Practice Essentials
Lymphoma is a descriptive term for malignancy of lymphoreticular cells of specific lineage (T cells, B cells, and histiocytes), in which the malignant lymphocytes crowd the normal, healthy cells in bone marrow and cause the lymph nodes to enlarge (see the images below). This disease is divided into Hodgkin disease (HD) and non-Hodgkin lymphoma (NHL). Non-Hodgkin lymphomas account for 90% of all lymphomas, while HD constitutes the remaining 10%. [1] The thorax is involved in 85% of all cases of HD and 45% of all cases of NHL.
Unlike HD, NHL has many subtypes. Diffuse large B-cell lymphoma (DLBCL) is the most common subtype, representing 25-30% of all lymphomas. DLBCL tends to be aggressive and often involves the lung. Extranodal marginal zone lymphoma (EMZL) of mucosa-associated lymphoid tissue (MALT) is another subtype that commonly affects the lung. [1, 2] The patient's prognosis and treatment vary according to the type of NHL.
Preferred examination
The primary investigation of suspected lung and mediastinal pathology is standard chest radiography. After a mediastinal lesion is identified on a conventional radiograph, CT scanning is the preferred modality for further evaluation of the middle and anterior mediastinum. MRI is preferred when neural involvement is suspected, and then imaging is generally limited to the spine. [3, 4, 5, 6, 7]
Abdominal disease is demonstrable on ultrasonograms. However, CT scanning is commonly used to show the presence and extent of disease. Visceral involvement may be diffuse or focal, with multiple nodules or sometimes a large, solitary mass present. If symptoms indicate osseous involvement, conventional radiographs may depict areas of destruction, periosteal new-bone formation, and a sclerotic lesion (in some cases). Vertebral lesions are best evaluated with MRI, particularly when vertebral collapse has occurred. MRI provides elegant demonstration of surrounding soft tissue involvement and intraspinal disease if present. MRI has a role in select cases for follow-up and for differentiation of fibrosis from disease, but if the signal intensity remains high, differentiation may be impossible, and positron emission tomography (PET) is better. In cases of central nervous system (CNS) involvement, MRI is preferred and should be used for evaluation. MRI is a valuable tool in the setting of a residual mass after treatment, giving clinically useful information for prognosis. [8] Similarly, testicular ultrasonography (US) can be performed if it is clinically applicable. [3, 5]
Isotope studies with gallium are rarely used. Gallium-67 (67Ga) scintigraphy has a sensitivity of 85% for high-grade NHL. Its sensitivity for low-grade NHL is poor. Ga-67 scintigraphy can be used to monitor responses to treatment. Where available, fluorodeoxyglucose (FDG)-PET scanning is increasingly used to image and stage malignancy. Compared with cross-sectional morphologic imaging, FDG-PET has several advantages. FDG-PET depends on metabolic abnormalities in cancer tissue and not on size criteria, as CT scanning does. It also provides a complete body survey, which is important in evaluating a multifocal disease process such as NHL. FDG-PET provides superior lesion contrast, allowing for easy detection, and the tomograms enable good anatomic localization. Whole-body FDG-PET followed by conventional imaging techniques of areas of abnormal radionuclide uptake is more cost-effective than are conventional staging methods. PET/CT has increasingly been used in staging NHL, although its availability remains limited. [4, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19]
 Posteroanterior (PA) chest radiograph in a man with thoracic non-Hodgkin lymphoma (NHL) shows mediastinal widening due to grossly enlarged right paratracheal and left paratracheal nodes.
Posteroanterior (PA) chest radiograph in a man with thoracic non-Hodgkin lymphoma (NHL) shows mediastinal widening due to grossly enlarged right paratracheal and left paratracheal nodes.
 Posteroanterior (PA) chest radiograph in a 16-year-old male adolescent with thoracic non-Hodgkin lymphoma (NHL) shows subtle enlargement of the lower paratracheal lymph nodes.
Posteroanterior (PA) chest radiograph in a 16-year-old male adolescent with thoracic non-Hodgkin lymphoma (NHL) shows subtle enlargement of the lower paratracheal lymph nodes.
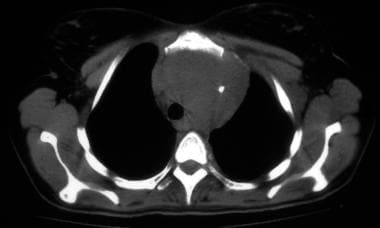
 Nonenhanced CT scan through the mediastinum at the level of the carina shows enlarged tracheobronchial and subcarinal nodes. Note the small bilateral pleural effusion.
Nonenhanced CT scan through the mediastinum at the level of the carina shows enlarged tracheobronchial and subcarinal nodes. Note the small bilateral pleural effusion.
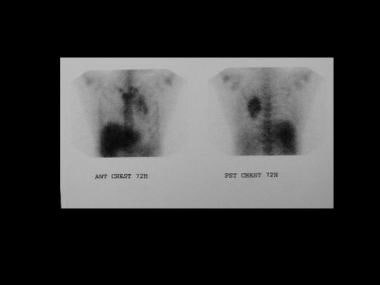
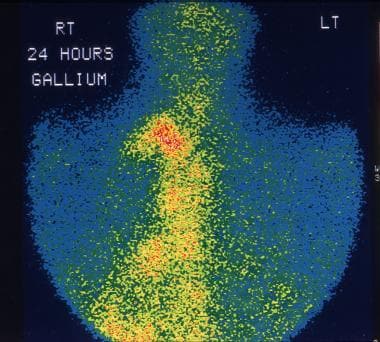 This 28-year-old man was being evaluated for fever of unknown origin. Gallium-67 study shows extensive uptake in the mediastinal lymph nodes due to non-Hodgkin lymphoma (NHL).
This 28-year-old man was being evaluated for fever of unknown origin. Gallium-67 study shows extensive uptake in the mediastinal lymph nodes due to non-Hodgkin lymphoma (NHL).
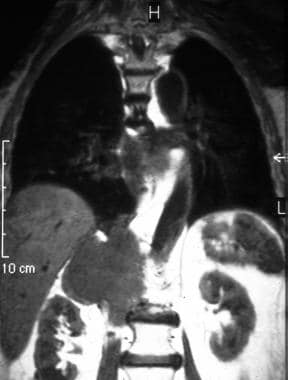 T1-weighted coronal MRIs of the thorax in a 55-year-old woman with lower dorsal pain (same patient as in the previous image). Note the signal-intensity changes in the body of D12; these are associated with a right-sided, large, paravertebral soft-tissue mass involving the psoas muscle. Biopsy confirmed non-Hodgkin lymphoma (NHL).
T1-weighted coronal MRIs of the thorax in a 55-year-old woman with lower dorsal pain (same patient as in the previous image). Note the signal-intensity changes in the body of D12; these are associated with a right-sided, large, paravertebral soft-tissue mass involving the psoas muscle. Biopsy confirmed non-Hodgkin lymphoma (NHL).
 A PA chest radiograph in a 28-year-old woman who presented with weight loss, showing a cavitating lesion (mimicking tuberculosis) in the left midzone adjacent to the left hilum. Histology confirmed a large-cell NHL.
