Practice Essentials
In 1891, Hans von Chiari described certain hindbrain abnormalities as postmortem findings in infants; these came to be known as Chiari malformations. Four types of Chiari malformations were initially described in the literature: types I, II, III, and IV. [1, 2] Chiari IV malformation is now an obsolete term; it was used in the old literature to describe extreme cerebellar hypoplasia. [3]
Chiari I malformation, or Chiari malformation type I (CMI), is the most common, having been estimated to occur in 1 in 1000 births. [4] CMI is characterized by herniation of the cerebellar tonsils through the foramen magnum into the cervical spinal canal (> 5 mm in adults and > 3 mm in children; see images below). The cerebellar tonsils often are elongated and peg-like. Mild caudal displacement and flattening or kinking of the medulla may be present. The vermis cerebelli and the fourth ventricle are normal or only minimally deformed. It is worth noting that CMI can be picked up incidentally on imaging and can be totally asymptomatic (in about 30% of patients). The most common presenting symptom is occipital headache. The degree of tonsillar descent does not always correlate with symptoms. [5] CMI is more common in females. [6]
Chiari I malformation is usually an isolated abnormality, but it can be associated with other abnormalities, including cervical cord syrinx (20%–56% cases), hydrocephalus (7%–10% cases), and skeletal anomalies (23%–45 % cases). Hydrocephalus is attributed to abnormal CSF flow due to cerebellar tonsillar descent. It is believed that syringohydromyelia is probably secondary to pathologic CSF dynamics. The exaggerated pulsatile systolic wave in the spinal subarachnoid space drives the CSF through anatomically continuous perivascular and interstitial spaces into the central canal of the spinal cord. In case there is more severe obstruction, it can cause hydrocephalus in 3%–12% of cases. [7]
Skeletal abnormalities may include platybasia, atlanto-occipital assimilation, and Sprengel deformity. There are also syndromic associations, including Klippel-Feil syndrome, Crouzon syndrome and Hadju-Cheney syndrome. [3] This is why some authors encourage the usage of "Chiari Type 1 syndrome" as a term to highlight the need for evaluation of associated abnormalities beyond just cerebellar tonsillar descent. [8]
MRI
MRI is the imaging modality of choice except in patients in whom this is contraindicated. Chiari I malformation on MRI is defined as herniation of the cerebellar tonsils below the foramen magnum of more than 3 mm in children and more than 5 mm in adults. This is found in up to 0.6% of the general pediatric population and 0.9% of the general adult population. Patients with tonsillar ectopia on brain MRI should undergo spinal MRI to completely assess degree of descent and presence of a syrinx. Other imaging findings encountered may include cervicomedullary kinking, crowding of the foramen magnum, effacement of CSF spaces, and tonsillar pegging. [9, 10, 11]
By virtue of excellent contrast resolution, MRI of the brain allows optimal visualization of the cerebellar tonsils and local anatomy. Inclusion of spine imaging may reveal the presence of syringomyelia or scoliosis. [12] MRI CSF flow study can demonstrate abnormal CSF flow patterns by virtue of attenuation of CSF spaces around the descended tonsils or brain stem.
Symptomatic patients usually require surgery, which attempts to restore CSF flow at the foramen magnum. Offered surgical procedures include suboccipital decompression, cerebellar tonsillar cautery, or resection of the C1 posterior arch. [5]
Brainstem auditory evoked potentials are widely used during posterior fossa decompression to assess functional integrity of the central auditory system during surgery. Improvement has been shown to occur primarily during bony decompression. [13] MRIs may not reliably demonstrate abnormal findings of the skeleton that can be associated with Chiari malformations, and a concomitant diagnostic CT may be required. [14, 15, 16, 17]
When MRI scanning is contraindicated, a non-contrast CT brain or CT myelography may be used. While CT offers excellent spatial resolution, its ability to resolve soft tissues is limited. Radiographs of the head, neck, spine, and extremities are helpful in assessing associated skeletal abnormalities. [18]
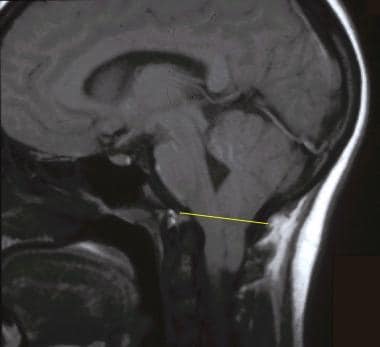 Sagittal T1-weighted magnetic resonance image of the brain. The line joining the basion to the opisthion defines the lower limit of the posterior cranial fossa and is the reference point for measuring tonsillar ectopia.
