Practice Essentials
Gallstones (cholelithiasis) are solid calculi formed by precipitation of supersaturated bile composed of cholesterol monohydrate crystals or by “black pigment” of polymerized calcium bilirubinate. In the United States, 6% of men and 9% of women have gallstones, most of which are asymptomatic. More than 80% of gallstones contain cholesterol as their major component. In Asia, pigmented stones predominate, although studies have shown an increase in cholesterol stones in the Far East. Gallstones are present in 10-20% of the population in developed countries. The incidence increases with age and is higher in women. About 80% of carriers are asymptomatic, and most remain asymptomatic throughout life. Potentially life-threatening complications of gallstones include acute cholecystitis, obstructive cholangitis, and gallstone pancreatitis. Acute cholecystitis, which is typically caused by gallstone obstruction of the cystic duct, affects approximately 200,000 people in the US annually. [1, 2, 3, 4, 5]
The characteristic symptoms of gallstones are episodic attacks of severe pain in the right upper abdominal quadrant (biliary colic) for at least 15-30 minutes, with radiation to the right back or shoulder and a positive reaction to analgesics. Most attacks resolve spontaneously. The following are all highly suggestive of gallstones [1] :
-
Irregular periodicity of pain
-
Onset of pain after meals, during the evening, or at night
-
Pain awakening the patient from sleep
-
Pain duration of more than an hour
Acute cholecystitis should be suspected in a patient with fever, severe pain located in the right upper abdominal quadrant lasting for several hours, and right upper abdominal pain and tenderness on palpation (the Murphy sign). [1]
Imaging modalities
Ultrasonography is the procedure of choice in suspected gallbladder or biliary disease; it is the most sensitive, specific, noninvasive, and inexpensive test for the detection of gallstones. Current high-resolution, real-time US can identify gallstones as small as 2 mm, with a sensitivity greater than 95%. Moreover, it is simple, rapid, and safe in pregnancy, and it does not expose the patient to harmful radiation or intravenous contrast. An added advantage is that it can be performed by skilled practitioners at the bedside. [6, 7, 8, 9, 10, 11, 12] False negatives may occur on ultrasonograms when small stones are in the presence of biliary sludge. Inadequate visualization of the gallbladder may occur in obese patients or patients with abdominal wounds.
Although cholescintigraphy is recognized to have a higher sensitivity and specificity, US remains the initial test of choice for imaging patients with suspected acute cholecystitis (AC). Among its disadvantages are longer study time, ionizing radiation, and findings limited to the hepatobiliary tract. [13]
Radiography of the abdomen is of limited value for evaluating right upper quadrant pain. Although abdominal radiographs performed for initial evaluation may identify gallstones, they are not sufficient for establishing diagnoses of AC.
Only 74-79% of gallstones are identified in patients with computed tomography (CT) scanning. CT is not a screening tool for uncomplicated cholelithiasis. [14]
Magnetic resonance imaging (MRI) is not a diagnostic screening tool for cholelithiasis. Stones may be incidental findings on abdominal MRI.
(See the images below.)
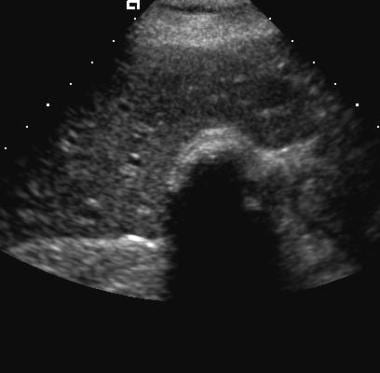
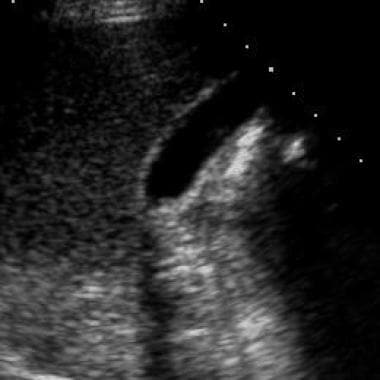
 Cholelithiasis. Ultrasound image obtained with a 4-MHz transducer demonstrates a stone in the gallbladder neck with typical acoustic shadow.
Cholelithiasis. Ultrasound image obtained with a 4-MHz transducer demonstrates a stone in the gallbladder neck with typical acoustic shadow.
