findings, NCCN recommends patients younger than 40 years be referred to an orthopedic oncologist; patients 40 years of age or older should receive a workup for potential bone metastasis, which includes bone scans, chest ra.diographs, chest/abdominal/pelvic CT with contrast, and mammography. [5]
The ACR Appropriateness Criteria includes the the following recommendations for second-line imaging on the basis of radiographic findings [16] :
-
MRI with or without contrast in cases of negative findings or findings that do not explain symptoms.
-
MRI with or without contrast in cases of lesions with intermediate or aggressive appearance for malignancy.
Staging
The Enneking staging system for musculoskeletal sarcomas is applicable to chondrosarcomas, as follows [17] :
-
Stage I (low-grade tumor) - Stage I-A, intracompartmental; stage I-B, extracompartmental
-
Stage II (high-grade tumor) - Stage II-A, intracompartmental; stage II-B, extracompartmental
-
Stage III (distant metastasis)
Radiography
Radiographs typically show a lucent lesion, which frequently contains matrix calcification, particularly in well-differentiated tumors. The degree of organization of the matrix calcification may be correlated with the grade of the tumor. Aggressive tumors contain irregular calcifications, and they often have large areas showing no calcification at all. Well-differentiated lesions tend to have more developed matrix; the typical appearance is of rings and arcs. [13] Radiographs alone are often inadequate for assessing the size of the tumor; MRI is useful for demonstrating both the intramedullary extension and the soft-tissue extension of the lesion. CT scanning may be helpful in identifying matrix calcification in some lesions that appear entirely lucent on radiographs.
(See the images below.)
 Frontal radiograph of the left fibula head demonstrates a lucent lesion that contains the typical chondroid matrix calcification. Low-grade tumor.
Frontal radiograph of the left fibula head demonstrates a lucent lesion that contains the typical chondroid matrix calcification. Low-grade tumor.
 Frontal radiograph of the left acetabulum demonstrates an expansile lucent lesion with no internal matrix calcification. Low-grade central tumor.
Frontal radiograph of the left acetabulum demonstrates an expansile lucent lesion with no internal matrix calcification. Low-grade central tumor.
 Frontal radiograph of right side of upper abdomen demonstrates a destructive, expansile lesion of the 12th rib. The lesion contains irregular calcification. High-grade central tumor.
Frontal radiograph of right side of upper abdomen demonstrates a destructive, expansile lesion of the 12th rib. The lesion contains irregular calcification. High-grade central tumor.
 Frontal radiograph of the pelvis demonstrates extensive calcification overlying the left ilium and in the lateral soft tissues. No bone destruction is shown. High-grade secondary peripheral tumor.
Frontal radiograph of the pelvis demonstrates extensive calcification overlying the left ilium and in the lateral soft tissues. No bone destruction is shown. High-grade secondary peripheral tumor.
 Lateral radiograph of the distal femur in a patient with hereditary multiple exostoses. Several osteochondromas of varying appearances arise from the metaphyseal region; these typically grow away from the joint. Soft-tissue calcification is shown overlying the most posterior osteochondroma. High-grade secondary peripheral tumor.
Lateral radiograph of the distal femur in a patient with hereditary multiple exostoses. Several osteochondromas of varying appearances arise from the metaphyseal region; these typically grow away from the joint. Soft-tissue calcification is shown overlying the most posterior osteochondroma. High-grade secondary peripheral tumor.
The margin of intramedullary lesions is determined by the degree of aggression of the tumor. It is frequently ill defined. Endosteal scalloping may be present; when its depth is more than two thirds the normal thickness of the cortex, this scalloping is useful in distinguishing chondrosarcoma from enchondroma, except in lesions of the hands and feet. Benign enchondromas in these areas may cause considerable cortical thinning; such enchondromas may occur as a pathologic fracture.
The presence of cortical destruction or a soft-tissue mass is indicative of malignancy. Destruction of matrix calcification that was previously visible in an enchondroma is indicative of malignant transformation.
Computed Tomography
In as many as 90% of cases, tumors appear as lucent areas containing chondroid matrix calcification. Endosteal scalloping and cortical destruction are frequently easier to appreciate on CT scans than on radiographs. [11, 15] CT scanning may be used to guide percutaneous biopsy, and it is the modality of choice for investigating possible pulmonary metastatic disease. CT scanning may often be used to successfully categorize the lesion as being of cartilaginous origin. The medullary extension of the lesion may be assessed more accurately with CT than with radiography. However, MRI is superior, and it is also the most useful modality for determining soft-tissue extension.
(See the images below.)
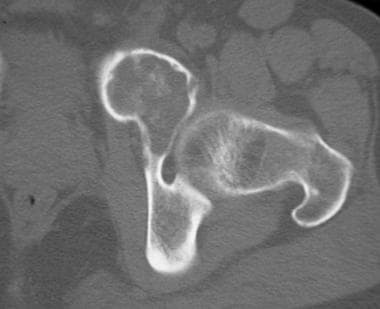 Bone-window CT scan of left acetabulum demonstrates matrix calcification in the expansile lucent lesion in the anterior column. Low-grade central tumor.
