Practice Essentials
Juvenile idiopathic arthritis (JIA), or juvenile rheumatoid arthritis, is the most common chronic arthritis in children. It is one of the most common chronic illnesses of childhood and a major cause of short-term and long-term functional disability and eye disease leading to blindness. Although it has been customary to refer to JIA as one disease, it is almost certainly 3 or more diseases, which may have the same cause, different causes, or a closely related series of host responses. The course of JIA is unpredictable; it tends to be most predictable after the pattern of the disease is established. JIA affects one or more joints before the age of 16 years, persists for more than 6 weeks, and is of unknown etiology and pathophysiology. The most commonly involved and clinically important joints in JIA are the temporomandibular joints, spine, sacroiliac joints, wrists, hips, and knees. [1, 2, 3, 4, 5, 6, 7, 8]
Uveitis is the most common extra-articular manifestation of JIA and can be chronic or acute. Chronic anterior uveitis occurs in 10-20% of children; it is usually asymptomatic, and external evidence is rare. [4]
The following 7 categories of JIA have been devised by the International League of Associations for Rheumatology (ILAR), classified on the basis of clinical and biochemical markers that aid detection and treatment, as well as research [7] :
-
Enthesitis-related arthritis (ERA)
-
Extended oligoarticular JIA (eoJIA), which involves ≤4 joints
-
Juvenile psoriatic arthritis (jPsA)
-
Rheumatoid factor (RF)-positive polyarticular JIA (RF+ pJIA)
-
RF-negative polyarticular JIA (RF- pJIA)
-
Systemic-onset JIA (sJIA)
-
Undifferentiated JIA, which generally involves ≥4 joints
Imaging plays an important role in supporting the clinical diagnosis of JIA by narrowing the differential diagnoses and establishing a baseline for monitoring disease progression. The mainstay of initial imaging remains conventional radiography, which is readily accessible and provides needed information on growth disturbances and damage to cartilage and bone. Indirect radiographic signs include soft-tissue swelling, increased density of soft tissue, and dislocation of fat folds. Other features include periarticular osteoporosis, joint space narrowing, bone erosion and deformity, and joint subluxation or ankyloses. [9]
MRI is the preferred imaging modality for the assessment of inflammatory and destructive changes in JIA. All affected joints can be easily examined, with excellent contrast resolution of both bone and soft tissues. It is the most sensitive imaging technique for detecting synovitis. The MR imaging protocol should include T1 spin-echo sequence, fat-suppressed sequence (classic T2 fat-sat; short tau inversion recovery-STIR; DIXON fat-suppression sequence); and T1 fat-suppressed sequence precontrast and postcontrast. [10, 11, 12, 3]
Ultrasonography (US) may be helpful to define affected anatomic compartments. Dynamic, Doppler, and/or multifocal US assessments can be used to monitor therapy response and guide interventions. Ultrasound allows easy access and nonirradiating examination for JIA. US evaluation of synovial thickening and synovitis is particularly important. They appear as abnormally hypoechoic tissue associated with joint lines or surrounding tendons. US also provides an accurate guide for intra-articular corticosteroid injections. [9, 13, 12, 3, 14, 15, 16]
In some studies, ultrasonography has been reported as possibly being more sensitive than plain radiography in the detection of cartilage erosions and effusions, but ultrasonography is notoriously operator dependent. On sonograms, inflamed synovium can appear as an area of mixed echogenicity lining the articular cartilage. Serial measurements of synovial thickness and effusion volumes have been used to monitor disease progression. The vascularity of the synovium can be assessed with Doppler flow studies. Ultrasonography can be helpful for assessment of inflammation and guiding joint injections primarily in peripheral joints. [17, 9, 14]
(See the images of JIA below.)
 Plain radiograph of the knee shows osteopenia with enlargement of the distal femoral epiphysis. Epiphyseal overgrowth is thought to result from chronic hyperemia.
Plain radiograph of the knee shows osteopenia with enlargement of the distal femoral epiphysis. Epiphyseal overgrowth is thought to result from chronic hyperemia.