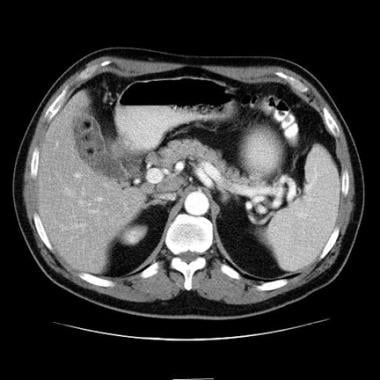
 Cholelithiasis. A noncalcified filling defect is present in the gallbladder on this contrast-enhanced CT. Ultrasound examination confirmed a mobile stone and excluded the other possible diagnoses of polyp or tumor.
Cholelithiasis. A noncalcified filling defect is present in the gallbladder on this contrast-enhanced CT. Ultrasound examination confirmed a mobile stone and excluded the other possible diagnoses of polyp or tumor.
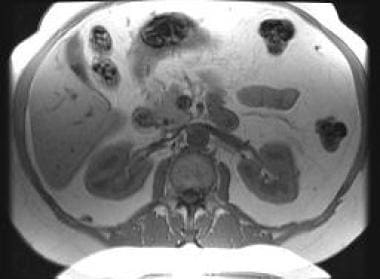 Cholelithiasis. Multiple tiny gallstones appear as signal void-filling defects in the gallbladder on this T1-weighted spoiled gradient-echo sequence.
Cholelithiasis. Multiple tiny gallstones appear as signal void-filling defects in the gallbladder on this T1-weighted spoiled gradient-echo sequence.
Each type of stone has a particular pathophysiology and specific set of risk factors that alter the equilibrium and solubility of the components of bile. Biliary microlithiasis refers to the presence of gallbladder calculi smaller than 2 mm, which is too small to be detected by current imaging techniques.
Although it originally referred to ultrasonographic findings of echogenic, nonshadowing, microscopic material within the gallbladder, the term biliary sludge currently indicates a precipitate of microcrystals occurring in bile with high mucous content. Sludge may contain microliths. Milk of calcium bile, a calcium carbonate precipitate opaque on plain radiographs, may coexist with cholelithiasis.
Guidelines
The ACR guidelines for evaluation of right upper quadrant pain include the following [13] :
-
Ultrasonography (US) is preferred as the initial imaging study for right upper quadrant pain, with supplemental cholescintigraphy performed when US results are equivocal.
-
If US shows gallstones, cholescintigraphy should be performed to exculde other sources of pain.
-
When fever is present and acute cholecystitis is suspected, the diagnosis should be confirmed or excluded using US and/or cholescintigraphy.
-
CT or MRI may be performed in equivocal cases and to identify complications of AC.
-
MRI is the preferred test for pregnant patients with right upper quadrant pain when US is inconclusive.
The European Association for the Study of the Liver (EASL) guidelines recommend that abdominal ultrasonography be used as the primary diagnostic imaging tool for suspected gallstones. In the case of strong clinical suspicion and negative abdominal ultrasound, endoscopic ultrasound or MRI may be performed. CT scanning should be performed if acute cholecystitis is suspected. [1]
The Japanese Society of Gastroenterology guidelines recommend the following stepwise algorithm for the diagnosis of cholelithiasis [15] :
-
Step 1: History and physical examination.
-
Step 2: Blood tests, ultrasonography, and abdominal radiograph.
-
Step 3: For cases that are undefined: CT and/or magnetic resonance cholangiopancreatography (MRCP), and drip infusion cholangiography with CT (DIC-CT) as the second-line modality
-
Step 4: For cases still to be diagnosed: endoscopic retrograde cholangiopancreatography (ERCP), endoscopic ultrasonography, intraductal ultrasonography, and percutaneous transhepatic cholangiography
Radiography
On plain radiographs, gallstones typically appear as single or multiple, pyramidal, faceted, or cuboidal calcifications located in the right upper quadrant (RUQ). Calcification may be central, homogeneous, or rimlike. When multiple gallstones are seen, the stones are clustered and usually faceted. Air may be present within central fissures, creating a stellate lucency termed the Mercedes Benz sign. On erect films, stones may layer in the dependent portion of the gallbladder.
