Practice Essentials
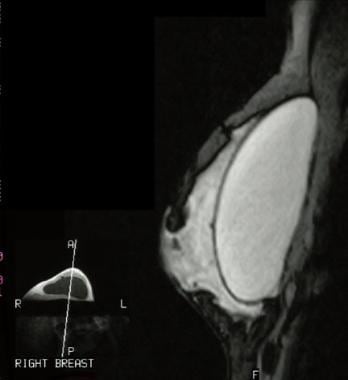
In the early 20th century, many cosmetic breast prosthetic techniques and materials were used for implants; these included polyvinyl alcohol prostheses, paraffin injections, and injections of free silicone. All of these techniques and materials had notable drawbacks and for the most part were abandoned. Silicone gel breast implants (SGBIs) have been marketed in the United States since 1962. (An intact SGBI is seen in the image below.) The US Food and Drug Administration (FDA) began regulating SGBIs in 1976 with the passage of the Medical Device Amendments. In 1992, after months of public and private meetings, the FDA restricted the use of SGBIs to specific instances of medical necessity, such as those involving patients who had undergone mastectomy. Saline breast implants have replaced SGBIs as the common breast prosthesis. Details of the FDA rulings and current status updates are available at the Breast Implants information section of the FDA Web site. [1, 2, 3, 4, 5, 6]
Approximately 3.5 million people in the United States have breast implants. [7] Each year in the United States, about 300,000 women undergo breast augmentation, and another 90,000 receive breast implants for breast reconstruction after cancer surgery. Rupture has been noted to occur in over 17% of women after primary augmentation, over 14% after revision augmentation, and over 35% after breast reconstruction. [8, 9]
The true failure incidence of gel-filled implants remains elusive. One retrospective study by Hadad et al of 284 women (542 breasts) indicated that in breast augmentation mammoplasty with silicone gel implants, larger implant size and use of the submuscular, as opposed to the subglandular, plane increase the risk of implant rupture. The average implant age at explantation (among the study’s patients, who were undergoing implant exchange) was 10 years, with the investigators finding the relative proportion of submuscular to subglandular ruptured implants to be 64%. [10]
The ability to reliably evaluate SGBIs with imaging is important because the findings at clinical examination often are nonspecific. The incidence of implant rupture increases with time, and the long-term systemic effects of SGBIs, if any, remain unclear. The diagnosis of SGBI rupture is useful to clinicians and patients; it aids in surgical decision making and helps the patient gain peace of mind. [11]
This article does not address imaging of the rupture of single-lumen saline implants (which usually is clinically obvious because extravasated saline is rapidly absorbed and breast volume quickly decreases at examination).
Imaging modalities
The imaging examinations for SGBI rupture include MRI, ultrasonography, computed tomography (CT) scanning, and mammography. [12, 13, 14, 15, 16, 17, 18, 19, 20] Patients should undergo mammography per the American Cancer Society recommendations for breast cancer screening. [21, 22]
Mammography is the most common breast imaging examination and can readily depict extracapsular free silicone. When implant rupture and extravasation are detected on mammography, further imaging studies may not be required. However, screening mammography alone is insensitive for detection of intracapsular implant rupture, and its findings often are nonspecific in the detection of SGBI rupture. [12, 23, 24]
Mammography is the preferred imaging modality for breast cancer screening, but noncontrast MRI is the imaging modality of choice for breast implant integrity and complications of breast augmentation,. MRI contrast is indicated when infection or malignancy is suspected. [25, 26, 27]
MRI is the most accurate imaging examination for the evaluation of SGBI rupture. [28] MRI's drawbacks include its cost and possible unavailability. It provides a reliable way to assess implant rupture and is highly sensitive for detection of both intracapsular and extracapsular rupture. MRI findings of intracapsular rupture include the keyhole or noose sign, subcapsular line sign, and linguine sign. [12]
Ultrasonography can be used to assess the internal structure of the implant. [29, 30, 31, 26] Common ultrasound signs of intracapsular rupture include the keyhole or noose sign, subcapsular line sign, and stepladder sign. Extracapsular silicone has a distinctive snowstorm or echogenic noise appearance. Ultrasonography is fairly accurate and more available than MRI but is highly operator dependent and has a steep learning curve. [12, 32, 27]
CT scanning can show findings similar to those obtained with MRI, but the modality involves ionizing radiation, and it has not been systematically studied to the extent that MRI has been. [33] A prospective study of 46 patients with SGBI who underwent MRI and dual-energy CT (DECT) reported similar performance for the detection of rupture and the presence of silicone in regional lymph nodes. [34]
Bengtson and Eaves showed that MRI scans, surgeon-performed high-resolution ultrasound scans, and radiologist-performed high-resolution ultrasound scans were all accurate in predicting implant shell integrity. [29, 30] According to a study by Bogetti et al, the sensitivity and specificity of ultrasound scans were 90% and 80%, respectively, and the sensitivity and specificity of MRI scans were 87% and 85%, respectively. [29, 31]
Guidelines
The US Food and Drug Administration recommends that individuals who receive silicone gel implants should undergo MRI or ultrasound screening at 5-6 years after implantation to screen for silent rupture, followed by screening every 2-3 years. However, the compliance rate with MRI has been less than 5% because of high cost and inconvenience. [35, 36, 37]
The American College of Radiology (ACR) has published the following guidelines regarding evaluation of breast implant integrity [38] :
-
For asymptomatic women of any age with saline implants, no imaging is recommended for implant evaluation.
