Practice Essentials
Hodgkin disease (lymphoma) is a cancer of the lymph system that is characterized by the presence of large, abnormal Reed-Sternberg cells in a background of lymphocytes, macrophages, fibroblasts, and granulocytes. Dr Thomas Hodgkin first described Hodgkin disease in 1832. [1, 2, 3, 4] The lymphatic system is composed of lymph nodes, lymphatic channels, the spleen, bone marrow, and the thymus. Because the lymphatic system is located throughout the body, Hodgkin disease can start almost anywhere; however, in this article, only thoracic involvement is addressed. [5]
Classical Hodgkin lymphoma (HL) accounts for approximately 95% of all HL cases, with the other 5% being nodular lymphocyte-predominant HL (NLP-HL). Classical lymphoma is further divided into nodular sclerosis, lymphocyte-rich, mixed cellularity, and lymphocyte-depleted. [6, 7]
Hodgkin lymphoma has an incidence of about 3 new cases per 100,000 individuals per year, making it one of the most common lymphomas. It responds very well to therapy, with cure rates of approximately 80-90% with chemoradiotherapy. [8, 9, 6, 7]
Imaging modalities
CT, MRI, PET/CT, and PET/MRI play a major role in the diagnosis, staging, and response to therapy of Hodgkin lymphoma. Cross-sectional imaging has replaced staging laparotomy and splenectomy. FDG/PET and MRI can identify involvement of bone marrow, and imaging can confirm poor prognostic indicators such as large mediastinal adenopathy, stage IV disease, systemic symptoms, and pleural effusion and pericardial effusion. [10]
CT scanning of the thorax, abdomen, and pelvis is performed for initial staging purposes. Compared with other methods, CT is more sensitive for detecting lymphadenopathy and extralymphatic involvement. CT scanning may be most useful for evaluating patients with lymphoma, because it can depict the lymph nodes in the chest, abdomen, and pelvis. [11, 12, 13, 14] CT scans cannot be used to differentiate the various causes of lymph node enlargement or to determine whether tumor residue is active or inactive. [15]
Magnetic resonance imaging (MRI) is performed in patients with suggested chest wall involvement because it offers better tissue contrast. [16] MRI is still limited in its availability because of its high cost. Also, some patients are claustrophobic and cannot tolerate the MRI examination.
Ultrasonography and echocardiography are useful for detecting pericardial effusion and for directing lymph node biopsies and pleural interventions, [17] but ultrasonography is limited in the thorax because air contained in the lungs is not a suitable window through which the ultrasonographic waves can travel.
Bone scanning is useful for evaluating bone involvement in Hodgkin disease. Gallium-67 (67Ga) scans obtained at baseline, during therapy, and in the posttreatment period can help differente active Hodgkin disease from nonactive Hodgkin disease. [18]
Positron emission tomography (PET) scanning with fluorodeoxyglucose (FDG) is most useful for detecting disease relapse. [19, 20, 21, 22, 23] If available, PET-CT is most often preferred. Currently, PET-CT is widely accepted in developed countries, but this imaging modality has limited availability in developing countries, and the studies are expensive. [11]
Bilateral bone marrow aspirations and biopsies are performed to assess stage III or IV disease with associated symptoms (eg, fever, weight loss >10%, drenching night sweats). [24]
Other investigations are directed to a particular clinical problem. For example, a superior venacavogram is obtained if the patient has clinical findings of superior vena cava (SVC) syndrome. Immunoscintigraphy is used only on an experimental basis.
Radiography is available everywhere and is inexpensive; however, it is limited in the evaluation of soft-tissue involvement of the chest wall. Chest radiographs cannot be used to differentiate the various causes of lymph node enlargement. Posteroanterior (PA) and lateral chest radiographs are essential for clinical staging. Mediastinal adenopathy is the most common presentation, and direct extension of the disease can be detected on chest radiographs. Chest images also allow for the evaluation of complications related to chemotherapy and radiation therapy. In follow-up studies for recurrent disease, chest radiography is the primary imaging modality (along with history taking, physical examination, and laboratory investigations). [25, 26]
(Radiologic characteristics of Hodgkin disease are shown in the images below.)
 A positron emission tomography (PET) scan obtained with fluorodeoxyglucose (FDG) that shows increased FDG uptake in a mediastinal lymph node.
A positron emission tomography (PET) scan obtained with fluorodeoxyglucose (FDG) that shows increased FDG uptake in a mediastinal lymph node.
In the thorax, Hodgkin lymphoma most commonly involves the mediastinum. The nodular sclerosing histologic subtype of Hodgkin disease is the most common form found in the thorax, and it has a predilection for the anterior mediastinum (especially the thymus). The diagnosis of Hodgkin disease must be based on tissue biopsy results, because treatment strategies are based on the histologic type, the stage of disease, and the age, as well as performance status of the patient. Imaging is essential for tumor staging, for assessing the response to treatment, for diagnosing relapses, and for evaluating treatment-related disorders. [2, 27, 28, 29, 30, 31, 25]
Staging
Staging of Hodgkin lymphoma is important for planning effective treatment, for follow-up monitoring, and for comparing trial treatment plans available in various centers.