Only 50% of pigment stones and 20% of cholesterol stones contain sufficient calcium to be visible on plain radiographs. Differentiation from right renal calculi usually is not problematic, because calyceal stones normally conform in shape to the collecting system. Occasionally, an oblique radiograph may be required to confirm the anterior location of gallbladder calcification.
Porcelain gallbladder is characteristic in appearance on plain radiographs, presenting as eggshell calcification in the RUQ. Other RUQ calcifications, such as hepatic granulomas, tumoral calcification, costal cartilage calcification, calcified mesenteric lymph nodes, and, rarely, hepatic artery or renal artery aneurysms, usually are not confused with gallbladder calculi.
Following plain film radiography, RUQ calcifications that are not typical in appearance or location should be investigted with US.
On oral cholecystograms (OCG), single or multiple lucent-filling defects within an opacified gallbladder are seen and usually are gravity-dependent; however, stones with high cholesterol or that contain air content may float. Mobility is demonstrated by a change in position on supine and upright films. Compression films may be necessary to displace bowel gas. The findings on OCG are characteristic, and no further imaging is required. OCG assessment of the number and size of gallstones is more accurate than US.
On OCG, a nonmobile filling defect may be an adherent stone, but it must be differentiated from polyps, adenomyomas, or, rarely, primary or metastatic tumors, heterotopic gastric mucosa, or pancreatic mucosa. Calcified stones may be obscured by contrast within the gallbladder.
Computed Tomography
Gallstones appear as single or multiple filling defects within the gallbladder and are densely calcified, rim calcified, or laminated or have a central nidus of calcification. Stones also may present as a soft-tissue density or a lucent filling defect within the bile. Some stones may contain air. [14]
Although approximately 20% of gallstones are not identified on CT, when calcified stones are present, the appearance is characteristic and no further imaging is warranted. Perform US for filling defects in which calcification is not clearly present.
A mucosal fold in the gallbladder lumen may be confused with rim-calcified stone on contrast CT. Partial volume averaging of adjacent colon contrast may obscure or mimic stones. Noncalcified stones that are isodense with bile are not visualized. Single noncalcified stones may be indistinguishable from polyps or tumors.
(See the images below.)
 Cholelithiasis. Contrast CT demonstrates multiple stones that are faintly rim calcified and contain air.
Cholelithiasis. Contrast CT demonstrates multiple stones that are faintly rim calcified and contain air.
 Cholelithiasis. Contrast-enhanced CT demonstrates a layer of calcific-dense material in the gallbladder that may be gravel or milk of calcium bile.
Cholelithiasis. Contrast-enhanced CT demonstrates a layer of calcific-dense material in the gallbladder that may be gravel or milk of calcium bile.
 Cholelithiasis. A noncalcified filling defect is present in the gallbladder on this contrast-enhanced CT. Ultrasound examination confirmed a mobile stone and excluded the other possible diagnoses of polyp or tumor.
Cholelithiasis. A noncalcified filling defect is present in the gallbladder on this contrast-enhanced CT. Ultrasound examination confirmed a mobile stone and excluded the other possible diagnoses of polyp or tumor.
Magnetic Resonance Imaging
Most gallstones have no signal on MRI and present as signal void-filling defects within the gallbladder. These are most apparent on T2-weighted sequences where signal-void stones are contrasted against high-signal bile.
Multiple, faceted, or pyramidal signal void-filling defects on T2-weighted scans are most suggestive of stones. Since the accuracy of MRI in the identification of stones within the gallbladder has not been established, confirm findings with US to rule out polyps or tumor. Stones may be indistinguishable from polyps or tumors. Stones may be missed because they are small or because of respiratory or motion artifacts.
(See the image below.)
 Cholelithiasis. Typical appearance of a gallstone as a signal void-filling defect within the gallbladder on this T2 fat-saturated MRI of the abdomen
Cholelithiasis. Typical appearance of a gallstone as a signal void-filling defect within the gallbladder on this T2 fat-saturated MRI of the abdomen
On T1-weighted sequences, bile usually shows a homogeneous low signal; however, since the composition and concentration of bile varies, it may appear inhomogeneous with areas or levels of higher signal. Therefore, signal-void stones also may be apparent on T1-weighted images (see the image below). High signal may be seen occasionally on T2-weighted images within stones that contain bile within clefts. Stones with high fatty acid content may demonstrate high signal on T1-weighted images. [16]
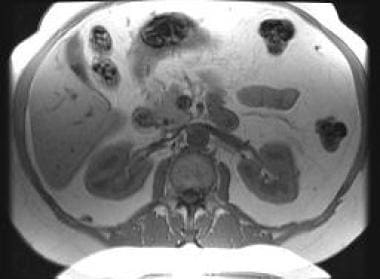 Cholelithiasis. Multiple tiny gallstones appear as signal void-filling defects in the gallbladder on this T1-weighted spoiled gradient-echo sequence.