-
For women < 30 yr with saline implants and clinical examination equivocal for implant rupture, breast ultrasonography (US) is recommended for implant evaluation.
-
For women 30-39 yr with saline implants and clinical examination equivocal for implant rupture, mammography, digital breast tomosynthesis (DBT), or breast US is recommended for implant evaluation.
-
For women ≥40 yr with saline implants and clinical examination equivocal for implant rupture, mammography or DBT is recommended for implant evaluation.
-
For asymptomatic women of any age with silicone implants, no imaging is recommended for implant evaluation.
-
For women < 30 yr with silicone implants and suspected implant complication, breast MRI without contrast or US is recommended for implant evaluation.
-
For women 30-39 yr with silicone implants and suspected implant complication, breast MRI without contrast, mammography and DBT, or breast US is recommended for implant evaluation.
-
For women ≥40 yr with silicone implants and suspected implant complication, breast MRI without contrast, mammography, or DBT is recommended for implant evaluation.
-
For women < 30 yr with silicone implants (current or prior) and unexplained axillary adenopathy, axillary US is recommended for evaluation of unexplained axillary adenopathy.
-
For women 30-39 yr with silicone implants (current or prior) and unexplained axillary adenopathy, axillary US is recommended for evaluation of unexplained axillary adenopathy. Mammography or DBT may also be performed as a complementary examination.
-
For women ≥40 yr with silicone implants (current or prior) and unexplained axillary adenopathy, mammography or DBT and axillary US are recommended for evaluation of unexplained axillary adenopathy. These procedures are complementary and should be performed together.
-
For women of any age with suspected implant-associated anaplastic large-cell lymphoma and breast implants of any type, breast US is recommended.
Radiography
Findings at mammography include the following:
-
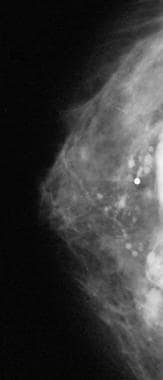
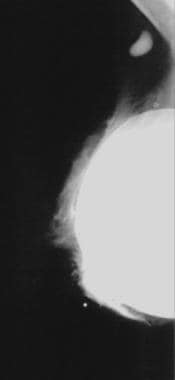
Rupture with deflation and silicone extravasation (shown in the images below)
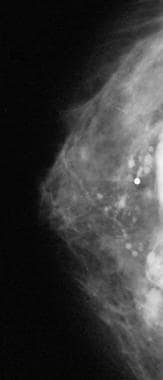 Craniocaudal mammogram shows free extracapsular silicone around a ruptured silicone gel breast implant.
Craniocaudal mammogram shows free extracapsular silicone around a ruptured silicone gel breast implant.
-
Measurable periprosthetic opaque band or rim of tissue
-
Periprosthetic calcification
-
Asymmetry in the size and/or shape of the implant
-
Focal implant herniation
Silicone injections and SGBIs can limit the sensitivity of mammography. Implant-displaced views should be obtained, if possible. Comparison with prior images is strongly advised.
When rupture and extravasation are present, confidence is high. However, these findings are uncommon, and other signs are both insensitive and relatively nonspecific. When screening mammography performed for other reasons reveals incidental signs of rupture, the sensitivity is high.
Magnetic Resonance Imaging
MRI can be used to exploit differences in silicone, water, and fat resonance frequencies to deliver high-resolution images of SGBIs. [28, 39, 40] The approximate resonance frequency of silicone is 100 Hz lower than that of fat and 320 Hz lower than that of water. Because the resonance of silicone is similar to that of fat, silicone appears similar to fat on nonselective chemical fat- or water-suppressed images. [41, 42, 43, 17] MRI has a reported a sensitivity of 76-95% and a specificity of 93-97% in the detection of rupture.
