Practice Essentials
The temperomandibular joint (TMJ) is defined as the area where the mandible articulates with the temporal bone of the cranium. [1, 2] Symptomatic temporomandibular joint dysfunction affects 28% of the adult population, with a smaller, although significant, percentage experiencing severe impairment. [3] A displaced disc is a critical sign of TMJ dysfunction, and it is important for the maxillofacial radiologist to detect early imaging signs of dysfunction because the condition can ultimately become irreversible, characterized by osteoarthritic changes such as condylar flattening or osteophytes. [1, 4, 5, 6]
The clinical problem is complex because TMJ dysfunction is multifactorial. Although most occurrences are related to internal derangement, many joints are painful secondary to nondiscogenic causes, such as referred pain from spondylosis of the upper cervical spine and other inflammatory and neoplastic bone lesions in the vicinity of the TMJ. A variety of pathologies may affect the TMJ, of which internal derangement is the most common.
Plain film and tomographic examinations are useful screening modalities for meniscus abnormalities in the TMJ in that they are valuable for determining the presence of osseous changes and traumatic injury to the osseous components of the joint. MRI is the examination of choice because it is the only modality that directly visualizes the meniscus and other soft-tissue joint components. Bony components are visualized better on CT scans than on MRI scans. [7, 8, 9, 10]
Advantages of MRI is that it is noninvasive, requires no ionizing radiation for image acquisition, readily obtains multiplanar images in an infinite array of anatomic sections, allows direct visualization of soft-tissue components (including disc and joint structures), allows easy bilateral assessment, allows assessment of joint effusion and inflammation, and easily can image structures outside the joint, such as the joint capsule and muscles of mastication. [11, 12, 13, 14, 15] In addition, fewer artifacts result from dense bone, and it allows imaging of the bone marrow of the condyle.
Disadvantages of MRI include high cost, inability to visualize perforations of the posterior attachment or of the disc, difficulty in assessing accurate jaw position for the initiation or adjustment of protrusive splint therapy, claustrophobia in some patients, length of scanning time, and inferior images of hard tissues.
(See the images below.)
 Anteroposterior projection skull radiograph showing an osteoma (O) involving the right temporal bone and the temporomandibular joint.
Anteroposterior projection skull radiograph showing an osteoma (O) involving the right temporal bone and the temporomandibular joint.
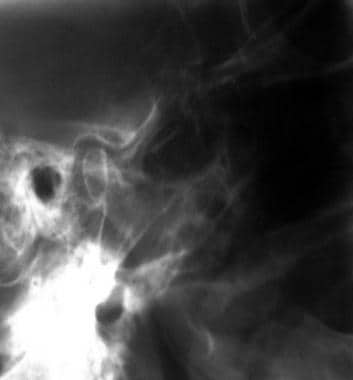 Conventional tomogram of the right temporomandibular joint showing a normal joint. Note that the bony detail is visualized well.
Conventional tomogram of the right temporomandibular joint showing a normal joint. Note that the bony detail is visualized well.
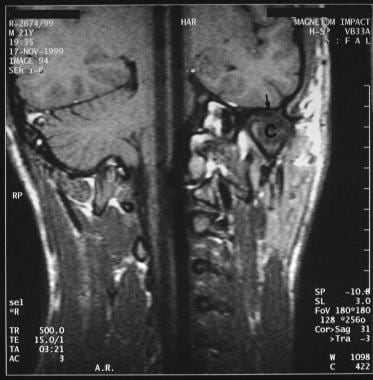
 Coronal T1-weighted MRI sequence through the left temporomandibular joint of a 37-year-old man previously treated conservatively for a left meniscus dysfunction. Flattening and sclerosis of the mandibular condyle (c) is noted but no meniscus is identified as a result of automeniscectomy (confirmed on sagittal T1-weighted scans).
Coronal T1-weighted MRI sequence through the left temporomandibular joint of a 37-year-old man previously treated conservatively for a left meniscus dysfunction. Flattening and sclerosis of the mandibular condyle (c) is noted but no meniscus is identified as a result of automeniscectomy (confirmed on sagittal T1-weighted scans).
Planar radionuclide imaging using technetium-99m methylene diphosphonate/hydroxymethylene diphosphonate (99mTc MDP/HMDP) and single-photon emission computed tomography (SPECT) scanning using 99mTc MDP/HMDP have been found to be sensitive methods for the diagnosis of TMJ disorders. [16, 17, 18, 19] They can be used as screening tests before proceeding, if necessary, to other imaging techniques, such as MRI. Radionuclide imaging is a highly sensitive technique for evaluating the TMJ but is not specific; arthritis, tumor, inflammation, and trauma can give rise to similar appearances.