A PA chest radiograph in a 28-year-old woman who presented with weight loss, showing a cavitating lesion (mimicking tuberculosis) in the left midzone adjacent to the left hilum. Histology confirmed a large-cell NHL.
Classification of NHL
NHL tumors include the following:
Low-grade NHL tumors
-
Small lymphocytic tumors (lymphocytic and well-differentiated in the Rappaport classification)
-
Follicular predominantly small cleaved-cell (nodular, poorly differentiated lymphocytes) tumors
-
Follicular mixed and large cleaved-cell (nodular, [mixed] lymphocytic and histiocytic) tumors
Intermediate-grade NHL tumors
-
Follicular predominantly large-cell (nodular, histiocytic) tumors
-
Diffuse small cleaved cell (diffuse, poorly differentiated, lymphocytic) tumors
-
Diffuse (mixed) large- and small-cell (diffuse, [mixed] lymphocytic and histiocytic) tumors
-
Diffuse large-cell (diffuse, histiocytic) tumors
High-grade NHL tumors
-
Large-cell, immunoblastic (diffuse, histiocytic) tumors
-
Lymphoblastic (lymphoblastic lymphoma) tumors
-
Small noncleaved (undifferentiated Burkitt and non-Burkitt) tumors
Miscellaneous NHL tumors
-
Composite
-
Mycosis fungoides
-
Histiocytic
-
Unclassified
Follicular tumors are less aggressive and more widespread than are other tumors. Follicular tumors have a higher relapse rate and may undergo transformation into a more aggressive histology, whereas diffuse tumors are more aggressive and localized and have lower relapse rate. Most mediastinal tumors are of the diffuse and poorly differentiated lymphocytic type. Although this type is localized at presentation, its presence implies disseminated disease.
Staging of lymphomas
Lymphomas are staged by using the Ann Arbor system, as follows:
-
Stage I - The tumor involves only 1 lymph node region, organ, or other site
-
Stage II - The tumor involves 2 or more lymph node regions on the same side of the diaphragm, an organ and lymph nodes in the same half of the body, or another site and lymph nodes in the same half
-
Stage III - The tumor involves lymph node regions and/or the spleen (and on both sides of the diaphragm): Stage III (1) - the tumors are above the renal vessels; Stage III (2) - the tumors are in the lower abdomen.
-
Stage IV - The tumor is extranodal, with diffuse involvement of nonlymphatic organs or tissues (eg, bone, marrow, lung, liver): Stage IV A - constitutional symptoms are absent; Stage IV B - constitutional symptoms are present
Limitations of techniques
The appearances of a mediastinal mass on chest radiographs are nonspecific, with a wide differential diagnosis, and the differentiation of benign and malignant lesions may not be possible. Subtle bone erosions can be missed on conventional radiographs. Underlying masses with pleural and pericardial effusions may not be detected. Fat attenuation in benign lesions may be obscured with tumor hemorrhage or rupture, and a false diagnosis of malignant lesion can be made. A standard PA chest radiograph may be difficult to obtain in ill patients and in young children with mediastinal magnification obscuring anterior mediastinal masses, as shown on anteroposterior (AP) radiographs.
Although CT scanning is the examination of choice in the assessment of mediastinal masses, at best, the findings only suggest the diagnosis of NHL. A tissue diagnosis is required. CT scanning can be invasive, and young patients may require sedation or a general anesthetic. In addition, CT scanning is expensive and exposes the patient to radiation. Moreover, patients may be allergic to iodinated contrast medium, which must be used with caution in persons with renal failure.
MRI provides better contrast resolution than do other studies, but biopsy is often required for a definitive diagnosis. [20] MRI is expensive and not universally available, and patients with claustrophobia and young children may need sedation or general anesthesia. MRI cannot be used with certain types of metallic implants or clips, with cardiac pacemakers, or with ferromagnetic foreign bodies. Image-guided biopsy may require more expensive, MRI-compatible equipment.
US is operator dependent, and access to the anterior mediastinum may be difficult because of the thoracic bony cage and lungs. US cannot be used to evaluate the lungs.
Although radionuclide scans are more tissue specific than are other studies, it has a potential for false-positive results, and uptake may occur in a variety of normal, inflammatory, and neoplastic tissues.
FDG-PET is expensive, currently has limited availability, and requires prolonged acquisition times. Sites with normal physiologic activity may contribute to false results, although this appears to be less of a problem than it is with 67Ga imaging. Persistent FDG uptake in a residual mass should prompt strong consideration of additional therapy, although occasionally, uptake may be related to thymic hyperplasia or a histiocytic reaction.
Intervention
Image-guided biopsy (with US, conventional radiography, or CT scanning) conducted using fine-needle aspiration (FNA) or core-needle techniques is considered safe and is increasingly used in preference to a surgical biopsy. Interpretation of FNA results needs an expert cytopathologic opinion. Differentiation of various types of mediastinal tumors, such as thymomas, lymphomas, and germ cell tumors, is possible when core-needle biopsy material is subjected to special histologic staining, including immunohistochemical techniques.
Radiography
Radiologically, the appearance of intrathoracic involvement in NHL is generally similar to that of HD (see the images below). Pulmonary parenchymal involvement and mediastinal lymphadenopathy are less common manifestations of NHL than they are of HD. The pattern of pulmonary disease varies with the histologic type of NHL. A mediastinal mass as a presenting feature of NHL occurs in approximately 20% of cases.
 Posteroanterior (PA) chest radiograph in a man with thoracic non-Hodgkin lymphoma (NHL) shows mediastinal widening due to grossly enlarged right paratracheal and left paratracheal nodes.
Posteroanterior (PA) chest radiograph in a man with thoracic non-Hodgkin lymphoma (NHL) shows mediastinal widening due to grossly enlarged right paratracheal and left paratracheal nodes.
 Posteroanterior (PA) chest radiograph shows a large mass in the right parahilar region extending into the right upper and middle zones, with silhouetting of the right pulmonary artery. Smaller mass is seen in the periphery of the right lower zone. The masses did not respond to a trial of antibiotics. Core-needle biopsy of the larger lesion revealed NHL deposits in the lung.
Posteroanterior (PA) chest radiograph shows a large mass in the right parahilar region extending into the right upper and middle zones, with silhouetting of the right pulmonary artery. Smaller mass is seen in the periphery of the right lower zone. The masses did not respond to a trial of antibiotics. Core-needle biopsy of the larger lesion revealed NHL deposits in the lung.
 Tomogram of the right lower chest wall demonstrates the lesion better than previous image in this patient with non-Hodgkin lymphoma (NHL) of the ribs.
Tomogram of the right lower chest wall demonstrates the lesion better than previous image in this patient with non-Hodgkin lymphoma (NHL) of the ribs.
 Anteroposterior (AP) view shows a collapsed vertebra in a patient with non-Hodgkin lymphoma (NHL) of the thoracic vertebrae.
Anteroposterior (AP) view shows a collapsed vertebra in a patient with non-Hodgkin lymphoma (NHL) of the thoracic vertebrae.