Extensive gel bleeding can have the same findings as those of an intracapsular rupture, in which the keyhole sign is present and the linguine sign is absent. Some authors believe that a tiny tear is present and that it can be found with diligent examination at surgery. Other authors maintain that microscopic gel bleeding alone is the cause. Radial folds are normal invaginations of the silastic membrane, and they should not be confused with the keyhole sign. Silicone should not be present both inside and outside a radial fold.
On short–inversion time inversion-recovery (STIR) images, the fat signal is suppressed and water and silicone are bright. Water-suppressed STIR sequences produce a silicone-only image. Chemical-shift imaging with the modified 3-point Dixon protocol provides both a silicone-only and a water-and-fat image with a single sequence. The relative appearances of silicone, fat, and water on various types of MRIs are summarized in the following table:
Table. Relative Appearances of Silicone, Fat, and Water on MRI of SGBI Rupture* (Open Table in a new window)
MR Pulse Sequence† |
Silicone |
Fat |
Water |
FSE T2 weighted |
Bright |
Moderate |
Very bright |
FSE T2 weighted, water suppressed |
Bright |
Moderate |
Dark |
STIR |
Bright |
Dark |
Very bright |
STIR water suppressed |
Bright |
Dark |
Dark |
Three-point Dixon, silicone only |
Bright |
Dark |
Dark |
* Adapted, with permission, from Bassett and Jackson. [44] † FSE indicates fast spin echo. |
|||
While exact protocols differ among institutions, in general, orthogonal-plane imaging with several pulse sequences is performed. Image quality is maximized with the use of a dedicated phased-array breast coil and a high–field-strength magnet; however, in our experience, an adequate examination can also be performed with a low–field-strength, open-sided magnet.
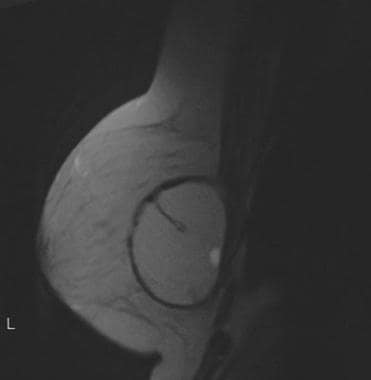
(Intact silicone breast implants are shown in the MRI scans below.)
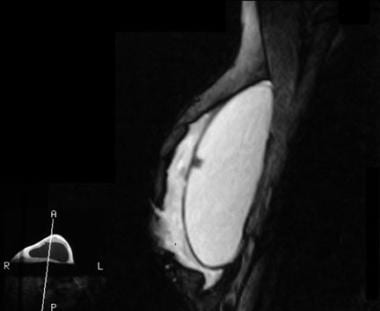 An intact silicone gel breast implant with a valve appears as a low–signal-intensity region in the retroareolar area. Most silicone implants are valveless; this implant includes a port for addition of saline by the implanting surgeon, for custom-fit sizing. No saline was added to this implant.
An intact silicone gel breast implant with a valve appears as a low–signal-intensity region in the retroareolar area. Most silicone implants are valveless; this implant includes a port for addition of saline by the implanting surgeon, for custom-fit sizing. No saline was added to this implant.
MRI findings in intact single-lumen implants
These include the following:
-
Smooth, low–signal-intensity silicone membrane shell
-
A few internal water droplet signals (common; not a reliable indication of rupture)
-
Reactive fluid around textured implants (common; not indicative of rupture)
-
Fibrous capsule (dark, ringlike structure around the implant)
MRI findings in double-lumen implants
Gradual deflation of the saline chamber over time results in complex fold patterns and occasional, nonspecific findings of fluid around the outer capsule of the implant.
MRI findings in intracapsular rupture
The linguine sign refers to a collapsed and folded elastomer shell that is floating in gel. This is the most reliable sign of intracapsular rupture.
The keyhole (ie, teardrop, inverted teardrop, noose) sign refers to the presence of silicone both inside and outside a radial fold. (These signs are shown in the images below.)
 Fast spin-echo T2-weighted magnetic resonance image shows the keyhole sign. Silicone appears on both sides of the radial fold. The differential diagnosis includes intracapsular rupture and extensive gel bleeding. A small water droplet is in the posterior aspect; small water droplets have no prognostic importance in silicone gel breast implant rupture.