Arthrography/arthroscopy is used very selectively but is often considered the gold standard. [20] Arthrography is a sensitive and highly specific technique in the evaluation of TMJ meniscus abnormalities, but it is invasive and uncomfortable for the patient. Unlike arthrography, MRI is noninvasive, requires no ionizing radiation for image acquisition, readily obtains multiplanar images in an infinite array of anatomic sections, allows direct visualization of soft-tissue components (including disc and joint structures), allows easy bilateral assessment, allows assessment of joint effusion and inflammation, and easily can image structures outside the joint, such as the joint capsule and muscles of mastication. [11, 12, 13, 21, 22]
Ultrasound studies have been done in cases of disc displacement. Ultrasound has a number of advantages over MRI for the initial screening of TMJ dysfunction, including the ability to observe motion, clicking, crepitus, and snapping sensations in real-time. Additionally, patients can direct the operator to areas of pain during the evaluation. [9, 23] Abnormal TMJ findings on ultrasound require confirmation by MRI, and a number of causes of dysfunction cannot be visualized, including medial and lateral disc displacements and subcortical osseous abnormalities. [24]
As a primary imaging modality for internal derangement of the TMJ, CT scanning has fallen into disfavor because of the superiority of MRI, but it does have specialized imaging capabilities for assessing bone detail, for taking disc density measurements, and for permitting 3-dimensional (3D) assessment of congenital, traumatic, and postsurgical conditions involving the TMJ.
Etiology
The etiology of internal derangement is obscure, although in 25% of patients, a history of trauma is elicited; in these cases, 30% of the causes are iatrogenic and result, for example, from procedures that necessitate jaw extension. These include tonsillectomy, endoscopy, and molar tooth extraction.
Typically, the patient with TMJ dysfunction is a young woman aged 20-40 years who has experienced symptoms for 3-5 years. Not uncommonly, misdiagnosis continues for several years, particularly during childhood and adolescence, because of a variety of poorly understood presenting symptoms. As a result, severe degenerative changes in the TMJ are observed even in children.
A wide variety of abnormalities can present with signs and symptoms mimicking a possible problem in the TMJ. Studies have shown that physical examination alone is inaccurate in determining the status of the joint. Accuracy of the clinical diagnosis for the specific status of the joint is only 50-65%. The primary rationale for imaging the TMJ lies in the fact that mechanical internal derangement resulting from an anteriorly displaced disc and its concomitant pathology is treated differently from the multiple miscellaneous disorders of the TMJ and from myofascial pain dysfunction (MPD) syndrome. MPD is a common disorder affecting a considerable population, and clinical features include jaw pain, limited opening, headache, and earache.
Treatment
Imaging allows accurate staging of internal derangement for operative planning. Patients in whom surgery is planned on one side frequently require evaluation of the asymptomatic joint, because silent TMJ dysfunction is frequent. Advances in imaging have contributed greatly to the understanding and treatment of TMJ dysfunction and related pathologies. MRI is regarded as the modality of choice in the evaluation of TMJ dysfunction, although other modalities still have specific roles to play. [11, 21, 22, 25]
The objective of conservative and surgical treatment is to shorten the period of the patient's symptoms and to reduce the incidence of long-term joint disfigurement, such as osteoarthrosis, ankylosis, and avascular necrosis. A variety of splints are used to change the position of the meniscus and/or occlusion, but although splints may stabilize the joint, they cannot reverse joint pathology. [26] The most commonly performed surgical procedures include discal plication with repositioning of the disc, and simple discectomy, with or without the employment of a disc implant. [27]
Various alloplastic and autogenous materials can be used to fashion a disc implant, such as Teflon, silicon, silastic, and fascial, dermal, and rib grafts. The object of the disc implant is to reduce the probability of osteoarthrosis, adhesions, and recurrent pain and dysfunction. In more advanced cases, condylectomy and reduction osteotomy of the articular eminence may be necessary. The complications of joint stabilization may cause continued TMJ pain; these complications include avascular necrosis, osteochondritis dissecans, and osteoporosis, which may lead to progressive bone remodeling.
Differential diagnosis
The differential diagnosis of meniscus derangement includes the following [28] :
-
Osteoarthritis (OA) - OA of the TMJ is a common clinical problem, and most TMJ meniscus dysfunction results in degenerative arthritis. Primary OA, OA resulting from trauma, mandibular asymmetry, and calcium pyrophosphate dihydrate crystal deposition diseases also are well-known causes of degenerative arthritis.