According to the World Health Organization (WHO)/Revised European-American Lymphoma (REAL) classification, classic Hodgkin lymphoma (HL) is grouped into the following 4 types [32] :
-
Nodular sclerosis classic HL
-
Lymphocyte-rich classic HL
-
Mixed cellularity classic HL
-
Lymphocyte-depleted classic HL
Staging according to the Cotswolds classification is as follows [33] :
-
Stage I - Involvement of a single lymph node region (I) or localized involvement of a single extralymphatic organ (IE)
-
Stage II - Involvement of 2 or more lymph node regions on the same side of the diaphragm (II) or localized involvement of a single extralymphatic organ or site and its regional lymph node or nodes, with or without involvement of the other lymph node region on the same side of the diaphragm (IIE)
-
Stage III - Involvement of lymph node regions on both sides of the diaphragm (III) with or without localized involvement of an associated extralymphatic organ or site (IIIE), with or without involvement of the spleen (IIIS), or with or without involvement of both (IIIE+S)
-
Stage IV - Disseminated/multifocal involvement of 1 or more extralymphatic organs, with or without associated lymph node involvement, or isolated extralymphatic organ involvement with distal nodal involvement
Bulk disease, or massive mediastinal disease, is defined as the ratio of the maximum transverse diameter of a mass to the internal transverse thoracic diameter being 0.33 or greater, as measured on chest radiographs at the T5-T6 vertebral disk level. Other authors have defined bulk disease as a lymph node mass measuring 10 cm or more in its greatest dimension. [34]
The presence of other symptoms (eg, fever, weight loss >10%, drenching night sweats) and bulk disease is associated with a worse prognosis for patients with clinical stage I or stage II Hodgkin lymphoma.
Radiography
Hodgkin disease commonly appears as intrathoracic disease. Posteroanterior (PA) and lateral chest radiographs are essential for clinical staging. Mediastinal adenopathy is the most common presentation, and direct extension of the disease can be detected on chest radiographs. Chest images also allow for the evaluation of complications related to chemotherapy and radiation therapy. In follow-up studies for recurrent disease, chest radiography is the primary imaging modality (along with history taking, physical examination, and laboratory investigations). [25]
Among patients with Hodgkin disease, 67-74% have abnormal radiographic findings at presentation. Among patients with abnormal radiographic findings on chest images, 90% have bilateral, asymmetrical nodal disease.
In Hodgkin lymphoma, disease spreads contiguously along lymph node chains. Prevascular and paratracheal lymph nodes are most commonly affected. A single lymph node group is involved in only 15% of patients. Rarely, the posterior mediastinal or paracardiac lymph nodes are involved.
The internal mammary chain of lymph nodes can be enlarged, but not without involvement of other lymph nodes.
Chest radiographs can demonstrate either a single group with lymph node enlargement or a lobulated appearance resulting from multinodal involvement.
Calcification is very rarely seen in untreated lymphoma. [35]
Direct invasion of the lungs can occur in 15-40% of patients and is nearly always associated with hilar adenopathy. [36] Primary pulmonary involvement without hilar, mediastinal, or extrathoracic involvement is unusual; however, recurrent Hodgkin disease may appear in the absence of adenopathy (especially in nodular sclerosing Hodgkin disease).
Lung involvement can produce either ill-defined or well-defined nodules, which can be unilateral or bilateral. These nodules may cavitate. Lung involvement can also appear as consolidation.
Other findings in Hodgkin lymphoma that can be detected on radiographs of the chest include pleural effusions and skeletal lesions. [18]
In Hodgkin disease, two thirds of bone lesions are of the mixed lytic and sclerotic variety, 10-15% are sclerotic alone, and a small percentage are lytic alone. Sclerotic lesions tend to be confined to the vertebrae, demonstrating the typical appearance of ivory vertebrae.
Anterior scalloping of vertebrae can be detected on lateral chest radiographs, especially in the lower thoracic region.
With chest radiographs, Hodgkin disease can be quantified by calculating the mediastinal mass ratio (the ratio of the maximum width of the mediastinum to the maximum transverse thoracic diameter at the level of the diaphragm), by finding a mediastinal mass larger than one third of the transverse thoracic diameter at the T4-T5 level, or by determining an absolute transverse mediastinal diameter of 10 cm. [37]
In follow-up imaging of mediastinal bulk disease, 60% of chest radiographs demonstrate findings of residual adenopathy after treatment. This residual adenopathy may not contain active disease and may represent only residual scarring, but these can be seen at long-term follow-up.