Bone-window CT scan of left acetabulum demonstrates matrix calcification in the expansile lucent lesion in the anterior column. Low-grade central tumor.
 CT of the right side of the upper abdomen demonstrates the expansile tumor with a large, associated soft-tissue mass containing foci of calcification. High-grade central tumor.
CT of the right side of the upper abdomen demonstrates the expansile tumor with a large, associated soft-tissue mass containing foci of calcification. High-grade central tumor.
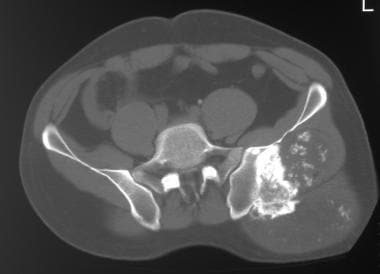 CT scan of the pelvis demonstrates a large soft-tissue mass that contains calcification arising from a broad-based sessile osteochondroma on the posterior aspect of the ilium. High-grade secondary peripheral tumor.
CT scan of the pelvis demonstrates a large soft-tissue mass that contains calcification arising from a broad-based sessile osteochondroma on the posterior aspect of the ilium. High-grade secondary peripheral tumor.
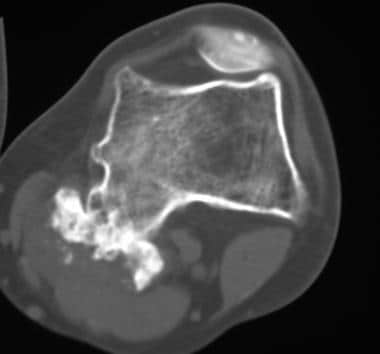 CT scan of the distal femur demonstrates a broad-based osteochondroma with a thick overlying soft-tissue cap that contains focal calcification. The metaphyseal contour is irregular because of the presence of several other osteochondromas in this patient with hereditary multiple exostoses. High-grade secondary peripheral tumor.
CT scan of the distal femur demonstrates a broad-based osteochondroma with a thick overlying soft-tissue cap that contains focal calcification. The metaphyseal contour is irregular because of the presence of several other osteochondromas in this patient with hereditary multiple exostoses. High-grade secondary peripheral tumor.
Magnetic Resonance Imaging
MRI typically demonstrates lobulated lesions of high signal intensity on T2-weighted images. Lobules are commonly separated by septa of low signal intensity. On T1-weighted images, the lesion generally displays low signal intensity. [12, 13, 14, 15] MRI is the method of choice for clarifying the intramedullary and extraosseous extension of a chondrosarcoma; features related to cortical bone and matrix calcification are more accurately assessed with CT.
Areas of matrix calcification are shown as signal voids on images obtained with all sequences, but small amounts of calcification may not be identifiable. MRI may demonstrate large aggregates of calcium, but tiny scattered calcifications may be completely missed because of partial-volume averaging. MRI may be used to assess soft-tissue extension and the intramedullary extent of the tumor. MRIs may demonstrate endosteal cortical scalloping, but this feature is more easily assessed with CT.
MRI is useful in assessing the thickness of the cartilage cap of osteochondromas to identify chondrosarcoma transformation. Chondrosarcomas show variable patterns of enhancement after the administration of contrast material.
(See the images below.)
 T2-weighted axial MRI of the pelvis demonstrates the high signal intensity of the acetabular lesion. Low-grade central tumor.
T2-weighted axial MRI of the pelvis demonstrates the high signal intensity of the acetabular lesion. Low-grade central tumor.
 T1-weighted axial MRI of the pelvis demonstrates the low signal intensity of the acetabular lesion. Low-grade central tumor.
T1-weighted axial MRI of the pelvis demonstrates the low signal intensity of the acetabular lesion. Low-grade central tumor.
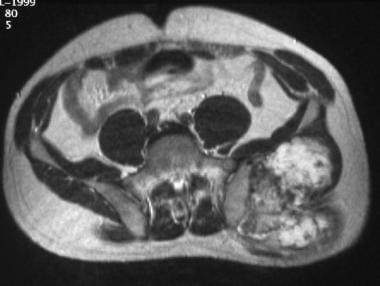 T2-weighted axial MRI of the pelvis demonstrates a lobulated high-signal-intensity soft tissue with local-signal-intensity septa arising from the osteochondroma on the posterior aspect of the ilium. Several areas of low signal intensity are shown; these correspond to focal areas of dense calcification. This appearance is typical of cartilaginous material. High-grade secondary peripheral tumor.
T2-weighted axial MRI of the pelvis demonstrates a lobulated high-signal-intensity soft tissue with local-signal-intensity septa arising from the osteochondroma on the posterior aspect of the ilium. Several areas of low signal intensity are shown; these correspond to focal areas of dense calcification. This appearance is typical of cartilaginous material. High-grade secondary peripheral tumor.