-
Rheumatoid arthritis (RA) and other erosive arthritides affecting the TMJ is not uncommon; some patients with RA may first seek dental consultation because of TMJ-related problems. Imaging findings in an RA-affected TMJ are similar to findings elsewhere and include erosions, osteoporosis, joint narrowing, and restricted range of movement associated with flattening of the condyle and glenoid fossa. CT scanning demonstrates the changes better than does conventional radiography, although MRI can be useful in demonstrating joint effusion and pannus, as well as the morphology of the disc. Other erosive arthritides, such as psoriatic arthritis, ankylosing spondylitis, and systemic lupus erythematosus, can present in a clinically and radiologically similar manner.
-
Septic arthritis - Infections affecting the TMJ, including pyogenic or granulomatous conditions, are rare. Most infections of the TMJ result from extension of oral infections or as a complication of TMJ surgery. The clinical setting/presentation is sufficiently characteristic to avoid being confused with other TMJ pathology.
-
Gout - Gout is an exceptional cause of TMJ arthritis. As elsewhere, the presentation may be acute, usually in a patient with known gouty arthritis who has appropriate serum biochemistry; aspirate for negatively birefringent crystals.
-
Tumor - Tumors of the TMJ are rare. Osteosarcomas of the TMJ are the most common malignant tumors, but osteomas, giant cell tumors, fibrous cortical defects, and nonossifying fibromas can affect the TMJ. Malignant tumors usually affect the TMJ by direct extension of a mandibular tumor, such as a metastatic deposit or an osteosarcoma. Tumors may be seen equally well on conventional radiography, radionuclide scanning (particularly SPECT), CT scanning, and MRI, all of which are complementary.
-
Nonneoplastic miscellaneous conditions - Some nonneoplastic processes that affect other body joints, such as osteochondromatosis, pigmented villonodular synovitis, and ganglion cysts, also may involve the TMJ. Clinical presentation and imaging findings also are similar. Pathologically, synovial chondromatosis is characterized by proliferation of the synovium with formation of foci of hyaline cartilage, which may calcify and eventually detach and form loose bodies within the joint. Demonstration of calcified bodies in and around the TMJ on conventional radiographs, but particularly on CT scans, suggests the diagnosis. Usually, the TMJ shows changes of OA on conventional radiographs in the form of marginal sclerosis and lytic changes.
-
Ganglion cysts - Ganglion cysts are mucin-containing cystic structures; they may develop because of herniation of the joint synovium into para-articular tissue. The TMJ is a rare site for this complication, and only a dozen or so cases have been reported. Plain radiography has little to contribute.
-
Congenital malformations - Congenital malformations of the TMJ are uncommon and are usually associated with abnormalities of the external auditory canal and the middle ear. Rarely, they may clinically mimic discal abnormality. The most common malformation is condylar hyperplasia, which presents with development of facial asymmetry and dental occlusion. The hypertrophied condyle also may be confused with benign bone tumors. These changes are demonstrated well on conventional radiography.
Radiography
Radiography and conventional tomography can detect the shape of the condyle, joint outline, and osseous changes (including flattening, osteophytosis, sclerosis, and erosion). Comparisons of techniques indicate that tomography is superior to radiography, but it requires an experienced operator, requires more imaging time, and renders a higher radiation dose. However, if a strong clinical need exists for determining the position of the condyle in the glenoid fossa, tomography should be used. A transcranial projection is not reliable for determining the condylar position.
Other useful information that can be obtained on radiography is the extent of condylar translation at the maximal mouth opening. Restriction of anterior condylar translation at the maximal mouth opening implies that the condyle does not translate all the way to the most inferior aspect of the articular eminence. This is an indication that soft tissue is interposed between the joint components, which may indicate disc displacement without reduction but is not pathognomonic. However, these methods are ineffective in evaluating internal derangement of the TMJ.
(See the images below.)
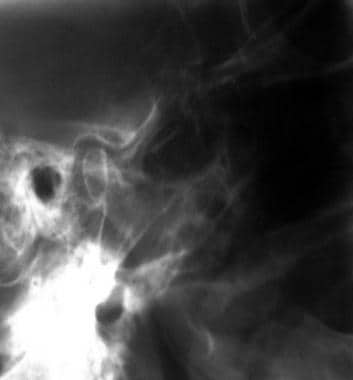 Conventional tomogram of the right temporomandibular joint showing a normal joint. Note that the bony detail is visualized well.
Conventional tomogram of the right temporomandibular joint showing a normal joint. Note that the bony detail is visualized well.
 Conventional tomogram of the right temporomandibular joint showing a normal joint. Note that the bony detail is visualized well (same patient as in the previous image).
Conventional tomogram of the right temporomandibular joint showing a normal joint. Note that the bony detail is visualized well (same patient as in the previous image).