 Image shows a right-sided, hemorrhagic pleural effusion. Cytologic and pleural biopsy results confirmed non-Hodgkin lymphoma (NHL).
Image shows a right-sided, hemorrhagic pleural effusion. Cytologic and pleural biopsy results confirmed non-Hodgkin lymphoma (NHL).
 Lateral myelogram shows abrupt tapering of thecal sac caused by compression of soft tissue associated with the lymphomatous deposit in the thoracic vertebrae.
Lateral myelogram shows abrupt tapering of thecal sac caused by compression of soft tissue associated with the lymphomatous deposit in the thoracic vertebrae.
Most common types of mediastinal NHL
The most common types of NHL to involve the mediastinum are large–B-cell lymphoma and lymphoblastic lymphoma. Parenchymal lung infiltration may occur in around 5% of cases, but this may be found without associated mediastinal lymphadenopathy. [21]
The plain radiographic finding of parenchymal lung involvement is also identical to that seen in HD. Multiple nodules are the most common features, but poorly defined opacification with an air bronchogram may also be seen. Features indistinguishable from pneumonic change, such as bilateral airspace consolidation and segmental or lobar atelectasis, are less common. Arora and colleagues reported on an uncommon case of diffuse histiocytic lymphoma that occurred with pulmonary miliary mottling that responded well to chemotherapy. [22]
Most histologic types of lymphoma can involve the mediastinum. However, some lymphomas have a predilection for the mediastinum; these include the following:
-
Nodular sclerosis HD - Classically seen in young women
-
Lymphoblastic lymphoma - Occurs in children and can grow rapidly
-
Diffuse large-cell type of lymphoma - Can occur at any age
While it is true that large-cell NHL favors the anterior mediastinum, follicular low- or intermediate-grade NHL, as well as high-grade NHL, can involve nodes anywhere in the chest and axillae.
If local symptoms indicate bone involvement, radiographs of the area may reveal areas of destruction, periosteal new-bone formation, and (occasionally) sclerotic lesions.
Pleural disease
NHL may extend into the pleural space by means of direct extension from contiguous chest-wall involvement or lung parenchymal disease. Pleural involvement in NHL (similar to that in HD) is characterized by nodular or plaquelike subpleural deposits of lymphomatous tissue or a pleural effusion due to obstruction of the lymphatics, pulmonary veins, or thoracic duct. Alternatively, it is a result of direct pleural invasion. Primary pleural lymphoma is rare and is usually associated with mediastinal or lung parenchymal disease, although disease recurrence is occasionally confined to the pleura.
Pleural effusions are seen on chest radiographs in up to 25% of patients with lymphoma at presentation; on CT scans, they are seen in an even higher percentage of patients. Individuals with large mediastinal masses are particularly prone to pleural effusions. Most pleural effusions associated with lymphomas are small, unilateral, and exudative. These generally resolve promptly with treatment. A chylothorax can be caused by lymphatic obstruction and would be slow to resolve.
Dunnick and colleagues described the radiographic manifestations of Burkitt lymphoma in 40 American patients. Pleural effusions were found to be the most common intrathoracic abnormality; they were correlated with abdominal ascites more frequently than they were with intrathoracic tumors. [23]
Thoracic wall disease
Invasion of the thoracic wall as a direct extension from mediastinal disease is more common in NHL, although primary involvement of the thoracic wall may occur. Thoracic wall involvement may appear as a destructive rib or vertebral-body lesion with a surrounding soft-tissue mass.
Recurrent disease
Recurrent disease after treatment tends to occur at the initial site of presentation. On plain radiographs and CT scans, recurrent disease appears as nodular opacities or attenuations, as ill-defined parahilar opacities or attenuations, or as large, masslike lesions in the lung. Paracardiac or diaphragmatic lymphadenopathy is a relatively common feature of recurrent disease; this is particularly the case in HD, because these lymph nodes are not included in the mantle radiation treatment field.
Recurrence in previously irradiated intrathoracic lymph nodes, although uncommon, may occur, particularly in patients with initially large mediastinal masses. In most patients with recurrent NHL, relapse ensues within 2 years of completion of treatment. Plain radiographs and/or CT scans show an increase in the size of one or more masses.
Degree of confidence
Despite major advances in cross-sectional imaging, conventional chest radiography retains a major role in the initial diagnosis of mediastinal masses and of lung parenchymal and/or pleural disease. It guides the clinician regarding what to evaluate next in the patient with a mediastinal mass and lung and/or pleural disease. The standard chest radiograph is universally available, noninvasive, and inexpensive. In addition, it has a low radiation dose.
False positives/negatives
As with any other anatomic imaging, the appearances of an anterior mediastinal mass and many of the lung/pleural lesions are nonspecific, with a wide differential diagnosis. Differentiation between benign and malignant lesions may not be possible. CT scanning is superior to radiography for depicting calcification and obliteration of fat planes, mediastinal lymphadenopathy, and bone erosions. Most patients with anterior mediastinal masses are referred for a CT scan. PET/CT scanning may be more commonly used depending on availability.
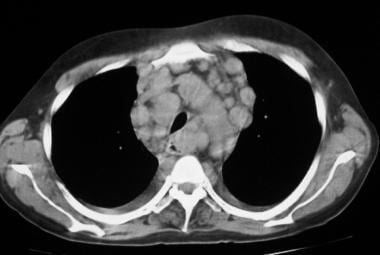
Computed Tomography
Computed tomography is the preferred imaging method for diagnosing mediastinal, lung parenchymal, and pleural disease (see the images below). Protocols for staging lymphoma include CT scanning of the neck, thorax, abdomen, and pelvis. All mediastinal, lung, thoracic wall, and lung abnormalities (as described in NHL) are better depicted on CT than on conventional radiography. [3, 9, 24, 25, 2] CT is also useful in diagnosing benign mediastinal masses and reliably differentiating from NHL.
 Nonenhanced CT scan through the mediastinum shows multiple enlarged lymph nodes in the prevascular space, in the right and left paratracheal region. Nodes in the left paratracheal region cause the trachea to be indented and narrowed on the left side. Note the small, bilateral pleural effusion.
Nonenhanced CT scan through the mediastinum shows multiple enlarged lymph nodes in the prevascular space, in the right and left paratracheal region. Nodes in the left paratracheal region cause the trachea to be indented and narrowed on the left side. Note the small, bilateral pleural effusion.
 Contrast-enhanced axial CT scan in a child shows hypoattenuating, enlarged, subcarinal lymph nodes with splaying of the tracheal bifurcation.
Contrast-enhanced axial CT scan in a child shows hypoattenuating, enlarged, subcarinal lymph nodes with splaying of the tracheal bifurcation.
 Nonenhanced axial CT scan shows biopsy-proved non-Hodgkin lymphoma (NHL) of the thymus, which appears as a hypoattenuating mass in the anterior mediastinum. Note the tracheal displacement to the right.
Nonenhanced axial CT scan shows biopsy-proved non-Hodgkin lymphoma (NHL) of the thymus, which appears as a hypoattenuating mass in the anterior mediastinum. Note the tracheal displacement to the right.