Sagittal T1-weighted magnetic resonance image of the brain. The line joining the basion to the opisthion defines the lower limit of the posterior cranial fossa and is the reference point for measuring tonsillar ectopia.
Incidental finding of Chiari I malformation in asymptomatic patients on MRI does not require routine followup imaging. Otherwise, this may result in inappropriate excessive use of imaging and add to patient anxiety. Asymptomatic patients do not require surgery, so it is important to be aware of the usually benign course of this malformation to avoid unnecessary treatment. [19, 10, 11]
In symptomatic patients, CSF velocity at the craniovertebral junction (CVJ) is known to be altered. Normalization of CSF flow and velocity at the foramen magnum is associated with resolution of symptoms. In a study by Delavari et al of pediatric patients (mean age, 14 yr; range 4–18 yr) undergoing posterior fossa decompression (PFD) for CMI, phase-contrast MRI was found to assist in diagnosing CMI and in guiding the intraoperative decision to perform duraplasty during PFD. Phase-contrast MRI demonstrated a marked and immediate increase in CSF velocity at the posterior CVJ during PFD with duraplasty. [20]
Some patients with idiopathic intracranial hypertension (IIH) have cerebellar tonsillar herniation 5 mm or more, mimicking Chiari I malformation. Ebrahimzadeh compared 98 patients with IIH, 8 with CMI, and 99 controls retrospectively to identify findings that could help differentiate between these two conditions. The authors noted that the presence of bilateral transverse sinus stenosis (BTSS) and/or hypophysis-sella ratio (HSR) less than 0.5 in patients with tonsillar herniation (ETH) of 5 mm or greater should suggest further evaluation to exclude IIH before considering CMI surgery. There were 13 of 98 patients (13.2%) with IIH who had tonsillar herniation 5 mm or greater and were significantly younger and had higher BMI compared to patients with CMI and control patients. [21]
Although the association of Chiari I malformation with cranial and vertebral anomalies is well known, this condition is not directly associated with other neuroectodermal abnormalities (ie phakomatoses). When present, neural abnormalities are attributable to the effects of tonsillar herniation. In a study comparing 30 patients with Chiari I malformation to 76 control subjects, patients with Chiari I malformation had a higher likelihood of transverse sinus stenosis associated with increased intracranial pressure (ICP). When transverse sinus stenosis is identified on MRI, further evaluation for clinical and MRI findings to support increased ICP, as well as to exclude other causes of elevated ICP, is warranted. The identification of elevated ICP in Chiari I malformation is a significant finding because increased ICP can complicate the postsurgical course after posterior fossa decompression. [22]
Acquired Chiari I malformation is reported to develop after lumboperitoneal or ventriculoperitoneal shunt placement, in addition to other conditions. Radiologic findings in patients with acquired Chiari I malformation cannot be distinguished from those in the congenital form of the malformation.
Evaluation by Davidson et al of a large group of patients with incidentally discovered Chiari I malformations demonstrated that most patients can be managed conservatively, especially in the absence of syringomyelia. [23]
(The anatomic landmarks pertinent to this disorder are shown in the image below. [24] )
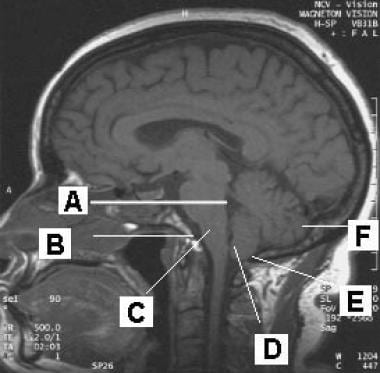 Sagittal T1-weighted magnetic resonance image of the brain. Anatomic landmarks identified include the fourth ventricle (A), basion (B), medulla oblongata (C), cerebellar tonsil (D), opisthion (E), and cerebellar hemisphere (F).