 Tomogram through the left temporomandibular joint showing osteopenia with minor remodeling. Both sides were examined with the mouth open and closed. Note the limitation of movement on both sides.
Tomogram through the left temporomandibular joint showing osteopenia with minor remodeling. Both sides were examined with the mouth open and closed. Note the limitation of movement on both sides.
 Tomogram through the left temporomandibular joint showing osteopenia with minor remodeling. Both sides were examined with the mouth open and closed. Note the limitation of movement on both sides.
Tomogram through the left temporomandibular joint showing osteopenia with minor remodeling. Both sides were examined with the mouth open and closed. Note the limitation of movement on both sides.
Arthrography
TMJ arthropathy implies radiographic imaging of the TMJ after introduction of radiographic contrast into the upper and/or lower joint spaces of the TMJ. TMJ arthrography is indicated for evaluating soft-tissue components, especially disc position, function, and morphology (eg, perforation, swelling, adhesions) in patients presenting with a suggested internal derangement of the TMJ. [20] The ability to assess soft-tissue components of the TMJ allows arthrography to go beyond simple delineation of osseous structures, as in transcranial or tomographic radiographs.
The objective of arthrography is to evaluate disc function during opening and closing maneuvers of the jaw. If the disc is displaced and reduces on jaw opening, the dynamic events are depicted more clearly with fluoroscopic analysis. The smooth to-and-fro flow of contrast material from the anterior recess in the closed-jaw position to the posterior recess in the open-jaw position indicates normal function. A continual collection of contrast material in the anterior recess of the lower joint compartment and progressive deformity of the anterior recess with jaw opening help to confirm the diagnosis of disc displacement without reduction. Perforations are detected easily during initial filling of the joint by observing contrast material flow from the inferior compartment to the superior compartment.
Arthrography can be performed as a single-contrast examination in which iodinated contrast is injected into one or both of the TMJ spaces, or as double-contrast arthrography in which the injection of iodinated contrast is combined with a gas contrast medium. Double-contrast arthrography, or more specifically, dual-space, double-contrast arthrography, is technically more difficult to perform and usually takes longer than does a single-contrast examination. However, double-contrast images depict with greater detail the articular surfaces, the extent of the joint spaces, and the configuration of the disc.
A side-by-side comparison of single-contrast arthrography with the double-contrast form of the modality has shown that single-contrast, lower-compartment arthrography is better for demonstrating joint dynamics. Double-contrast, dual-space arthrotomography better demonstrates anatomic features of the joint, such as shape of the joint spaces and the configuration of the disc in its different mediolateral sections. Perforation between the lower and upper joint spaces is best diagnosed with the help of single-contrast, lower-compartment arthrography, because contrast overflows from the lower joint space into the upper one.
Computed Tomography
Direct sagittal images (see the images below) and axial images of the TMJ allow noninvasive imaging of osseous and soft-tissue abnormalities related to disc damage and dysfunction. [16, 17, 18, 19] High-resolution CT scanning can depict bony and soft-tissue changes that are not detectable using conventional radiography. CT scan attenuation values have been used as a diagnostic approach to delineating tissues of different densities.
For assessment of bone detail, CT scanning is a superior imaging method, because it is not subject to the projectional limitations of conventional radiography. Multiplanar reconstructions allow superior morphologic analyses of the osseous joint structures. Computer-generated analysis and displays of 3-D imaging data are available in conjunction with CT scanning. CT scanning does not visualize the disc directly but shows osseous changes that are nonspecific, such as joint space narrowing and changes of osteoarthritis secondary to meniscus abnormalities. CT scanning does not differentiate osteoarthritis resulting from meniscal dysfunction from other types of arthritides.
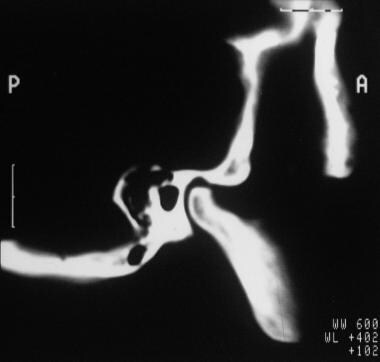 Sagittal CT cut through the temporomandibular joints examined on a bone window, elegantly demonstrating the right and left temporomandibular joints.
Sagittal CT cut through the temporomandibular joints examined on a bone window, elegantly demonstrating the right and left temporomandibular joints.