Cholelithiasis. Multiple tiny gallstones appear as signal void-filling defects in the gallbladder on this T1-weighted spoiled gradient-echo sequence.
Ultrasonography
In a fasting patient, stones appear as intraluminal, echogenic, mobile foci that are gravity-dependent and create a clean acoustic shadow (see the first image below). In contracted and noncontracted gallbladders filled with stones, the wall-echo shadow triad is present (see the second image below), which consists of visualization of a well-defined near wall, echos from stones beneath the wall, and posterior shadowing from stones in the gallbladder fossa. [9]
 Cholelithiasis. Ultrasound image obtained with a 4-MHz transducer demonstrates a stone in the gallbladder neck with typical acoustic shadow.
Cholelithiasis. Ultrasound image obtained with a 4-MHz transducer demonstrates a stone in the gallbladder neck with typical acoustic shadow.
Differentiation from bowel is easier if there is a small amount of bile between the gallbladder wall and the stone. Air present within gallbladder calculi creates reverberation artifacts and a dirty shadow. Small stones produce an acoustic shadow only if scanned by a high-frequency transducer (5 MHz or higher), since these transducers have a smaller beam width. A shadow is produced only if the stone intercepts the entire beam.
An optimal gallbladder examination visualizes the entire organ from the distal fundus to the cystic duct/common hepatic duct junction with the patient in supine, right anterior oblique, and, if necessary, prone or upright positions. This yields an examination sensitivity and specificity of more than 95%.
In patients in whom small stones are present and a 5 MHz or higher frequency transducer cannot be used, acoustic shadowing is not seen. In these patients, mobility is demonstrated by changing patient position to confirm the diagnosis. In some nonfasting patients, repeat scans after fasting may be necessary to better distend the gallbladder to confirm the absence or presence of small stones.
A retrospective study that reviewed the records of 186 patients who underwent cholecystectomy reported 3 signs on preoperative US to be predictive of acute cholecystitis: gallbladder distention, wall edema, and pericholecystic fluid collection. When none of the US signs were registered, sonography proved to have a 72.4% (95% CI, 59.1-83.3) negative predictive value. When registering 2 or 3 signs, sonography had positive predictive values of 78% (95% CI, 56.3-92.5) and 100% (95% CI, 58.9-100), respectively. [10]
A retrospective review by Sharif et al of 577 patients found the sensitivity and specificity of point-of-care ultrasound for diagnosing cholelithiasis to be 95.2% and 93.1%, respectively. Negative predictive value was 97.6%. [6]
False positives/negatives
The false-negative rate is 1-4%. Sludge may obscure stones; adherent, nonshadowing stones may mimic polyps. Focal shadowing at the gallbladder neck resulting from refraction of the US beam may simulate a stone (see the image below). Rarely, a stone in the cystic duct may be missed. A stone-filled Phrygian cap or gallstones distal to a mucosal septum may be missed if mistaken for an adjacent bowel.
 Cholelithiasis. Do not confuse the reflective echo caused by the curve of the gallbladder neck with acoustic shadow related to a stone.
Cholelithiasis. Do not confuse the reflective echo caused by the curve of the gallbladder neck with acoustic shadow related to a stone.
A mucosal fold located at the junction of the gallbladder body and infundibulum may simulate a polyp or stone. This finding, termed a junctional fold, usually can be diagnosed accurately with careful real-time US examination.
Stones smaller than 2 mm in diameter may be mistaken for sludge, particularly if patient body habitus prevents the use of an appropriately high-frequency transducer. A porcelain gallbladder may be indistinguishable from a large intraluminal stone.
Emphysematous cholecystitis or air within the gallbladder from an enteric fistula creates reverberation artifacts that may prevent adequate examination of the gallbladder lumen. Rarely, a contracted gallbladder may not be visualized. Most importantly, if the gallbladder cannot be adequately visualized, stones may be missed.
