Practice Essentials
Male breast cancer is similar to breast cancer in females in its etiology, family history, prognosis, and treatment. In approximately 30% of cases of breast cancer in men, the family history is positive for the disease. A familial form of breast cancer is seen in which both genders are at increased risk for breast cancer. Male breast neoplasms are relatively rare, in contrast to gynecomastia, which is a relatively common condition. [1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11]
Male breast cancer accounts for less than 1% of all breast cancers diagnosed, with approximately 2600 cases annually in the United States, [12, 13, 14, 15] but the case fatality rate is similar to that in women. [16] The incidence of male breast cancer peaks at age 71 years. [17] Male breast cancer accounts for less than 0.1% of all canceers in men. [18]
Risk factors for male breast cancer include BRCA mutation, estrogen exposure/androgen insufficiency (Klinefelter syndrome, obesity, cirrhosis, exogenous estrogen therapy, testicular abnormality), and radiation exposure. [16, 19]
Male breast cancer is most commonly invasive ductal or ductal carcinoma in situ (DCIS). [16] Male breasts lack terminal ductal lobular units; thus, lobular carcinoma is extremely rare except in cases of estrogen exposure.
The majority of male breast cancers are estrogen and progesterone receptor positive, as in female breast cancer. However, male breast cancer is 3 times less likely to be HER2 positive. [20]
Preferred Examination
The American College of Radiology (ACR) Appropriateness Criteria recommends the following approach to breast imaging in symptomatic men [21, 22] :
-
In men with clinical findings consistent with gynecomastia or pseudogynecomastia, no imaging is routinely recommended.
-
If an indeterminate breast mass is identified, the initial recommended imaging study is ultrasound in men younger than 25 years and, in men 25 years of age and older, mammography or digital breast tomosynthesis.
-
If physical examination is suspicious for male breast cancer, mammography or digital breast tomosynthesis is recommended regardless of the patient’s age.
The clinical examination is key in the evaluation of a palpable mass in a male. If the clinical features strongly suggest gynecomastia, further evaluation may not be necessary. If the clinical features are equivocal or worrisome for malignancy, then additional evaluation with mammography and/or ultrasound may be appropriate. [11, 23, 24, 25, 26, 27, 28, 29, 21, 30, 31, 32]
For patients at high risk of breast cancer (family history, genetic predisposition, personal history of breast cancer), recommendations include monthly breast self-examinations, semiannual clinical breast examinations, and baseline followed by yearly mammography if gynecomastia or breast density are seen. [16]
MRI is generally not indicated in the workup for male breast cancer unless there is concern for chest wall invasion. Features worrisome for female breast cancer are the same for male breast cancer: spiculated margins, washout enhancement kinetics, and abnormal lymphadenopathy. [33]
Fluorodeoxyglucose (FDG) PET/CT has shown good diagnostic potential in recurrent male breast cancer in some studies, particularly in detecting second malignancy. [28, 29, 31, 34]
(See the image below.)
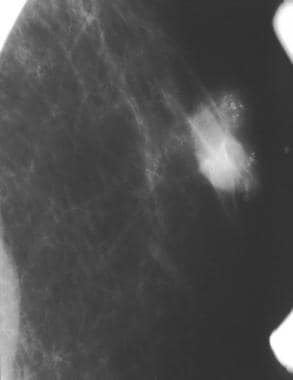 A partially circumscribed retroareolar mass in a male with suspicious microcalcifications; this is known breast cancer.
A partially circumscribed retroareolar mass in a male with suspicious microcalcifications; this is known breast cancer.
For excellent patient education resources, visit eMedicineHealth's Cancer Center. Also, see eMedicineHealth's patient education articles Breast Cancer, Breast Lumps and Pain, and Breast Self-Exam.
Mammography
On mammography, male breast cancer is typically retroareolar as it arises from the central ducts. Gynecomastia will always originate in a subareolar position, although the distribution may extend away from the nipple. An asymmetry with the morphology of gynecomastia that does not involve the subareolar breast is thus suspicious.
Masses are most commonly high density with an irregular shape. [23] Margins are usually spiculated, lobulated, or microlobulated.
Calcifications are observed less commonly than in female breast cancer and, when found, are coarser in appearance. Benign breast calcifications in men are uncommon, with the exception of vascular calcifications and fat necrosis.
Axillary adenopathy may be observed as well. [35, 24, 25] Nipple retraction, skin thickening, and increased trabeculation are worrisome findings.
Mammography is highly sensitive and specific for breast cancer in men, but it should be used to complement the clinical examination. Cases of carcinoma have been found by ultrasonography after they were obscured on previous mammograms by gynecomastia. [26]
Bilateral mammography should always be obtained to help in the evaluation of the baseline breast architecture. Almost all cases of gynecomastia will be bilateral, although typically asymmetric; thus, comparison with the contralateral side can aid in differentiating breast cancer from gynecomastia.
(See the image below.)
Ultrasonography
Ultrasound features of male breast cancer are similar to those of female breast cancer. Masses that are taller than wide (antiparallel) and hypoechoic are worrisome. The margins are angulated, microlobulated, or spiculated. [27, 23]
Similar sonographic findings may be observed in gynecomastia or inflammation; therefore, ultrasonography alone is not a reliable method to distinguish male breast cancer from other etiologies. Abscesses, sebaceous cysts, gynecomastia, and fat necrosis may all give false positives.
Evaluation of axillary lymph nodes is important if there is high clinical suspicion for breast cancer. Abnormal lymph nodes with an absent fatty hilum and asymmetric cortical thickness are suspicious for regional metastatic disease.
Questions & Answers
Overview
How does breast cancer differ between males and females?
What is the prevalence of breast cancer in men?
What are the risk factors for breast cancer in men?
What is the most common type of breast cancer in men?
What are the ACR appropriateness criteria for male breast cancer imaging?
Which tests are performed in the evaluation for breast cancer in men?
What are the guidelines for monitoring men at high risk of breast cancer?
What is the role of MRI in male breast cancer imaging?
What is the role of ultrasonography in male breast cancer imaging?
What is the role of radiography in male breast cancer imaging?
-
A partially circumscribed retroareolar mass in a male with suspicious microcalcifications; this is known breast cancer.