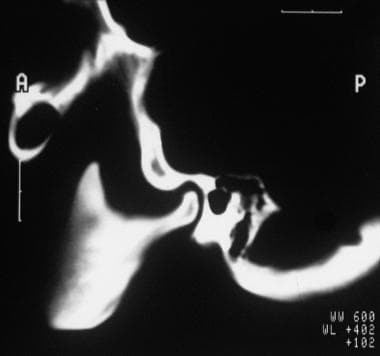 Sagittal CT cut through the temporomandibular joints examined on a bone window, elegantly demonstrating the right and left temporomandibular joints (same patient as in the previous image).
Sagittal CT cut through the temporomandibular joints examined on a bone window, elegantly demonstrating the right and left temporomandibular joints (same patient as in the previous image).
In assessment of bone detail, CT scanning is a superior imaging method, because it is not subject to the projectional limitations of conventional radiography (see the images below). Multiplanar reconstructions provide superior morphologic evaluation of the osseous joint structures. Computer-generated analysis and displays of 3D imaging data are available in conjunction with CT scanning. Direct sagittal imaging and axial imaging with parasagittal reconstruction have been described as useful in the assessment of TMJ internal derangement.
 Coronal 5-mm CT cut through the anterior cranial fossa and sinuses showing a right maxillary tumor invading the lateral sinus wall and destroying the right ramus and condyle of the mandible.
Coronal 5-mm CT cut through the anterior cranial fossa and sinuses showing a right maxillary tumor invading the lateral sinus wall and destroying the right ramus and condyle of the mandible.
 Coronal 5-mm CT cut through the anterior cranial fossa and sinuses showing a right maxillary tumor invading the lateral sinus wall and base of the anterior cranial fossa and destroying the right ramus and condyle of the mandible. Note the brain invasion (small arrow).
Coronal 5-mm CT cut through the anterior cranial fossa and sinuses showing a right maxillary tumor invading the lateral sinus wall and base of the anterior cranial fossa and destroying the right ramus and condyle of the mandible. Note the brain invasion (small arrow).
 Coronal 5-mm CT cut through the anterior cranial fossa and maxillary antra showing a right maxillary tumor invading the lateral sinus wall and eroding the right ramus and condyle of the mandible (arrow). The right condyle is no longer articulating at the mandibular fossa.
Coronal 5-mm CT cut through the anterior cranial fossa and maxillary antra showing a right maxillary tumor invading the lateral sinus wall and eroding the right ramus and condyle of the mandible (arrow). The right condyle is no longer articulating at the mandibular fossa.
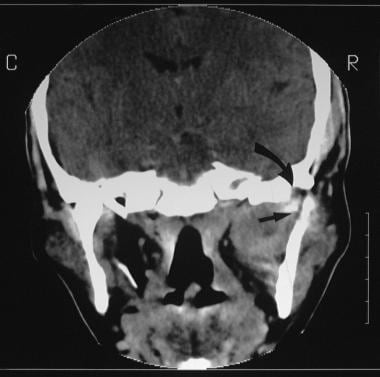 Coronal 5-mm CT cut through the anterior cranial fossa and the maxillary antra showing a right maxillary tumor invading the lateral sinus wall and eroding the right ramus and condyle of the mandible. Note the erosion and fragmentation of the right mandible (arrow). The right condyle is no longer articulating at the mandibular fossa.
Coronal 5-mm CT cut through the anterior cranial fossa and the maxillary antra showing a right maxillary tumor invading the lateral sinus wall and eroding the right ramus and condyle of the mandible. Note the erosion and fragmentation of the right mandible (arrow). The right condyle is no longer articulating at the mandibular fossa.
For the assessment of internal derangement, the angle between the condylar head and the glenoid fossa is examined closely on each scan. The ability of direct sagittal CT scanning to evaluate osseous structures is an important advantage of the technique. Diagnosis of degenerative joint disease is based on the criteria of bone erosion, eburnation, fragmentation, remodeling of the articular eminence or condylar head, and osteophyte formation.
Magnetic Resonance Imaging
MRI is the diagnostic modality of choice for most disorders of the temporomandibular joint (TMJ). The first step in MR imaging of the TMJ is evaluation of the articular disc, or meniscus, regarding morphologic features and location relative to the condyle in both the closed-mouth position and the open-mouth position. A displaced disc is a critical sign of TMJ dysfunction. [1, 4, 5, 6, 29, 30, 31]
Routine examination of the TMJ consists of conventional spin-echo, T1-weighted coronal, sagittal, and axial MRI scans, as well as fast spin-echo, T2-weighted axial images in the closed-mouth position. Fat-suppressed proton density (PD) and 2-dimensional (2D)–gradient, refocused-echo (2D-GRE) sagittal images are performed in the sagittal plane in the open and closed position to look at the meniscus. Some investigators use cephalometrically corrected sagittal images by obtaining images in an oblique plane that is perpendicular to the horizontal long axis of the condyle.