Nuclear Imaging
Hepatobiliary imaging is a functional imaging tool used to diagnose acute cholecystitis and evaluate gallbladder contractility with determination of the gallbladder ejection fraction. In uncomplicated cholelithiasis, the study is normal (ie, the gallbladder visualizes within 60 min of radiopharmaceutical injection). However, the gallbladder ejection fraction, typically greater than 35%, may be reduced in the presence of cholelithiasis and/or chronic cholecystitis.
Normal gallbladder visualization excludes acute cholecystitis with an accuracy of 99%. Delayed visualization of the gallbladder may be seen in patients with cholelithiasis and chronic cholecystitis. In these patients, the gallbladder may not visualize until 4 hours after radiopharmaceutical injection.
A false-positive (for acute cholecystitis) result occurs in nonfasting patients, patients with other diseases (ie, acute pancreatitis), and in some patients with cholelithiasis and a gallbladder contracted due to chronic cholecystitis. Occasionally, stasis of radioactivity within the duodenal bulb may be difficult to differentiate from gallbladder activity. In such cases, oblique/lateral views (gallbladder will be anterior and duodenum posterior), delayed images, or imaging that follows administration of fluids by mouth may demonstrate clearance of radioactivity from the duodenum. (See the image below.)
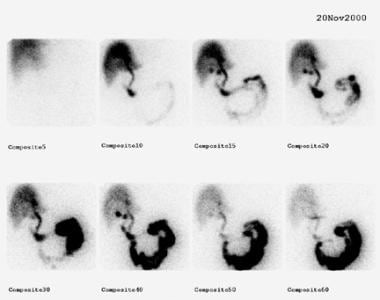 Cholelithiasis. Stasis of radioactivity in the duodenal bulb (seen on this technetium-99m diisopropyl iminodiacetic acid scan) can be misinterpreted as gallbladder activity. Delayed scans reveal clearance of activity from the duodenum and nonvisualization of the gallbladder in this patient with acute cholecystitis.
Cholelithiasis. Stasis of radioactivity in the duodenal bulb (seen on this technetium-99m diisopropyl iminodiacetic acid scan) can be misinterpreted as gallbladder activity. Delayed scans reveal clearance of activity from the duodenum and nonvisualization of the gallbladder in this patient with acute cholecystitis.
-
Cholelithiasis. Ultrasound image obtained with a 4-MHz transducer demonstrates a stone in the gallbladder neck with typical acoustic shadow.
-
Cholelithiasis. Ultrasound image obtained with a 3-MHz transducer demonstrates pyramidal nonshadowing stones.
-
Cholelithiasis. Ultrasound image obtained with a 3.5-MHz transducer demonstrates gallbladder sludge and tiny calculi.
-
Cholelithiasis. Wall-echo shadow sign indicates a stone-filled gallbladder.
-
Cholelithiasis. Do not confuse the reflective echo caused by the curve of the gallbladder neck with acoustic shadow related to a stone.
-
Cholelithiasis. Ultrasound image obtained with a 4-MHz transducer of a gallbladder filled with sludge and stones.
-
Cholelithiasis. Noncontrast CT demonstrates a typical, laminated, calcified gallstone.
-
Cholelithiasis. Contrast CT demonstrates multiple stones that are faintly rim calcified and contain air.
-
Cholelithiasis. Contrast-enhanced CT demonstrates a layer of calcific-dense material in the gallbladder that may be gravel or milk of calcium bile.
-
Cholelithiasis. A noncalcified filling defect is present in the gallbladder on this contrast-enhanced CT. Ultrasound examination confirmed a mobile stone and excluded the other possible diagnoses of polyp or tumor.
-
Cholelithiasis. Typical appearance of a gallstone as a signal void-filling defect within the gallbladder on this T2 fat-saturated MRI of the abdomen
-
Cholelithiasis. Multiple tiny gallstones appear as signal void-filling defects in the gallbladder on this T1-weighted spoiled gradient-echo sequence.
-
Cholelithiasis. Stasis of radioactivity in the duodenal bulb (seen on this technetium-99m diisopropyl iminodiacetic acid scan) can be misinterpreted as gallbladder activity. Delayed scans reveal clearance of activity from the duodenum and nonvisualization of the gallbladder in this patient with acute cholecystitis.