Sagittal T1-weighted magnetic resonance image of the brain. Anatomic landmarks identified include the fourth ventricle (A), basion (B), medulla oblongata (C), cerebellar tonsil (D), opisthion (E), and cerebellar hemisphere (F).
Radiography
Radiographs of the head, neck, spine and proximal extremities are helpful for assessing associated skeletal abnormalities in patients with Chiari I malformation.
Skull xrays may show reduced height of the supraocciput and clivus. Additional radiographs of the spine and extremities may be needed. In general, skeletal abnormalities are present in 23%–45% of patients with Chiari I malformation. These include the following (frequency of association is given in parentheses):
-
Platybasia, basilar invagination (25%–50%)
-
Atlantooccipital assimilation (1%–5%)
-
Klippel-Feil syndrome (5%–10%)
-
Incomplete ossification of C1 ring (5%)
-
Proatlantal remnant spina bifida at the C1 level
-
Retroflexed odontoid process (26%)
-
Scoliosis (42%)
-
Increased cervical lordosis
-
Cervical ribs
-
Fused thoracic ribs
Computed Tomography
When MRI scanning is contraindicated, a non-contrast CT brain or CT myelography may be used. While CT offers excellent spatial resolution, its ability to resolve soft tissues is limited. The real strength of CT is in delineating osseous abnormalities and bony details. On CT scans of patients with Chiari I malformation, the following findings may be observed:
-
Effaced cisterna magna
-
Hydrocephalus
-
Flattened spinal cord
-
Descending peg-like cerebellar tonsils (> 5 mm in adults, > 3 mm in children)
-
Normally positioned fourth ventricle
-
Tonsillar ectopia (see the image below)
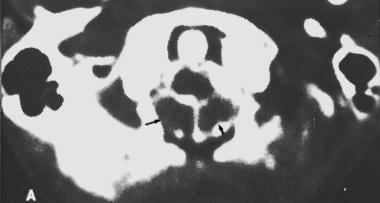 Axial computed tomography scan obtained at the C1 level after cervical myelography. The arrows mark cerebellar tonsils that are abnormally low (black arrows).
Axial computed tomography scan obtained at the C1 level after cervical myelography. The arrows mark cerebellar tonsils that are abnormally low (black arrows).
Rarely, cervical or spinal CT scans may show syringomyelia.
CT can also be used to assess associated bony abnormalities of the skull base and vertebral column. These associated abnormalities may include basilar invagination, platybasia, small posterior fossa, short horizontal clivus, retroverted dens, hypoplastic occipital condyles, segmentation anomalies (such as atlanto-occipital assimilation), scoliosis, etc. [5]
CT has a radiation burden, so regular follow-up using this modality is to be discouraged (unless MRI is absolutely contraindicated).
In the past, CT cisternography and/or myelography, supplemented by image reconstruction in non-axial planes, were used to assess tonsillar position and configuration. CT myelograms do not demonstrate the lower brainstem and bulbomedullary junction in sufficient detail. Associated syringomyelia is often missed. These techniques are rarely used now due to these limitations.
Magnetic Resonance Imaging
MRI has revolutionized the diagnostic evaluation for Chiari I malformation. This modality can be used to detect Chiari I malformation that previously remained unrecognized or was misdiagnosed. By virtue of excellent contrast resolution, tonsillar position, tonsillar configuration, and many associated abnormalities are depicted adequately on sagittal and axial T1 and T2-weighted images. [25, 26, 27, 28, 29, 30, 14, 15, 16, 17]
On MRIs, the following findings may be observed:
-
Displacement of cerebellar tonsils below the level of the foramen magnum
-
Pointed and/or peg-like tonsils
-
Narrow posterior cranial fossa
-
Elongation of the fourth ventricle, which remains in the normal position
-
Hindbrain abnormalities
-
Obstructive hydrocephalus
-
Associated abnormalities such as syringomyelia and skeletal abnormalities (if covered in the imaging field)
Tonsillar ectopia
The degree of tonsillar ectopia in Chiari I malformation is expressed as the number of millimeters that the tonsillar tips extend below a line connecting the basion with the opisthion (see the first image below). These measurements are usually undertaken on sagittal T1-weighted images. A key consideration is to use the signal intensity of cortical bone (black/low signal), and not that of the bone marrow, to define the anatomic landmarks (see the second image below). Tonsillar tips that extend less than 3 mm below the landmark are normal. Tonsillar ectopia of 5 mm is 100% specific and 92% sensitive for Chiari I malformation in adults.