MRI yields superb images of the TMJ, and disc morphology is demonstrated elegantly (see the image below).
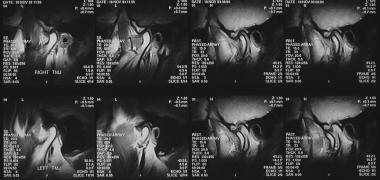 Phased-array temporomandibular joint coil with right and left temporomandibular joint images acquired simultaneously. Cine acquisition shows the temporomandibular joints from the closed to open positions in a volunteer patient.
Phased-array temporomandibular joint coil with right and left temporomandibular joint images acquired simultaneously. Cine acquisition shows the temporomandibular joints from the closed to open positions in a volunteer patient.
MRI of the TMJ is especially helpful in the following:
-
Determination of position, function, and form of the disc
-
Differential diagnosis of facial pain of uncertain etiology
-
Differential diagnosis of headache aggravated by jaw function
Internal derangement (ie, disc displacement or deformation) and degenerative joint disease are the most common findings in patients with TMJ dysfunction (see the images below); however, other abnormalities (eg, joint effusion, bone marrow edema, tumors) also may be detected. [21]
 Coronal T1-weighted MRI sequence through the left temporomandibular joint of a 37-year-old man previously treated conservatively for a left meniscus dysfunction. Flattening and sclerosis of the mandibular condyle (c) is noted but no meniscus is identified as a result of automeniscectomy (confirmed on sagittal T1-weighted scans).
Coronal T1-weighted MRI sequence through the left temporomandibular joint of a 37-year-old man previously treated conservatively for a left meniscus dysfunction. Flattening and sclerosis of the mandibular condyle (c) is noted but no meniscus is identified as a result of automeniscectomy (confirmed on sagittal T1-weighted scans).
 Sagittal T1-weighted MRI image through the left temporomandibular joint showing an anterior disk displacement (open mouth) without recapture of the meniscus (closed mouth). A small arrow has marked the meniscus.
Sagittal T1-weighted MRI image through the left temporomandibular joint showing an anterior disk displacement (open mouth) without recapture of the meniscus (closed mouth). A small arrow has marked the meniscus.
 Sagittal T1-weighted MRI image through the left temporomandibular joint showing an anterior disk displacement (open mouth) without recapture of the meniscus (closed mouth). A small arrow has marked the meniscus.
Sagittal T1-weighted MRI image through the left temporomandibular joint showing an anterior disk displacement (open mouth) without recapture of the meniscus (closed mouth). A small arrow has marked the meniscus.
MRI clearly demonstrates postoperative granulation tissue, joint effusion, and marrow edema; it also directly visualizes disc implants. However, following disc plication or discoplasty, clinical findings and MRI appearances correlate poorly. Failed implants resulting from foreign-body reaction are visualized as bone erosions similar to septic arthritis and RA. Plain radiographs are useful in differentiating joint calcification from the hypo-intense, postoperative scar and in distinguishing remodeling following surgery for OA.
Degree of confidence
Multiple clinical and experimental studies have shown a high diagnostic accuracy for MRI in the assessment of position and form of the disc. In a study by Kumar et al of 22 symptomatic patients, disc displacement was found in 18 (82%). Disc displacement on MRI correlated well with the presence or absence of clinical signs and symptoms of temporomandibular disorders, with a sensitivity of 90% and a specificity of 83.3%. [1]
Maizlin et al performed MRIs on 144 TMJs (in 72 patients), and disc displacement was found in 45 (54%) of the 84 symptomatic joints and 13 (22%) of the 60 asymptomatic joints. Of the 84 symptomatic joints, 31 (37%) had disc displacement with reduction and 14 (17%) had disc displacement without reduction. [6]
Gil et al evaluated 148 TMJs (74 symptomatic patients) using MRI for bone changes in the condyle, articular eminence, and glenoid fossa in relation to the position of the articular disc and found that disc displacement without reduction was present in 34 (23%) and disc displacement with reduction was present in 19 (12.8%). The combination of erosion and osteophytosis in the condyle and the bone changes of the posterior aspect of the articular eminence were associated with disc position. No bone changes were found in the glenoid fossa of the temporal bone. One had posterior displacement. [29]
Multisection analysis in the sagittal and coronal plane has been reported to increase MRI sensitivity, particularly in distinguishing the correct disc position from disc displacement. [32]
MRI is helpful in demonstrating TMJ arthropathies, such as joint effusion, pannus formation, and the morphology and position of the meniscus. MRI is also useful in the diagnosis of miscellaneous conditions, such as synovial chondromatosis and ganglion cysts. In synovial chondromatosis of the TMJ, MRI usually shows a large joint effusion and calcified loose bodies that are seen as foci of signal void. Ganglion cysts are demonstrated as low-signal masses on T1-weighted sequences and as high-signal cystic structures on T2-weighted sequences in close association with the TMJ.