Fast spin-echo T2-weighted magnetic resonance image shows the keyhole sign. Silicone appears on both sides of the radial fold. The differential diagnosis includes intracapsular rupture and extensive gel bleeding. A small water droplet is in the posterior aspect; small water droplets have no prognostic importance in silicone gel breast implant rupture.
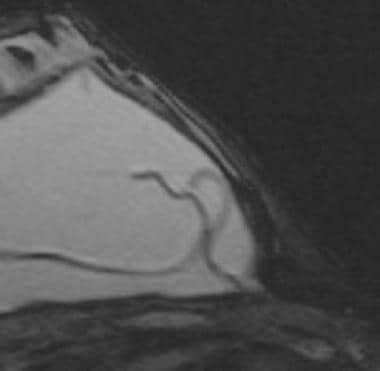 Magnetic resonance image shows the keyhole, or inverted teardrop, sign. The linguine sign is present elsewhere on the image, and a portion of the sign is adjacent to the keyhole sign. These findings are consistent with an intracapsular silicone gel breast implant rupture.
Magnetic resonance image shows the keyhole, or inverted teardrop, sign. The linguine sign is present elsewhere on the image, and a portion of the sign is adjacent to the keyhole sign. These findings are consistent with an intracapsular silicone gel breast implant rupture.
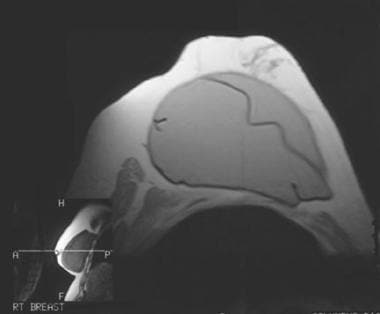
MRI findings in extracapsular rupture
Macroscopic extrusion of silicone through the fibrous capsule into the surrounding parenchyma, pectoralis muscle, or lymph nodes is present. [14] Findings in intracapsular rupture should be expected. (Extracapsular silicone is seen in the image below.)
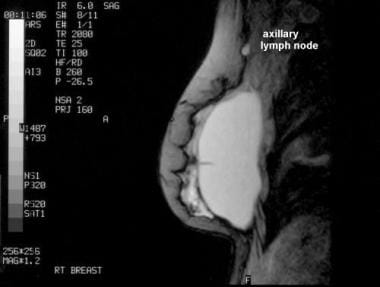 Sagittal magnetic resonance image shows extracapsular silicone, with a high–signal-intensity lesion in axilla (which is compatible with silicone in node, as shown on the mammogram).
Sagittal magnetic resonance image shows extracapsular silicone, with a high–signal-intensity lesion in axilla (which is compatible with silicone in node, as shown on the mammogram).
MRI findings in internal rupture of double-lumen implants
Failure of the inner shell may be depicted as saline droplets that are floating in the silicone gel; this is considered a form of intracapsular rupture. The presence of some saline droplets is a normal finding in single-lumen implants.
MRI findings in capsular contracture
Asymmetrical, serrated, focal folding of the fibrous capsule that changes the normal ovoid appearance of the implant may be present.
A transverse diameter of less than twice the anteroposterior depth corresponds well to clinically evident contracture.
Ultrasonography
Typically, a high-frequency (eg, 10-MHz) transducer is used. [19, 20, 45] Sensitivity ranges from 47 to 74%; specificity, from 55-96%. An anechoic interior, although rare (4 of 64 implants in one series), is a strong indicator of an intact implant. Ultrasonography is limited in the evaluation of the posterior implant wall, because of marked beam attenuation caused by silicone. Use of a low-frequency transducer (eg, 5 MHz) can help improve visualization of the posterior wall of the implant and the adjacent soft tissues. Reverberation artifacts from the near-side interface may limit visibility of the superficial implant margins. Prior silicone injections limit visualization of the implant. [32, 29]
Ultrasonographic findings in an intact implant
Ultrasound findings in an intact patient include the following:
-
Smooth, thin, linear membrane
-
Sonolucent anechoic interior (most reliable but insensitive finding)
-
Reverberation artifact from the proximal membrane wall
-
Radial folds possible
-
Linear internal echoes
With regard to radial folds, parts of the implant envelope may be connected by scanning adjacent portions of the implant.
Linear internal echoes do not indicate rupture. The abundance of the linear echoes has been evaluated, and their effect in the prediction of rupture is not statistically significant. [46]
Ultrasonographic findings in intracapsular rupture
Findings in intracapsular rupture include the following:
-
Stepladder sign
-
Echogenic implant lumen
-
Focal, prominent, irregular bulge in the implant
-
Ill-defined or poorly visualized implant margin
The stepladder sign is identified as multiple, discontinuous, parallel, linear echoes in the lumen. It is the most reliable ultrasonographic finding in intracapsular rupture and is analogous to the linguine sign at MRI.