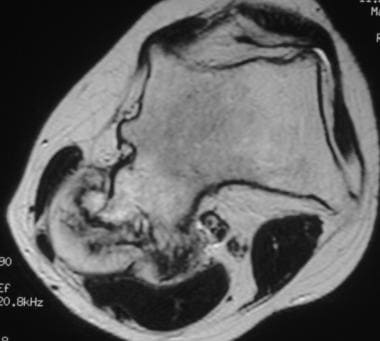 Fast spin-echo T2-weighted axial MRI of the distal femur in a patient with hereditary multiple exostoses. Image demonstrates the thick cartilage cap overlying a broad-based osteochondroma. Areas of focal reduced signal intensity in the cartilage cap correspond to foci of dense calcification. High-grade secondary peripheral tumor.
Fast spin-echo T2-weighted axial MRI of the distal femur in a patient with hereditary multiple exostoses. Image demonstrates the thick cartilage cap overlying a broad-based osteochondroma. Areas of focal reduced signal intensity in the cartilage cap correspond to foci of dense calcification. High-grade secondary peripheral tumor.
Nuclear Imaging
Central chondrosarcomas typically show significantly increased uptake of the radioisotope on isotopic bone scans, but differentiation between chondrosarcoma and enchondroma is unreliable. Uptake on isotopic bone scanning may indicate either metabolic activity in an osteochondroma or malignant transformation; these 2 conditions cannot be distinguished on the basis of such a finding. In the absence of an increase in uptake, malignancy is highly unlikely. [15]
A systematic review that compared the diagnostic accuracies of imaging modalities used in the diagnosis of chondrosarcoma found fluorodeoxyglucose positron emission tomography (FDG-PET) was more accurate than technetium-99m methylene diphosphonate, thallium-201 scintigraphy, and technetium-99m pentavalent dimercaptosuccinic acid . The negative predictive values of technetium-99m pentavalent dimercaptosuccinic acid were consistently 100%. [18]
A meta-analysis of FDG PET/CT to differentiate chondrosarcoma from benign cartilaginous lesions and to predict the histopathological grade of chondrosarcoma revealed excellent accuracy in the diagnosis of chondrosarcoma. [19]
-
Frontal radiograph of the left fibula head demonstrates a lucent lesion that contains the typical chondroid matrix calcification. Low-grade tumor.
-
Frontal radiograph of the left acetabulum demonstrates an expansile lucent lesion with no internal matrix calcification. Low-grade central tumor.
-
Bone-window CT scan of left acetabulum demonstrates matrix calcification in the expansile lucent lesion in the anterior column. Low-grade central tumor.
-
T2-weighted axial MRI of the pelvis demonstrates the high signal intensity of the acetabular lesion. Low-grade central tumor.
-
T1-weighted axial MRI of the pelvis demonstrates the low signal intensity of the acetabular lesion. Low-grade central tumor.
-
Frontal radiograph of right side of upper abdomen demonstrates a destructive, expansile lesion of the 12th rib. The lesion contains irregular calcification. High-grade central tumor.
-
CT of the right side of the upper abdomen demonstrates the expansile tumor with a large, associated soft-tissue mass containing foci of calcification. High-grade central tumor.
-
Frontal radiograph of the pelvis demonstrates extensive calcification overlying the left ilium and in the lateral soft tissues. No bone destruction is shown. High-grade secondary peripheral tumor.
-
CT scan of the pelvis demonstrates a large soft-tissue mass that contains calcification arising from a broad-based sessile osteochondroma on the posterior aspect of the ilium. High-grade secondary peripheral tumor.
-
T2-weighted axial MRI of the pelvis demonstrates a lobulated high-signal-intensity soft tissue with local-signal-intensity septa arising from the osteochondroma on the posterior aspect of the ilium. Several areas of low signal intensity are shown; these correspond to focal areas of dense calcification. This appearance is typical of cartilaginous material. High-grade secondary peripheral tumor.
-
Lateral radiograph of the distal femur in a patient with hereditary multiple exostoses. Several osteochondromas of varying appearances arise from the metaphyseal region; these typically grow away from the joint. Soft-tissue calcification is shown overlying the most posterior osteochondroma. High-grade secondary peripheral tumor.
-
CT scan of the distal femur demonstrates a broad-based osteochondroma with a thick overlying soft-tissue cap that contains focal calcification. The metaphyseal contour is irregular because of the presence of several other osteochondromas in this patient with hereditary multiple exostoses. High-grade secondary peripheral tumor.
-
Fast spin-echo T2-weighted axial MRI of the distal femur in a patient with hereditary multiple exostoses. Image demonstrates the thick cartilage cap overlying a broad-based osteochondroma. Areas of focal reduced signal intensity in the cartilage cap correspond to foci of dense calcification. High-grade secondary peripheral tumor.