 An axial CT scan showing an intraparenchymal cavitating lung lesion adjacent to the anterior thoracic wall.
An axial CT scan showing an intraparenchymal cavitating lung lesion adjacent to the anterior thoracic wall.
Benign anterior mediastinal masses
Benign anterior mediastinal masses are typically depicted on CT as well-marginated, lobulated, encapsulated, mixed solid and/or cystic masses. In 13% of patients with an anterior mediastinal mass, the tumor extends into the middle and posterior mediastinal compartments. Cystic areas are often multilocular and thinly septate; they are found in up to 88% of cases. Tumors are predominantly cystic in 80% of cases. About 50-73% of benign tumors have fat content, and 25-50% of tumors calcify. A fat-fluid layer may be found in up to 11% of patients. Pleural effusion can be found in up to 17% of cases, and pericardial effusion in 5%. [26]
CTA sign
The CT angiographic (CTA) sign is visualization of an enhancing vessel within the area of consolidated lung. This is described in association with bronchoalveolar cell carcinoma and may also be seen with primary pulmonary lymphoma. Cavitation of nodules is rare before treatment. Calcification is found in less than 1% of cases before treatment, but it may suggest a more aggressive lesion. Calcification can be seen in 2-8% of cases after irradiation or chemotherapy.
Liver and splenic involvement
In NHL, liver and splenic involvement is seen in 15% and 22% of patients, respectively. Infiltrative involvement of the liver, spleen, and bone marrow cannot be accurately detected with CT, as organomegaly is a poor predictor of tumor involvement. In fact, approximately 30% of patients with splenic enlargement do not have malignant involvement. Sensitivity rates for CT are 15-37% for infiltrative splenic disease and 19-33% for infiltrative liver disease.
Degree of confidence
CT is the imaging study of choice for evaluating mediastinal lesions. CT is an excellent modality in determining the exact location of the mediastinal tumor, as well as its relationship to adjacent structures. It is also useful in differentiating masses originating in the mediastinum from those encroaching on the mediastinum from the lung or other structures.
CT can be used to differentiate tissue attenuations, and it is highly accurate in differentiating fluid, fat, and calcification. CT helps in assessing the vascularity of mediastinal tumors. CT is better than other cross-sectional imaging in revealing local invasion of adjacent structures by a mass or intrathoracic metastases. Fat-fluid levels are considered highly specific in diagnosing mediastinal, mature teratomas (though these are uncommon).
Conventional imaging modalities such as CT and MRI can demonstrate only a decrease in lesion size, and the findings are poor predictors of clinical outcome after treatment for lymphoma. On long-term follow-up, less than 50% of patients with positive CT findings have disease relapse or other evidence of residual tumor.
A study by Albano et al found that pulmonary MALT lymphoma is 18F-FDG avid in most cases, 18F-FDG avidity is correlated with tumor size, and single or multiple areas of consolidation are the most common pattern of presentation of lung MALT lymphoma on CT. [2]
False positives/negatives
Although CT is highly sensitive in the diagnosis of anterior mediastinal masses, its specificity is low in terms of differentiating benign from malignant lesions and in the classification of the histologic types of malignant lesions. Lung parenchymal involvement in NHL also has a nonspecific appearance on CT and has a wide differential diagnosis.
To be detected on CT imaging, osseous involvement must be focal and associated with bone destruction. Patients with infiltrative marrow involvement have no bone destruction and are usually asymptomatic; their lesions may be difficult to detect on CT. Lastly, CT cannot be used to monitor response to treatment, as residual abnormalities that may represent nonviable fibrotic tissue are frequently detected.
Magnetic Resonance Imaging
MRI is used as a problem-solving tool in the imaging of thoracic lymphoma and is generally not used as the primary imaging modality, except for few specific indications (see the images below). Weinreb and Naidich used mediastinal MRI particularly when CT scan findings were equivocal. MRI was especially useful in evaluating cardiovascular abnormalities. Virtually the entire spectrum of aortic disease could be assessed accurately, making MRI a reasonable alternative to CT scanning or angiography in most cases. [27, 8]
In staging mediastinal malignancy, MRI is more accurate than CT scanning in assessing thoracic wall invasion. MRI has also been useful in evaluating the response to therapy in lymphoma. MRI is an excellent noninvasive modality in the assessment of superior vena cava syndrome and other venous obstructions, especially when the use of radio-iodinated intravenous contrast medium is contraindicated.
 T1-weighted coronal MRIs of the thorax in a 55-year-old woman with lower dorsal pain. Note the signal-intensity changes in the body of D12; these are associated with a right-sided, large, paravertebral soft-tissue mass involving the psoas muscle. Biopsy confirmed non-Hodgkin lymphoma (NHL).
T1-weighted coronal MRIs of the thorax in a 55-year-old woman with lower dorsal pain. Note the signal-intensity changes in the body of D12; these are associated with a right-sided, large, paravertebral soft-tissue mass involving the psoas muscle. Biopsy confirmed non-Hodgkin lymphoma (NHL).
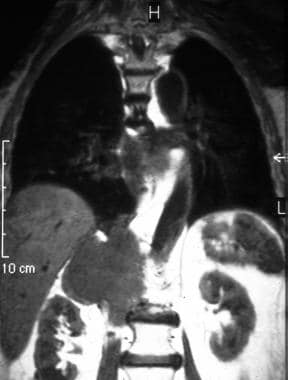 T1-weighted coronal MRIs of the thorax in a 55-year-old woman with lower dorsal pain (same patient as in the previous image). Note the signal-intensity changes in the body of D12; these are associated with a right-sided, large, paravertebral soft-tissue mass involving the psoas muscle. Biopsy confirmed non-Hodgkin lymphoma (NHL).
T1-weighted coronal MRIs of the thorax in a 55-year-old woman with lower dorsal pain (same patient as in the previous image). Note the signal-intensity changes in the body of D12; these are associated with a right-sided, large, paravertebral soft-tissue mass involving the psoas muscle. Biopsy confirmed non-Hodgkin lymphoma (NHL).
Degree of confidence
The lack of ionizing radiation and its multiplanar capability make MRI an excellent modality in the initial diagnosis of a mediastinal mass and in its follow-up after treatment. The vascular images provided are superior to CT scans and can better delineate the relationship of an identified mediastinal mass to adjacent intrathoracic vascular structures. MRI can be used to differentiate a suspected mediastinal mass and a vascular abnormality, such as an aortic aneurysm.
MRI contrast agents can be used when iodinated contrast is contraindicated. It provides increased detail in the subcarinal and aortopulmonary window areas, as well as in the inferior aspects of the mediastinum at the level of the diaphragm. MRI is preferred to CT scanning in the evaluation of invasion or extension of tumors, especially tumors closely associated with the heart. MRI is also superior to CT scanning for defining masses impinging on the thoracic inlet or at the thoraco-abdominal level. MRI better depicts recurrences in the chest wall in HD and NHL.
MRI cannot reliably depict pulmonary pathology and shares nonspecificity with other cross-sectional imaging in terms of tissue diagnosis of anterior mediastinal masses.