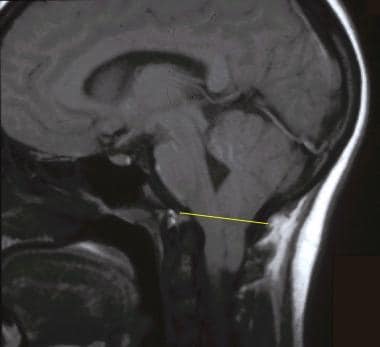 Sagittal T1-weighted magnetic resonance image of the brain. The line joining the basion to the opisthion defines the lower limit of the posterior cranial fossa and is the reference point for measuring tonsillar ectopia.
Sagittal T1-weighted magnetic resonance image of the brain. The line joining the basion to the opisthion defines the lower limit of the posterior cranial fossa and is the reference point for measuring tonsillar ectopia.
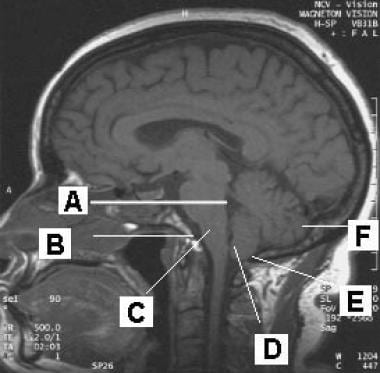 Sagittal T1-weighted magnetic resonance image of the brain. Anatomic landmarks identified include the fourth ventricle (A), basion (B), medulla oblongata (C), cerebellar tonsil (D), opisthion (E), and cerebellar hemisphere (F).
Sagittal T1-weighted magnetic resonance image of the brain. Anatomic landmarks identified include the fourth ventricle (A), basion (B), medulla oblongata (C), cerebellar tonsil (D), opisthion (E), and cerebellar hemisphere (F).
To meet the criterion for congenital Chiari I malformation, tonsillar herniation should be primary and not secondary to an intracranial mass lesion (eg, brain tumor, cerebral edema). The most reliable criterion is herniation of at least 1 cerebellar tonsil that is 5 mm or more below the plane of the foramen magnum, as defined above. However, because the cerebellar tonsils tend to ascend with age, the criteria for ectopia of the cerebellar tonsils may vary in different age groups: 6 mm in the 1st decade of life, 5 mm in the 2nd and 3rd decades, 4 mm in the 4th to 8th decades, and 3 mm in the 9th decade. [7] Asymmetric tonsillar herniation may be observed. (See the images below.)
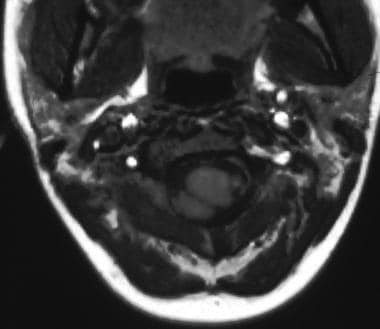 Axial T1-weighted magnetic resonance image of the upper cervical spinal cord at the level of C1-2. Note the low right cerebellar tonsil. Also note that the tonsillar ectopia is asymmetric.
Axial T1-weighted magnetic resonance image of the upper cervical spinal cord at the level of C1-2. Note the low right cerebellar tonsil. Also note that the tonsillar ectopia is asymmetric.