Nuclear Imaging
Radionuclide bone scanning can detect the early changes in the temporomandibular joint (TMJ) that affect the adjacent bones and that may occur in meniscus abnormalities (see the first image below). [33] The TMJ is ideally suited for single-photon emission CT (SPECT) scanning, because it is small and lies close to the base of the skull and the paranasal sinuses. SPECT imaging can effectively produce high-quality images of the TMJ isolated from other high bone density areas, which is not possible on planar images (see the second and third images below).
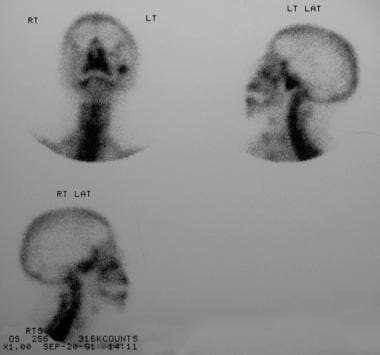 Frontal and lateral (right and left) radionuclide images of the skull showing intense activity in the left temporomandibular joint in a 41-year-old woman with an MRI-confirmed temporomandibular joint meniscus dysfunction.
Frontal and lateral (right and left) radionuclide images of the skull showing intense activity in the left temporomandibular joint in a 41-year-old woman with an MRI-confirmed temporomandibular joint meniscus dysfunction.
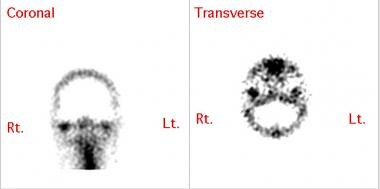 Coronal and transaxial sections generated after single-photon emission computed tomography imaging in a patient with right temporomandibular joint ankylosis. Increased uptake is seen in the right temporomandibular joint region in both sections.
Coronal and transaxial sections generated after single-photon emission computed tomography imaging in a patient with right temporomandibular joint ankylosis. Increased uptake is seen in the right temporomandibular joint region in both sections.
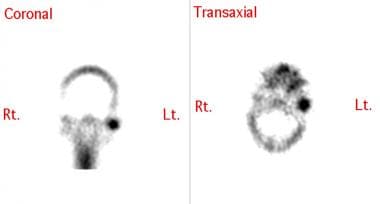 Coronal and transaxial sections generated after single-photon emission computed tomography imaging in a patient with left temporomandibular joint ankylosis. Increased uptake is seen in the left temporomandibular joint region in both sections.
Coronal and transaxial sections generated after single-photon emission computed tomography imaging in a patient with left temporomandibular joint ankylosis. Increased uptake is seen in the left temporomandibular joint region in both sections.
Subsequently, the TMJ may be studied by one of the following techniques:
-
The 3-phase technique is composed of a 30-second perfusion study in which images are obtained every 3 seconds with computed analysis of perfusion, immediate soft-tissue views of the head and anterior or lateral projections with the mouth open and closed, and delayed views of the TMJ
-
Delayed views of the TMJ are SPECT scans, as well as planar views in anterior, posterior, and both lateral projections
Radionuclide findings include the following:
-
Abnormal activity on flow studies in the TMJ is seen in patients in whom disease has an inflammatory component; the activity reflects increased perfusion and hyperemia in the joint.
-
Usually, images also demonstrate an abnormal increase in activity on immediate views.
-
Increased activity on delayed views may vary from mildly to markedly increased.
-
SPECT scanning has exquisite sensitivity in the detection of abnormally increased uptake in the TMJ, which can be quantified. The primary disadvantage of SPECT scanning is that it is a nonanatomic examination.
-
Although a region of increased uptake suggesting repair phenomena or abnormal stresses on the TMJ can be readily diagnosed, the cause of these findings may remain obscure. Mechanical internal derangement, OA, infection, and a host of other arthropathies demonstrate the same finding.
-
Usually, condylar hyperplasia is a slowly developing enlargement of the condyle and condylar neck that results in malocclusion and facial asymmetry. Disturbances in the growth pattern of a condyle during the normal growth period or during adulthood may result in condylar hyperplasia. Radionuclide imaging of the TMJ is also performed to exclude active condylar growth in patients with condylar hyperplasia. The objective is to determine whether the condylar growth has ceased or is still progressing. This helps in planning the extent of orthognathic surgery. If the condition is progressive, the entire condyle and neck may be removed; otherwise, the enlarged condyle is only trimmed.