Ultrasonography
Although US has traditionally been used to differentiate solid from cystic masses elsewhere in the body, the study has been extended to evaluating the anterior mediastinum and to assist in determining a connection between a mass and adjacent structures. US is more useful than other studies in the evaluation of vascular abnormalities and of masses associated with the heart. In general, given the accuracy and detail provided by CT, MRI, and selected radionuclide scans, US techniques generally are not used as primary tools in the evaluation of mediastinal lymphadenopathy. [28, 29]
Although mediastinal US is rarely used in the United States to assess NHL, it might play a role in the diagnostic workup of mediastinal pathology as an adjunct technique to other imaging studies, such as conventional chest radiography, CT scanning, and MRI.
The pleural space lends itself well to ultrasonographic examination in the presence of pleural effusions. US can be used to evaluate the extent and characteristics of the effusions, as well as the presence or absence of pleural nodules and/or masses. US is an excellent tool when pleural intervention is planned.
NHL has a secondary cardiac localization in 20% of patients, but primary cardiac NHL is extremely rare, and only sporadic cases have been reported; most are diagnosed on autopsy. As a noninvasive technique, echocardiography may depict these tumors early, but the prognosis nevertheless remains poor.
Guided tumor biopsy
US can be used to perform guided tumor biopsy of the anterior mediastinum. Andersson and associates concluded that US-guided tumor biopsy of the anterior mediastinum is safe, cost-effective, and reliable, as well as a good alternative to traditional biopsy techniques employing mediastinoscopy or thoracotomy. [30] The authors performed US-guided biopsy of the anterior mediastinum in 23 patients on 28 occasions. US was chosen when CT scanning had shown the tumor to be in contact with the thoracic wall. The procedure was technically successful in all cases, and no complications occurred. In 27 of the 28 occasions, the biopsy diagnosis was identical to the final diagnosis. In 1 patient with a malignant lymphoma, a connective tissue remnant was falsely diagnosed.
Degree of confidence
Mediastinal US is an effective and inexpensive imaging method, with a higher sensitivity than that of conventional radiographs for the detection of mediastinal tumors. US is quick, accurate, noninvasive, and universally available, and it involves no ionizing radiation. The diagnostic advantage of mediastinal US over chest radiography results from its ability to demonstrate deep, central mediastinal lymph nodes long before a displacement of pleuromediastinal lines occurs.
Mediastinal US is only marginally inferior to CT scanning in the detection of supra-aortic, pericardial, and prevascular lesions (sensitivity, 98-100%), but certain compartments (eg, the posterior mediastinum and the paravertebral region) can be evaluated only with CT scanning or MRI. In addition to the assessment of size and topographic characteristics of mediastinal masses, US precisely shows the internal structure of the tumor, which may suggest a specific diagnosis when considered along with the tumor's clinical presentation and location.
US remains operator dependent, and the anterior mediastinum may not be accessible because of the thoracic bony cage. In common with cross-sectional imaging, tissue diagnosis may not be possible, because the differential diagnosis of solid, cystic, and complex mediastinal masses is wide.
Nuclear Imaging
Technetium-99m (99mTc) pertechnetate, as well as iodine-131 (131I) or iodine-123 (123I), is used to identify aberrant thyroid tissue in the anterior mediastinum, as well as goiters and thyroid neoplasms in the mediastinal thyroid gland (see the images below). Radioiodine scans are particularly useful in identifying anterior mediastinal masses at the level of the thoracic inlet, such as the substernal extension of cervical thyroid goiter. Because lymphomas and thyroid abnormalities may appear as anterior mediastinal masses, these radionuclides may help confirm or eliminate thyroid tissue as the cause of an anterior mediastinal mass. [9, 10, 11, 12, 13, 14, 15, 19]
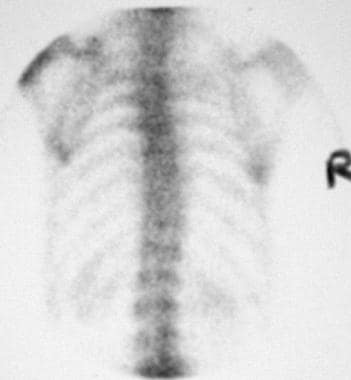 Posterior bone scan shows no abnormally increased uptake in the thoracic vertebrae. Image shows an unusual pattern of non-Hodgkin lymphoma (NHL) of the upper thoracic vertebra.
Posterior bone scan shows no abnormally increased uptake in the thoracic vertebrae. Image shows an unusual pattern of non-Hodgkin lymphoma (NHL) of the upper thoracic vertebra.
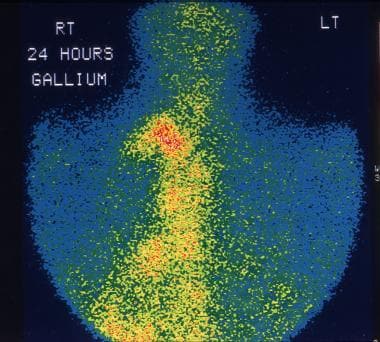 This 28-year-old man was being evaluated for fever of unknown origin. Gallium-67 study shows extensive uptake in the mediastinal lymph nodes due to non-Hodgkin lymphoma (NHL).
This 28-year-old man was being evaluated for fever of unknown origin. Gallium-67 study shows extensive uptake in the mediastinal lymph nodes due to non-Hodgkin lymphoma (NHL).
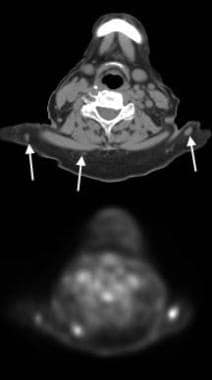 Positron emission tomography (PET) CT in an 80-year-old woman with diffuse, large B-cell NHL of the skin and subcutaneous tissues that recently transformed from prior low-grade non-Hodgkin lymphoma (NHL). CT scan of the lower neck shows several subcutaneous nodules of varying size with variable uptake on PET (arrows).
Positron emission tomography (PET) CT in an 80-year-old woman with diffuse, large B-cell NHL of the skin and subcutaneous tissues that recently transformed from prior low-grade non-Hodgkin lymphoma (NHL). CT scan of the lower neck shows several subcutaneous nodules of varying size with variable uptake on PET (arrows).
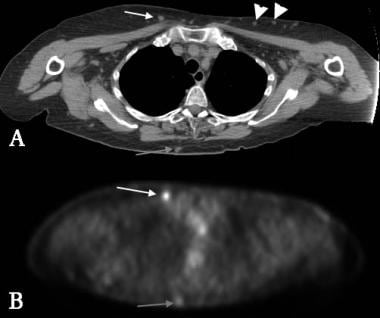 Positron emission tomography (PET) CT in an 80-year-old woman with diffuse, large B-cell NHL of the skin and subcutaneous tissues that recently transformed from previous low-grade non-Hodgkin lymphoma (NHL) in the same patient as in the previous image. PET shows high level of uptake in the anterior subcutaneous nodule in the chest (white arrows). CT scan of similar nodules (arrowheads) on the anterior left chest does not show PET uptake; these may represent regions of lower-grade NHL. PET image of posterior lesions shows only mild uptake (gray arrow).