 Ankylosis in the cervical spine at several levels due to long-standing juvenile idiopathic arthritis (JIA).
Ankylosis in the cervical spine at several levels due to long-standing juvenile idiopathic arthritis (JIA).
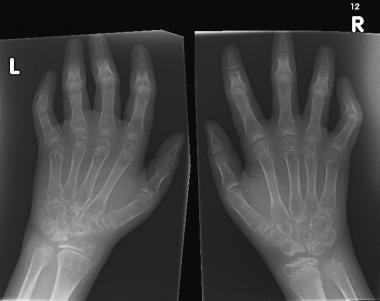 Widespread osteopenia, carpal crowding (due to cartilage loss), and several erosions affecting the carpal bones and metacarpal heads in particular in a child with advanced juvenile idiopathic arthritis (JIA).
Widespread osteopenia, carpal crowding (due to cartilage loss), and several erosions affecting the carpal bones and metacarpal heads in particular in a child with advanced juvenile idiopathic arthritis (JIA).
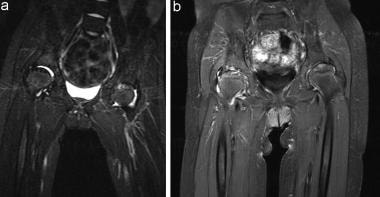 (A) T2-weighted MRI shows high signal in both hips, which may be due to hip effusions or synovitis. High signal intensity in the left femoral head indicates avascular necrosis. (B) Coronal fat-saturated gadolinium-enhanced T1-weighted MRI shows bilateral enhancement in the hips. This indicated bilateral active synovitis, which is most pronounced on the right. Because the image was obtained with fat saturation, the hyperintensity in both hips is pathologic, reflecting an inflamed pannus.
(A) T2-weighted MRI shows high signal in both hips, which may be due to hip effusions or synovitis. High signal intensity in the left femoral head indicates avascular necrosis. (B) Coronal fat-saturated gadolinium-enhanced T1-weighted MRI shows bilateral enhancement in the hips. This indicated bilateral active synovitis, which is most pronounced on the right. Because the image was obtained with fat saturation, the hyperintensity in both hips is pathologic, reflecting an inflamed pannus.
Criteria and classification
The European League against Rheumatism (EULAR) proposed the term juvenile chronic arthritis (JCA) for the heterogeneous group of disorders that manifest as juvenile arthritis. The diagnosis requires that the arthritis begins before the age of 16 years, that it lasts for at least 6 weeks, and that other diseases are excluded. The EULAR criteria for JCA recognize the following subtypes, based on characteristics at onset [18] :
-
Pauciarticular (1-4 joints)
-
Polyarticular (≥5 joints)
-
Presence of RF (2 positive tests at least 3 months apart)
-
Systemic onset with characteristic features
-
Positivity for rheumatoid factor
-
Juvenile ankylosing spondylitis
-
Juvenile psoriatic arthritis
Knee
The knee joint is the most commonly affected joint in JIA and can therefore be considered an index joint for evaluation of disease and for monitoring response to therapy. As in other joints, knee involvement is characterized by a swollen, painful, warm joint with loss of function. In patients with JIA and knee involvement, the main imaging features include synovial thickening, joint effusion, and bone marrow edema. In addition, cartilage loss and bone erosions may be observed. Tendinopathy, enthesopathy, inhomogeneity of the infrapatellar fat pad, and bone cysts may be seen but are relatively uncommon in the knee joint. [10, 11, 17, 19, 12, 20, 21]
Hip
The hip is affected in 20-50% of children with JIA and can result in irreversible destructive damage within 5 years. Imaging findings include inflammation (synovitis, tendinitis, bursitis) and effusions before the occurrence of periarticular bony changes such as bone marrow edema. MRI is the only imaging modality that can identify both soft tissue and bone marrow changes. [12]
Spine