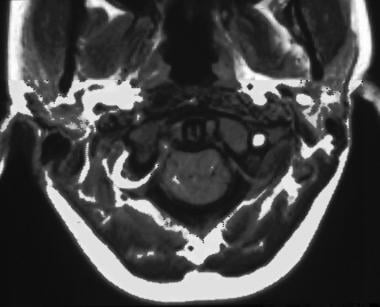 Axial T1-weighted magnetic resonance image of the upper cervical spinal cord at the C1 level. Note that the ectopic cerebellar tonsils are positioned snugly in the posterolateral subarachnoid space of the cervical spinal canal.
Axial T1-weighted magnetic resonance image of the upper cervical spinal cord at the C1 level. Note that the ectopic cerebellar tonsils are positioned snugly in the posterolateral subarachnoid space of the cervical spinal canal.
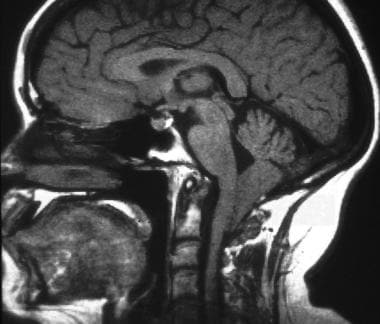 Sagittal T1-weighted magnetic resonance image of the brain. Note the advanced tonsillar ectopia, cervicomedullary kinking, diminutive posterior cranial fossa, underdeveloped basiocciput, and craniovertebral junction.
Sagittal T1-weighted magnetic resonance image of the brain. Note the advanced tonsillar ectopia, cervicomedullary kinking, diminutive posterior cranial fossa, underdeveloped basiocciput, and craniovertebral junction.
Tonsillar herniation of less than 5 mm does not exclude the diagnosis. Herniation of both tonsils that are 3–5 mm below the foramen magnum, when accompanied by certain other features, may suggest Chiari I malformation. These other features include a syrinx (see the image below), cervicomedullary kinking, elongation of the fourth ventricle and a pointed or peglike appearance of the tonsils. A key consideration is whether the patient is symptomatic.
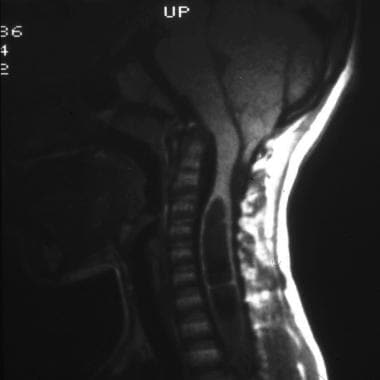 Sagittal T1-weighted magnetic resonance image of the brainstem and cervical spinal cord. Note the presence of a large syrinx in association with mild tonsillar ectopia.
Sagittal T1-weighted magnetic resonance image of the brainstem and cervical spinal cord. Note the presence of a large syrinx in association with mild tonsillar ectopia.
Other findings
Narrowing or obliteration of the retrocerebellar CSF spaces is observed in association with a meniscus sign at the lower pole of the cerebellar tonsils. The height of supraocciput is reduced and the slope of tentorium is increased. The posterior cranial fossa volume, in absolute terms and expressed as a ratio of supratentorial volume (posterior fossa ratio), is significantly smaller. However, mean brain volumes have not differed between patients and control subjects.
The cervical subarachnoid space below the level of the C2-3 discs is markedly narrowed in patients with syringomyelia as a result of spinal cord expansion. The posterior subarachnoid space below the tip of the cerebellar tonsils may be completely obliterated.
Other findings include anterior displacement of the cerebellum, kinking of the medulla, compression of the fourth ventricle, hydrocephalus (mild or moderate), and an empty sella. The cerebral aqueduct is frequently elongated and narrowed, however, no significant descent of the latter structure or brainstem is observed.
Syringohydromyelia is most commonly observed between the C4 and C6 levels. Holocord hydromyelic cavities may be present. Cervical/upper thoracic and bulbar/cervical syrinxes also are observed. Isolated thoracic syrinxes are not described. The level of widest syrinx diameter most frequently occurs at the C2-3 level. Asymmetric or multiple axial syrinxes are described.