Positron emission tomography (PET) CT in an 80-year-old woman with diffuse, large B-cell NHL of the skin and subcutaneous tissues that recently transformed from previous low-grade non-Hodgkin lymphoma (NHL) in the same patient as in the previous image. PET shows high level of uptake in the anterior subcutaneous nodule in the chest (white arrows). CT scan of similar nodules (arrowheads) on the anterior left chest does not show PET uptake; these may represent regions of lower-grade NHL. PET image of posterior lesions shows only mild uptake (gray arrow).
Indium-111
Indium-111 (111In) octreotide and pentetreotide scans may differentiate lymphomas and other mediastinal masses from mediastinal carcinoids. Carcinoids, including other neuroendocrine tumors, have somatostatin receptors and therefore can be imaged with somatostatin analogues (octreotide, pentetreotide) tagged to an appropriate radioisotope. Single-photon emission CT (SPECT) scanning and subtraction techniques improve detection.
Gallium-67
Gallium-67 scans are a valuable complement to anatomic imaging in HD and NHL in the detection of viable residual tumor after chemotherapy, as well as in the diagnosis of disease recurrence. Ga-67 scintigraphy has a high sensitivity for high-grade NHL, particularly for histiocytic lymphoma, but its sensitivity for low-grade NHL is poor. Ga-67 scintigraphy can be used to monitor response to treatment.
Thallium-201
Thallium-201 (201Tl) is of interest in differentiating cerebral lymphomas from infectious lesions in AIDS patients, but it is less useful in extracerebral lymphomas. Tl-201 has a higher avidity for low-grade NHL than does 67Ga; it therefore has a complementary role to 67Ga in the diagnosis of low-grade NHL. However, the sensitivity of 201Tl for high-grade NHL is generally poor; in this case, 67Ga scanning is the preferred imaging technique.
FDG-PET
Several studies have shown the superiority of FDG-PET scanning over 67Ga scanning in the initial diagnosis of HD and NHL, as well as in the diagnosis of recurrent HD and NHL. As many as 100% of patients with a positive PET scan after chemotherapy have an early relapse, while in more than 80% of patients with a negative PET, long-term remission occurs. Most studies indicate that FDG-PET scanning results are significantly correlated with patient outcome, whereas the correlation for CT scanning is poorer.
FDG-PET scanning does not rely entirely on lymph size, as do anatomic imaging methods, but is dependent on levels of metabolic activity, which can be high enough to visualize even some small lesions. CT scanning often cannot be used to differentiate residual disease and posttherapeutic fibrosis. On the basis of a number of clinical results, FDG-PET is gaining increasing importance for staging, restaging, and monitoring treatment responses in malignant lymphomas.
FDG-PET scanning has high sensitivity for the detection of nodal involvement in HD and NHL and generally detects activity in all abnormal lymph nodes identified on CT scans. FDG-PET scanning also has the advantage of detecting additional nodal disease, which might be missed on CT scans because of size criteria; this is particularly true for small mesenteric lymph nodes. The sensitivities reported for FDG-PET scanning in the detection of nodal disease are 62-100%; the variability is related to the fact that FDG-PET scanning's sensitivity differs according to the particular histologic grade of lymphoma that is present. Despite this range of sensitivities, FDG-PET scanning consistently has higher accuracy than CT scanning in the staging of lymphoma.
In a retrospective study of 56 patients (42 with mediastinal Hodgkin lymphoma and 14 with primary mediastinal B-cell lymphoma) to assess differences in clinical, laboratory, and FDG PET/CT metrics, lactate dehydrogenase (LDH) levels and several FDG PET/CT findings (tumor size, presence of necrosis, and degree of FDG uptake) were found to be helpful in discriminating mediastinal Hodgkin lymphoma from primary mediastinal B-cell lymphoma (PMBCL). [31]
However, another reretrospective study of FDG PET to assess response to therapy in 36 consecutive patients treated for PMBCL found that a positive interim FDG-PET/CT did not reflect persistence of active disease in the vast majority of PMBCL cases. The relapse rates were similar regardless of interim FDG-PET/CT results and interpretation criteria. [32] In NHL, extranodal disease generally worsens the prognosis. FDG-PET scanning detected 57% more extranodal sites of disease than can CT scanning.
A small study at 2 treatment sites found that coregistering FDG-PET and CT scans on treatment planning for lymphoma patients yielded changes in management, volume definition, and normal tissue dosimetry for a significant number of patients. [4]
F18 FDG-PET uptake variability within the liver and mediastinum during chemotherapy should be taken into account when this parameter is used to score the interim PET scans and to make decisions in defining response-adapted therapeutic strategies. The liver uptake increases in the interim period in comparison to a baseline study. Conversely, the stability of mediastinal uptake activity during therapy provides a more reliable benchmark for the response assessment. Finally, the intersubject’s variability of both parameters should be considered when point score models perform the visual evaluation of the interim PET. [16]
A study by Albano et al found that pulmonary MALT lymphoma is 18F-FDG avid in most cases, 18F-FDG avidity is correlated with tumor size, and single or multiple areas of consolidation are the most common pattern of presentation of lung MALT lymphoma on CT. [2]
Bone marrow involvement
Bone marrow involvement indicates stage IV disease and carries a less favorable prognosis for patients with NHL. Focal and infiltrative osseous lesions can be detected on FDG-PET imaging. Infiltrative osseous lesions show a diffuse increase in bone marrow radioactivity, which appears greater than that of the liver. Bone marrow involvement in NHL can be detected on FDG-PET scans with a sensitivity of 81-88% and a specificity of 100%. On 99mTc methylene diphosphonate (MDP) scans, osseous NHL deposits may be photon deficient, and FDG-PET scanning has been shown to be superior. FDG-PET scanning depicts up to 42% more focal osseous lesions than does 99mTc MDP bone scintigraphy.
Detection and accurate diagnosis
FDG-PET scanning can be used to differentiate between fibrosis and viable tumor. In patients with lymphoma, 30-64% have a residual mass after the completion of therapy. FDG accumulates in viable tumor, but it does not accumulate in fibrotic or necrotic tissue.
In a study by Sasaki and colleagues, the authors concluded that in the accurate detection of malignant lymphoma, FDG-PET scanning offers more information in addition to the findings of conventional diagnostic methods than does 67Ga scintigraphy. [17]
Kostakoglu and colleagues compared the accuracy of FDG-PET and 67Ga scanning in the identification of disease sites in patients with HD or with intermediate- or high-grade NHL at initial diagnosis or clinical recurrence. [18] The report indicated that in imaging aggressive lymphoma and HD before treatment, the site and patient sensitivity of FDG-PET scanning is significantly greater than that of 67Ga scintigraphy.
Preliminary results from a study by Schillaci and co-authors indicated that in untreated patients, 99mTc tetrofosmin scintigraphy effectively depicts supradiaphragmatic lymphoma lesions. [33] The report suggested that serial scintigraphic studies may be useful in the monitoring of treatment response, but it also stated that larger series would be required to better elucidate 99mTc tetrofosmin scintigraphy's possible role in such monitoring.