In cases of spine involvement, the cervical spine is the area of the spine that is most frequently involved, with up to 65% of patients having cervical spine symptoms. Contrast-enhanced MRI can detect early, subclinical cervical spine arthritis, with joint effusion, enhancing thickened synovium, and bone marrow edema. MRI can also identify late changes, such as erosions, dens deformation, subluxations, joint ankyloses, and neural compression. [12]
Wrist
The wrist is affected in JIA in about 25% of patients in early disease and increases to 40% after 5 years. Conventional radiography is generally used first identify growth abnormalities and destructive changes. Ultrasonography has also been found to help assess inflammation and guide joint injections. Ultrasound can detect synovitis, tenosynovitis, cartilage damage, and bone erosions in the wrist. MRI, however, is the most effective modality to identify inflammation, synovitis, tenosynovitis, effusion, bone marrow edema, and late destructive changes. [12]
Temporomandibular joint
Contrast-enhanced MRI is commonly used to evaluate TMJ disease in patients with JIA. MRI can detect acute and early inflammatory changes, including joint effusion, synovial enhancement and thickening, and bone marrow edema, along with chronic changes such as erosions, osseous deformity, new bone formation, and disc abnormalities. For evaluation of JIA in the TMJ, MRI examination includes both open-mouth and closed-mouth sequences. To identify disc position and function in relation to the condyle, it is important to compare open-mouth views with closed-mouth views. The closed-mouth view is best for evaluating condyle morphology. [22, 23, 24, 12, 15]
Sacroiliac joint
The sacroiliac joints are affected in about 30% of children with JIA, but these joints are not usually affected in the early stage of JIA; typically, enthesitis and lower extremity peripheral arthritis occur before SI joint involvement. MRI is the preferred imaging modality to detect sacroiliac inflammation. Active features include bone marrow edema, enthesitis, and capsulitis/synovitis. Structural damage includes erosions, fatty deposition, sclerosis, and ankylosis. [12]
Radiography
Plain radiography is the primary method of imaging for the diagnosis and follow-up evaluation of juvenile idiopathic arthritis. [25, 26, 22, 27] Basic radiographic changes include the following:
-
Soft-tissue swelling
-
Osteopenia and/or osteoporosis
-
Joint-space narrowing
-
Bony erosions
-
Intra-articular bony ankylosis
-
Periosteitis
-
Growth disturbances
-
Epiphyseal compression fracture
-
Joint subluxation
-
Synovial cysts
The main limitation of conventional radiography is that it does not allow direct examination of the articular cartilage, synovium, and other important noncalcified structures in a joint.
(See the images below.)
 Plain radiograph of the knee shows osteopenia with enlargement of the distal femoral epiphysis. Epiphyseal overgrowth is thought to result from chronic hyperemia.
Plain radiograph of the knee shows osteopenia with enlargement of the distal femoral epiphysis. Epiphyseal overgrowth is thought to result from chronic hyperemia.
 Ankylosis in the cervical spine at several levels due to long-standing juvenile idiopathic arthritis (JIA).
Ankylosis in the cervical spine at several levels due to long-standing juvenile idiopathic arthritis (JIA).
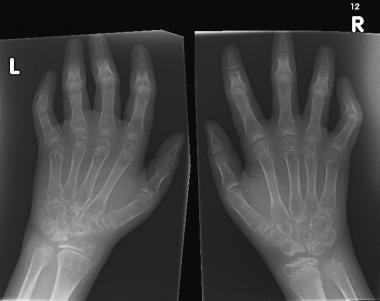 Widespread osteopenia, carpal crowding (due to cartilage loss), and several erosions affecting the carpal bones and metacarpal heads in particular in a child with advanced juvenile idiopathic arthritis (JIA).
Widespread osteopenia, carpal crowding (due to cartilage loss), and several erosions affecting the carpal bones and metacarpal heads in particular in a child with advanced juvenile idiopathic arthritis (JIA).