Ultrasonographic findings in extracapsular rupture
Findings include the following [14] :
-
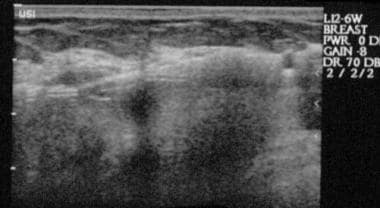
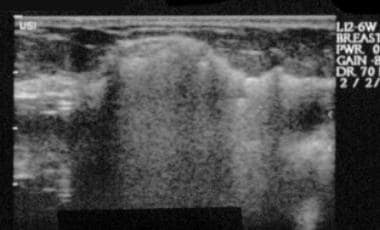
Snowstorm, or hyperechoic, noise (shown in the images below)
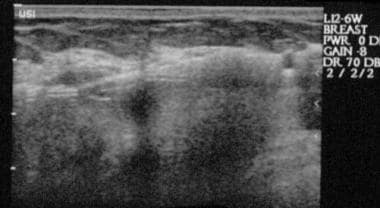 Longitudinal ultrasonogram shows the snowstorm, or hyperechoic, noise associated with the capsule in proven extracapsular silicone gel breast implant rupture. Usually, the interior of an intact implant is sonolucent.
Longitudinal ultrasonogram shows the snowstorm, or hyperechoic, noise associated with the capsule in proven extracapsular silicone gel breast implant rupture. Usually, the interior of an intact implant is sonolucent.
-
Silicone masses (granulomas) - The same hyperechoic noise pattern for snowstorm noise (described below); possibly hyperechoic or hypoechoic and similar to other breast lesions (including carcinoma) or nearly sonolucent and similar to breast cysts (hyperechoic noise is often near or around cystic-appearing masses)
-
Snowstorm pattern in involved axillary lymph node
Snowstorm noise refers to intense, homogeneous echogenicity with loss of the posterior detail of free silicone. (Silicone can replace portions of the implant envelope, be extruded into the breast parenchyma, forming nodules, and migrate to lymph nodes.)
Indeterminate findings
Indeterminate findings include the following:
-
Coarse echogenic aggregates
-
Cobwebs
-
Smooth focal bulge in the implant
-
Peri-implant fluid collections
In one study, coarse echogenic aggregates occurred in 41% of surgically confirmed implant ruptures. [47] They have also been found to occur in approximately the same percentage of implants that have been confirmed as intact at surgery.
Cobwebs are delicate, short, linear echoes that are diffusely scattered throughout the implant. (Most authors consider this finding to be a normal variant; they are also called "commas" in some reports.)
-
Inversion recovery magnetic resonance image shows an intact silicone gel breast implant.
-
An intact silicone gel breast implant with a valve appears as a low–signal-intensity region in the retroareolar area. Most silicone implants are valveless; this implant includes a port for addition of saline by the implanting surgeon, for custom-fit sizing. No saline was added to this implant.
-
Magnetic resonance image shows a normal radial fold, which appears as a low–signal-intensity line through the implant.
-
Fast spin-echo T2-weighted magnetic resonance image shows the keyhole sign. Silicone appears on both sides of the radial fold. The differential diagnosis includes intracapsular rupture and extensive gel bleeding. A small water droplet is in the posterior aspect; small water droplets have no prognostic importance in silicone gel breast implant rupture.
-
Magnetic resonance image shows the keyhole, or inverted teardrop, sign. The linguine sign is present elsewhere on the image, and a portion of the sign is adjacent to the keyhole sign. These findings are consistent with an intracapsular silicone gel breast implant rupture.
-
Craniocaudal mammogram shows free extracapsular silicone around a ruptured silicone gel breast implant.
-
Mediolateral oblique mammogram shows extracapsular silicone. Note the opaque axillary lymph node, which is consistent with nodal uptake of silicone.
-
Sagittal magnetic resonance image shows extracapsular silicone, with a high–signal-intensity lesion in axilla (which is compatible with silicone in node, as shown on the mammogram).
-
Longitudinal ultrasonogram shows the snowstorm, or hyperechoic, noise associated with the capsule in proven extracapsular silicone gel breast implant rupture. Usually, the interior of an intact implant is sonolucent.
-
Longitudinal ultrasonogram shows the snowstorm appearance of the soft tissues of the breast, which is consistent with extracapsular silicone gel breast implant rupture and free parenchymal silicone.