Degree of confidence
Ga-67 scintigraphy has a sensitivity of 85% for high-grade NHL. Sensitivity of 89% has been reported for histiocytic lymphoma. The modality's sensitivity for low-grade NHL is poor. Ga-67 scintigraphy can be used to monitor response to treatment.
Tl-201 has a higher avidity for low-grade NHL than does 67Ga. Therefore, it has a complementary role to 67Ga imaging in the diagnosis of low-grade NHL. However, the sensitivity of 201Tl for high-grade NHL is generally poor; in this case, 67Ga scintigraphy is the preferred imaging method.
FDG-PET scanning has several advantages over cross-sectional morphologic imaging. FDG-PET scanning depends on metabolic abnormalities in cancer tissue and not on size criteria, as does CT scanning. It provides a complete body survey, which is important in evaluating NHL and other multifocal disease processes.
False positives/negatives
Sarcoid anterior mediastinal lymphadenopathy may also uptake 67Ga. Ga-67-avid sarcoid disease is reported in over 90% of cases of pulmonary involvement. A lambda pattern of uptake in the parahilar, infrahilar bronchopulmonary, and mediastinal lymph nodes has been described in 72% of patients with intrathoracic sarcoidosis. Accumulation of 67Ga is a sensitive but nonspecific indicator of active inflammation in patients with sarcoidosis. Ga-67 scintigraphy is also useful in identifying extrathoracic sites of involvement, detecting active alveolitis, and assessing response to treatment.
Ga-67 uptake in the thoracic lymph nodes, the lungs, and the salivary and lacrimal glands is particularly suggestive of sarcoidosis. How well the extent of 67Ga uptake in the lung correlates with the degree of alveolitis is controversial. However, 67Ga scans may be useful as a baseline study at the time of diagnosis; if the results from 67Ga scintigraphy are initially positive, negative findings from a subsequent 67Ga scan obtained during the course of treatment suggest that alveolitis has resolved. In such a patient, 67Ga may be a useful marker for disease in activity and response to therapy.
Ga-67 uptake may also occur in infections and granulomatous diseases.
Because of gut activity, thallium imaging is not useful for the evaluation of abdominal or pelvic disease.
Inaccurate staging of lymphomas and a false-positive diagnosis may occur as a result of FDG uptake in association with nonspecific inflammatory lymph nodes. Lack of increased metabolic activity within enlarged nodes has been shown to correlate well with lack of tumor involvement. However, nodes and lesions smaller than 1 cm may lack sufficient metabolic activity and potentially can cause a false-negative result. The same size criteria also apply to cross-sectional imaging of nodes smaller than 1 cm, which can again lead to false-negative findings.
Persistent FDG uptake within a residual mass should prompt strong consideration of additional therapy, although occasionally the uptake may be related to thymic hyperplasia or a histiocytic reaction.
Several sites demonstrate normal physiologic activity on FDG-PET scans, and these may contribute to false findings. FDG-PET scanning can be degraded by physiologic activity that masks lesions, although this appears to be less of a problem with this modality than it is with 67Ga imaging.
Although the normal intense FDG-PET scan brain activity is not relevant to thoracic imaging, it is important overall for staging NHL. This activity may obscure a brain lesion, but it is not a severe limitation in FDG-PET scanning, because standard staging with CT scanning does not usually include the brain. Cardiac uptake may interfere with thoracic FDG-PET scanning, particularly in a postprandial state, when cardiac activity is at its maximum. Therefore, patients should fast to minimize myocardial uptake and maximize thoracic uptake. Urinary excretion of FDG may obscure abnormalities in the abdomen. Faint bowel activity can also be seen on FDG studies, but it is generally not enough to cause confusion with actual disease.
Angiography
Lymphomatous tissue is generally hypervascular, but angiography is seldom used in the diagnosis of NHL. With the widespread availability of multidetector-row CT scanners, CT angiography (CTA) is becoming increasingly feasible .
Radiation therapy to the thorax is a risk factor for coronary artery disease. [34] Patients with radiation-induced atherosclerosis are typically young and often have lesions involving the coronary ostia and the left anterior descending artery. Frequently, the best method of revascularization is coronary bypass. Because patients tend to be young, the use of arterial conduits is considered to be superior to the employment of venous grafts. However, the internal thoracic arteries may be caught in the radiation beam and may contain atheromas; hence, they may be unavailable for coronary artery revascularization. To show these changes, preoperative angiography is an essential prerequisite in these patients. [35, 36]
Angiography has little, if any, role in the diagnosis of NHL. Angiography is invasive but is still regarded as a criterion standard in imaging the heart and major blood vessels. However, angiography is being challenged by magnetic resonance angiography (MRA) and CTA.
Lymphomatous deposits may be hypovascular. In rare cases, false-negative results may also occur in the differentiation of aneurysms associated with laminar intraluminal thrombus from other mediastinal masses. The sensitivity and specificity of angiography in the diagnosis of aortic aneurysms are 85% and 95%, respectively.
Questions & Answers
Overview
What is the prevalence of thoracic involvement in non-Hodgkin lymphoma (NHL)?
What is the classification of low-grade thoracic non-Hodgkin lymphoma (NHL) tumors?
What are the preferred modalities for thoracic non-Hodgkin lymphoma (NHL) imaging?
What is the classification of intermediate-grade thoracic non-Hodgkin lymphoma (NHL) tumors?
What is the classification of high-grade thoracic non-Hodgkin lymphoma (NHL) tumors?
What is the classification of miscellaneous thoracic non-Hodgkin lymphoma (NHL) tumors?
What are the characteristics of follicular thoracic non-Hodgkin lymphoma (NHL) tumors?
How is thoracic non-Hodgkin lymphoma (NHL) staged?
What are limitations of radiography for thoracic non-Hodgkin lymphoma (NHL) imaging?
What are limitations of CT scans for thoracic non-Hodgkin lymphoma (NHL) imaging?
What are limitations of MRI for thoracic non-Hodgkin lymphoma (NHL) imaging?
What are limitations of ultrasonography for thoracic non-Hodgkin lymphoma (NHL) imaging?
What are limitations of nuclear imaging for thoracic non-Hodgkin lymphoma (NHL)?
What is the role of image-guided biopsy in the diagnosis of thoracic non-Hodgkin lymphoma (NHL)?
Which radiography findings are characteristic of thoracic non-Hodgkin lymphoma (NHL)?
Which types of non-Hodgkin lymphomas (NHL) have a predilection for the mediastinum?
Which radiographic findings are characteristic of pleural involvement of non-Hodgkin lymphoma (NHL)?
Which radiographic findings are characteristic of thoracic wall non-Hodgkin lymphoma (NHL)?
Which radiographic findings are characteristic of recurrent thoracic non-Hodgkin lymphoma (NHL)?
What is the role of radiography in thoracic non-Hodgkin lymphoma (NHL) imaging?
What is the accuracy of radiography for the diagnosis of thoracic non-Hodgkin lymphoma (NHL)?
What is the role of CT in thoracic non-Hodgkin lymphoma (NHL) imaging?
What is the CTA sign in thoracic non-Hodgkin lymphoma (NHL) imaging?