Magnetic Resonance Imaging
MRI is the imaging modality of choice for JIA and clearly shows the difference between changes in articular cartilage and bone erosions. Bone erosions can be seen on T1-weighted images as loss of normal low signal intensity of cortical bone and loss of the normal high signal intensity of trabecular bone. On T2-weighted images, bone erosions appear as hypointense lesions, whereas subchondral cysts appear as hyperintense signal on fluid-sensitive images. [10, 12, 21]
The MR imaging protocol should include T1 spin-echo sequence, fat-suppressed sequence (classic T2 fat-sat; short tau inversion recovery-STIR; DIXON fat-suppression sequence); and T1 fat-suppressed sequence precontrast and postcontrast. [3, 10, 11, 12]
To improve visualization of synovial hypertrophy and improve detection of cartilaginous erosions when an inflammatory arthritis is suspected, contrast-enhanced sequences should be performed. MRI provides the most sensitive radiologic indicator of disease activity. MRI can depict synovial hypertrophy, define soft tissue swelling, and demonstrate excellent detail of the status of articular cartilage and overall joint integrity. [22, 27, 28, 29, 19, 30, 23, 24, 31, 20]
(See the MRI image below.)
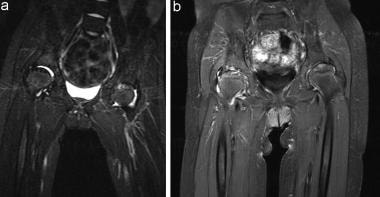 (A) T2-weighted MRI shows high signal in both hips, which may be due to hip effusions or synovitis. High signal intensity in the left femoral head indicates avascular necrosis. (B) Coronal fat-saturated gadolinium-enhanced T1-weighted MRI shows bilateral enhancement in the hips. This indicated bilateral active synovitis, which is most pronounced on the right. Because the image was obtained with fat saturation, the hyperintensity in both hips is pathologic, reflecting an inflamed pannus.
(A) T2-weighted MRI shows high signal in both hips, which may be due to hip effusions or synovitis. High signal intensity in the left femoral head indicates avascular necrosis. (B) Coronal fat-saturated gadolinium-enhanced T1-weighted MRI shows bilateral enhancement in the hips. This indicated bilateral active synovitis, which is most pronounced on the right. Because the image was obtained with fat saturation, the hyperintensity in both hips is pathologic, reflecting an inflamed pannus.
Synovitis and a joint effusion may have similar hyperintensity on T2-weighted (T2W) and short-tau inversion recovery (STIR) images. Therefore, gadolinium-enhanced T1-weighted (T1W) MRIs are necessary to accurately define active synovitis.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). NSF/NFD has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Ultrasonography
In some studies, ultrasonography has been reported as possibly being more sensitive than plain radiography in the detection of cartilage erosions and effusions, but ultrasonography is notoriously operator dependent. On sonograms, inflamed synovium can appear as an area of mixed echogenicity lining the articular cartilage. Serial measurements of synovial thickness and effusion volumes have been used to monitor disease progression. The vascularity of the synovium can be assessed with Doppler flow studies. [9, 17, 14]
In pediatric rheumatology, ultrasonography plays an important role in narrowing the differential diagnosis and can be useful for treatment monitoring and guiding joint injections. Because it has a relatively low cost and is widely available, it can be used to assess multiple joints. Limitations include the inability to examine bone marrow or reliably detect central erosive changes because of the low penetration of the ultrasound beam. [10]
Power and color Doppler imaging have proven useful for acquiring information about tissue perfusion and differentiating active (hypervascular) from fibrotic (hypovascular) pannus. [10]
-
Plain radiograph of the knee shows osteopenia with enlargement of the distal femoral epiphysis. Epiphyseal overgrowth is thought to result from chronic hyperemia.
-
Ankylosis in the cervical spine at several levels due to long-standing juvenile idiopathic arthritis (JIA).
-
Widespread osteopenia, carpal crowding (due to cartilage loss), and several erosions affecting the carpal bones and metacarpal heads in particular in a child with advanced juvenile idiopathic arthritis (JIA).
-
(A) T2-weighted MRI shows high signal in both hips, which may be due to hip effusions or synovitis. High signal intensity in the left femoral head indicates avascular necrosis. (B) Coronal fat-saturated gadolinium-enhanced T1-weighted MRI shows bilateral enhancement in the hips. This indicated bilateral active synovitis, which is most pronounced on the right. Because the image was obtained with fat saturation, the hyperintensity in both hips is pathologic, reflecting an inflamed pannus.