Degree of confidence
Radionuclide bone scanning using 99mTc MDP/HMDP is extremely sensitive in detecting bone pathology. TMJ meniscus abnormalities are bound to affect the underlying bone metabolically. In the authors' studies (unpublished data), a sensitivity of 68.75% and a specificity of 61.88% were found in the detection of TMJ meniscus abnormalities. These results can be improved considerably—to a sensitivity of 100% and a specificity of 83.33%— using SPECT scanning and semiquantitative methods. Planar imaging, which usually is combined with SPECT scanning, can also show other lesions that may mimic TMJ meniscus abnormalities and cause referred pain to the TMJ, such as upper cervical spine OA, bone metastases, and dental and sinus pathology.
Although the sensitivity of radionuclide imaging is high, its specificity is low. Usually, any inflammatory/traumatic/neoplastic lesion demonstrates increased isotope uptake, which is an advantage and a disadvantage.
-
Anteroposterior projection skull radiograph showing an osteoma (O) involving the right temporal bone and the temporomandibular joint.
-
Conventional tomogram of the right temporomandibular joint showing a normal joint. Note that the bony detail is visualized well.
-
Conventional tomogram of the right temporomandibular joint showing a normal joint. Note that the bony detail is visualized well (same patient as in the previous image).
-
Tomogram through the left temporomandibular joint showing osteopenia with minor remodeling. Both sides were examined with the mouth open and closed. Note the limitation of movement on both sides.
-
Tomogram through the left temporomandibular joint showing osteopenia with minor remodeling. Both sides were examined with the mouth open and closed. Note the limitation of movement on both sides.
-
Sagittal CT cut through the temporomandibular joints examined on a bone window, elegantly demonstrating the right and left temporomandibular joints.
-
Sagittal CT cut through the temporomandibular joints examined on a bone window, elegantly demonstrating the right and left temporomandibular joints (same patient as in the previous image).
-
Coronal 5-mm CT cut through the anterior cranial fossa and sinuses showing a right maxillary tumor invading the lateral sinus wall and destroying the right ramus and condyle of the mandible.
-
Coronal 5-mm CT cut through the anterior cranial fossa and sinuses showing a right maxillary tumor invading the lateral sinus wall and base of the anterior cranial fossa and destroying the right ramus and condyle of the mandible. Note the brain invasion (small arrow).
-
Coronal 5-mm CT cut through the anterior cranial fossa and maxillary antra showing a right maxillary tumor invading the lateral sinus wall and eroding the right ramus and condyle of the mandible (arrow). The right condyle is no longer articulating at the mandibular fossa.
-
Coronal 5-mm CT cut through the anterior cranial fossa and the maxillary antra showing a right maxillary tumor invading the lateral sinus wall and eroding the right ramus and condyle of the mandible. Note the erosion and fragmentation of the right mandible (arrow). The right condyle is no longer articulating at the mandibular fossa.
-
Phased-array temporomandibular joint coil with right and left temporomandibular joint images acquired simultaneously. Cine acquisition shows the temporomandibular joints from the closed to open positions in a volunteer patient.
-
Coronal T1-weighted MRI sequence through the left temporomandibular joint of a 37-year-old man previously treated conservatively for a left meniscus dysfunction. Flattening and sclerosis of the mandibular condyle (c) is noted but no meniscus is identified as a result of automeniscectomy (confirmed on sagittal T1-weighted scans).
-
The right mandibular condyle (c) appears normal and the normal meniscus is seen clearly (arrow).
-
Sagittal T1-weighted MRI image through the left temporomandibular joint showing an anterior disk displacement (open mouth) without recapture of the meniscus (closed mouth). A small arrow has marked the meniscus.
-
Sagittal T1-weighted MRI image through the left temporomandibular joint showing an anterior disk displacement (open mouth) without recapture of the meniscus (closed mouth). A small arrow has marked the meniscus.
-
Frontal and lateral (right and left) radionuclide images of the skull showing intense activity in the left temporomandibular joint in a 41-year-old woman with an MRI-confirmed temporomandibular joint meniscus dysfunction.
-
Coronal and transaxial sections generated after single-photon emission computed tomography imaging in a patient with right temporomandibular joint ankylosis. Increased uptake is seen in the right temporomandibular joint region in both sections.
-
Coronal and transaxial sections generated after single-photon emission computed tomography imaging in a patient with left temporomandibular joint ankylosis. Increased uptake is seen in the left temporomandibular joint region in both sections.