What are the advantages of CT for thoracic non-Hodgkin lymphoma (NHL) imaging?
What is the accuracy of CT in thoracic non-Hodgkin lymphoma (NHL) imaging?
What is the role of MRI in thoracic non-Hodgkin lymphoma (NHL) imaging?
What are the advantages of MRI in thoracic non-Hodgkin lymphoma (NHL) imaging?
What are the disadvantages of MRI in thoracic non-Hodgkin lymphoma (NHL) imaging?
What is the role of ultrasonography in thoracic non-Hodgkin lymphoma (NHL) imaging?
What are the advantages of ultrasonography for thoracic non-Hodgkin lymphoma (NHL) imaging?
What are the disadvantages of ultrasonography for thoracic non-Hodgkin lymphoma (NHL) imaging?
What is the role of nuclear imaging in the workup of thoracic non-Hodgkin lymphoma (NHL)?
What is the role of thallium-201 (201Tl) scans in thoracic non-Hodgkin lymphoma (NHL) imaging?
What is the role of gallium-67 scans in thoracic non-Hodgkin lymphoma (NHL) imaging?
What is the role of FDG-PET scans for thoracic non-Hodgkin lymphoma (NHL) imaging?
What is the role of FDG-PET scans in thoracic non-Hodgkin lymphoma (NHL) imaging?
What is the accuracy of Ga-67 scintigraphy for thoracic non-Hodgkin lymphoma (NHL) imaging?
What is the accuracy of Tl-201 scans for thoracic non-Hodgkin lymphoma (NHL) imaging?
What are the advantages of FDG-PET scanning for thoracic non-Hodgkin lymphoma (NHL) imaging?
What causes false positives and negatives in nuclear imaging of thoracic non-Hodgkin lymphoma (NHL)?
What is the role of angiography in thoracic non-Hodgkin lymphoma (NHL) imaging?
-
Posteroanterior (PA) chest radiograph in a man with thoracic non-Hodgkin lymphoma (NHL) shows mediastinal widening due to grossly enlarged right paratracheal and left paratracheal nodes.
-
Posteroanterior (PA) chest radiograph in a 16-year-old male adolescent with thoracic non-Hodgkin lymphoma (NHL) shows subtle enlargement of the lower paratracheal lymph nodes.
-
Nonenhanced CT scan through the mediastinum shows multiple enlarged lymph nodes in the prevascular space, in the right and left paratracheal region. Nodes in the left paratracheal region cause the trachea to be indented and narrowed on the left side. Note the small, bilateral pleural effusion.
-
Nonenhanced CT scan through the mediastinum at the level of the carina shows enlarged tracheobronchial and subcarinal nodes. Note the small bilateral pleural effusion.
-
Image shows gross enlargement of subcarinal lymph nodes, which causes the tracheal bifurcation to become splayed, and large hilar nodes. Small bilateral pleural effusions are present.
-
Contrast-enhanced axial CT scan in a child shows hypoattenuating, enlarged, subcarinal lymph nodes with splaying of the tracheal bifurcation.
-
Posteroanterior (PA) chest radiograph shows a large mass in the right parahilar region extending into the right upper and middle zones, with silhouetting of the right pulmonary artery. Smaller mass is seen in the periphery of the right lower zone. The masses did not respond to a trial of antibiotics. Core-needle biopsy of the larger lesion revealed NHL deposits in the lung.
-
Lateral image shows a large mass in the anterior aspect of the right upper lobe of the lung.
-
Image shows a normal mediastinum and lungs, destruction of the posterior aspect of the right seventh rib, and soft tissue swelling.
-
Radiograph of a patient with non-Hodgkin lymphoma (NHL) of the ribs shows destruction of the rib and soft-tissue mass.
-
Tomogram of the right lower chest wall demonstrates the lesion better than previous image in this patient with non-Hodgkin lymphoma (NHL) of the ribs.
-
Anteroposterior (AP) view shows a collapsed vertebra in a patient with non-Hodgkin lymphoma (NHL) of the thoracic vertebrae.
-
Lateral myelogram shows abrupt tapering of thecal sac caused by compression of soft tissue associated with the lymphomatous deposit in the thoracic vertebrae.
-
Posterior bone scan shows no abnormally increased uptake in the thoracic vertebrae. Image shows an unusual pattern of non-Hodgkin lymphoma (NHL) of the upper thoracic vertebra.
-
Image shows a right-sided, hemorrhagic pleural effusion. Cytologic and pleural biopsy results confirmed non-Hodgkin lymphoma (NHL).
-
Nonenhanced axial CT scan shows biopsy-proved non-Hodgkin lymphoma (NHL) of the thymus, which appears as a hypoattenuating mass in the anterior mediastinum. Note the tracheal displacement to the right.
-
This 28-year-old man was being evaluated for fever of unknown origin. Gallium-67 study shows extensive uptake in the mediastinal lymph nodes due to non-Hodgkin lymphoma (NHL).
-
T1-weighted coronal MRIs of the thorax in a 55-year-old woman with lower dorsal pain. Note the signal-intensity changes in the body of D12; these are associated with a right-sided, large, paravertebral soft-tissue mass involving the psoas muscle. Biopsy confirmed non-Hodgkin lymphoma (NHL).
-
T1-weighted coronal MRIs of the thorax in a 55-year-old woman with lower dorsal pain (same patient as in the previous image). Note the signal-intensity changes in the body of D12; these are associated with a right-sided, large, paravertebral soft-tissue mass involving the psoas muscle. Biopsy confirmed non-Hodgkin lymphoma (NHL).
-
Positron emission tomography (PET) CT in an 80-year-old woman with diffuse, large B-cell NHL of the skin and subcutaneous tissues that recently transformed from prior low-grade non-Hodgkin lymphoma (NHL). CT scan of the lower neck shows several subcutaneous nodules of varying size with variable uptake on PET (arrows).
-
Positron emission tomography (PET) CT in an 80-year-old woman with diffuse, large B-cell NHL of the skin and subcutaneous tissues that recently transformed from previous low-grade non-Hodgkin lymphoma (NHL) in the same patient as in the previous image. PET shows high level of uptake in the anterior subcutaneous nodule in the chest (white arrows). CT scan of similar nodules (arrowheads) on the anterior left chest does not show PET uptake; these may represent regions of lower-grade NHL. PET image of posterior lesions shows only mild uptake (gray arrow).
-
Contrast enhanced axial CT showing extensive right hilar and posterior mediastinal lymphadenopathy due to thoracic NHL.
-
Gallium-67 (67Ga) scan shows the intrathoracic lymphoma to be 67Ga avid.
-
A PA chest radiograph in a 28-year-old woman who presented with weight loss, showing a cavitating lesion (mimicking tuberculosis) in the left midzone adjacent to the left hilum. Histology confirmed a large-cell NHL.
-
An axial CT scan showing an intraparenchymal cavitating lung lesion adjacent to the anterior thoracic wall.
-
Axial CT scans showing superior vena caval obstruction secondary to lymphadenopathy from NHL.
-
Axial CT scans showing superior vena caval obstruction secondary to lymphadenopathy from NHL.