Literature shows that foramen magnum diameter, aqueductal stroke volume (ASV), diameter of herniated tonsil, and prepontine cistern diameter-to-aqueduct of sylvius ratio (PPC/AS ratio) are important factors in syrinx development. [31]
CSF flow abnormalities
Several investigators have studied CSF flow abnormalities in Chiari I malformation. All patients had narrowing of the CSF pathways at the foramen magnum, at the C2-3 disc level and in the posterior subarachnoid space below the tip of the cerebellar tonsils. The cardiac cycle and respiration-related CSF flow pulsatility is altered. These effects are detectable with motion-sensitive MRI sequences and these can be gated to the cardiac cycle.
A prolongation of CSF systole is observed in the area above the foramen magnum. In the anterior subarachnoid space below the foramen magnum and in the posterior subarachnoid space immediately below the tips of the cerebellar tonsils, systolic velocities are reduced. The duration of CSF systole and the ratio of systolic-to-diastolic CSF displacement are also decreased. These findings indicate impaired CSF systolic (craniocaudal) pulsations. Diastolic flow is unimpaired.
A reduction of CSF flow can be observed in the subarachnoid space of the posterior cranial fossa (cisterna magna, retrocerebellar, premedullary, and prepontine cisterns) along with a compensatory pulsatile downward motion of the cerebellar tonsils. These flow abnormalities have been shown to revert to normal levels after cranial decompression.
A relationship exists between CSF flow abnormalities detected on MRIs and syringomyelia. However, CSF flow abnormalities are not correlated with the degree of tonsillar ectopia or the presence of clinical symptoms or their severity.
Phase-contrast cine MRI may be helpful in demonstrating a disturbance of CSF velocity and/or flow at the foramen magnum in patients with tonsillar ectopia of less than 5 mm. Intraoperative use of phase-contrast MRI can assess the impact of decompression on the overall CSF flow.
A review article elaborated on the current status of the literature available for CSF flow studies undertaken in Chiari 1 malformation and possible future directions. [32]
Role of surgery
Surgery is generally only indicated if the patient is symptomatic. The goal of surgery is to restore CSF flow at the foramen magnum. Surgical procedures offered include resection of C1 posterior arch ± duraplasty, suboccipital decompression, cerebellar tonsil cautery/resection, odontoid resection, craniocervical junction fusion, and other methods. These procedures aim to correct cerebellar tonsillar descent, reduction of effacement of CSF spaces, and reduction in size of syrinx.
With the widespread availability and use of MRI, incidental Chiari I malformation is now more commonly recognized. In the absence of relevant clinical symptoms or a syrinx, routine follow-up is mostly unjustifiable. This practice incurs unnecessary costs with no benefit and adds to patient anxiety. Correlation with careful clinical assessment remains the cornerstone of proper diagnosis and management.
-
Sagittal T1-weighted magnetic resonance image of the brain. The line joining the basion to the opisthion defines the lower limit of the posterior cranial fossa and is the reference point for measuring tonsillar ectopia.
-
Sagittal T1-weighted magnetic resonance image of the brain. Anatomic landmarks identified include the fourth ventricle (A), basion (B), medulla oblongata (C), cerebellar tonsil (D), opisthion (E), and cerebellar hemisphere (F).
-
Sagittal T2-weighted magnetic resonance image of the brainstem and cervical spinal cord shows syringomyelia with marginal ectopia.
-
Sagittal T1-weighted magnetic resonance image of the brainstem and cervical spinal cord. Note the presence of a large syrinx in association with mild tonsillar ectopia.
-
Axial computed tomography scan obtained at the C1 level after cervical myelography. The arrows mark cerebellar tonsils that are abnormally low (black arrows).
-
Axial T1-weighted magnetic resonance image of the upper cervical spinal cord at the level of C1-2. Note the low right cerebellar tonsil. Also note that the tonsillar ectopia is asymmetric.
-
Axial T1-weighted magnetic resonance image of the upper cervical spinal cord at the C1 level. Note that the ectopic cerebellar tonsils are positioned snugly in the posterolateral subarachnoid space of the cervical spinal canal.
-
Sagittal T1-weighted magnetic resonance image of the brain. Note the advanced tonsillar ectopia, cervicomedullary kinking, diminutive posterior cranial fossa, underdeveloped basiocciput, and craniovertebral junction.