Knowledge of lymph node distribution and lymphatics in the thorax is important because mediastinal involvement of the lymph nodes is the most common manifestation of thoracic Hodgkin disease. A clear understanding of normal radiographic findings in chest radiography is pivotal to recognizing subtle enlargement of the lymph nodes. [2, 25]
On chest radiographs on the left side, the normal aortopulmonary window is slightly concave, straight, or invisible. Any departure should be viewed with suspicion, and further investigations are needed. In the prevascular area, adenopathy is the most common cause for convexity of the aortopulmonary bay toward the left lung.
On chest radiographs on the right side, the azygos node lies variably in relation to the azygos vein as the vein passes forward above the right bronchus to enter the superior vena cava (SVC). This node is the lowest member of the group of right paratracheal lymph nodes. Any convexity in this region that has a greater part of its curvature above the right main bronchus probably should be regarded as abnormal. Low right prevascular nodal enlargement also can distort this region.
Subcarinal lymph nodes are difficult to recognize until they are large. They can cause displacement of the azygoesophageal pleural reflection. Paravertebral adenopathy can be diagnosed by distortion of the paravertebral pleural reflections, which produces convexity toward the lungs.
Pericardiac and diaphragmatic lymph nodes can fill the cardiophrenic angle on posteroanterior (PA) chest radiographs. On lateral views, these may lie retrosternally or at the level of the inferior vena cava or phrenic nerve. Smaller lymph nodes in these areas may simulate a pericardiac fat pad.
On PA chest radiographs, internal mammary lymph nodes can produce ill-defined increased opacity lateral to the sternum when sufficiently enlarged. On lateral views, these can appear as anterior extrapleural masses against the chest wall.
Degree of confidence
Most of the time, sufficiently enlarged lymph nodes in the thorax can be detected on chest radiographs, but subtle enlargement can be missed; therefore, further imaging with CT scanning is warranted.
A confluence of pulmonary veins, especially on the right side, can be mistaken for subcarinal lymphadenopathy. Small pericardiac or diaphragmatic lymph nodes can mimic a fat pad. An enlarged azygos vein can mimic azygous adenopathy. When in doubt, repeat chest radiographs and use the Valsalva maneuver. All of these false-positive findings on chest radiography can be easily identified by performing CT.
Subtle enlargement of intrathoracic lymph nodes can be missed on chest radiographs, and its detection greatly depends on the observer's experience, as well as the type of radiograph performed.
Computed Tomography
In conjunction with chest radiographs, CT scanning is useful for initial staging and follow-up monitoring of Hodgkin disease. Contrast-enhanced CT scanning of the thorax, abdomen, and pelvis is performed in all patients. Any suggestion of lymph node enlargement, as demonstrated on chest radiographs, is usually confirmed with CT scanning. [13, 38, 39, 11]
CT scanning has the additional advantage of depicting other areas of lymph node enlargement that are not obvious on chest radiographs. Some areas of lymph node enlargement that are difficult to detect by using radiography include paracardiac, supradiaphragmatic, and internal mammary chain lymph nodes; these can be detected easily via CT scanning. The modality also helps in formulating treatment plans and radiation fields. [4, 12, 13, 38]
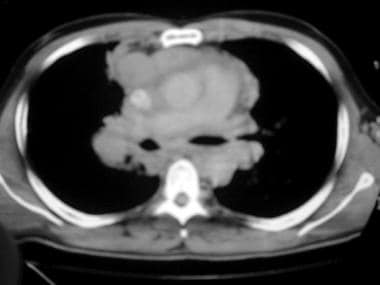
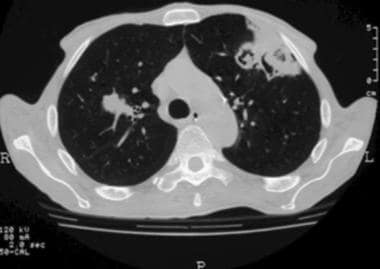
(CT scans depicting characteristics of Hodgkin disease are presented below.)
Involvement of the lungs and pericardium can occasionally be detected on CT scans; these exclude treatment by radiation therapy.
CT size criteria for lymph node involvement in the mediastinum are well defined. According to the criteria, subcarinal, paracardiac, and retrocrural lymph nodes are considered enlarged if they are larger than 12, 8, and 6 mm in their short-axis diameter, respectively. The remaining lymph nodes in the body are considered enlarged if they are larger than 10 cm in their short-axis diameter. [37, 40, 41, 42]
On CT scans, lymph node enlargement can be seen as multiple, rounded soft-tissue masses or bulky soft-tissue masses caused by nodal aggregation. Usually, a homogeneous soft-tissue mass is noted; it may be heterogeneous when it is large, with areas of low attenuation representing necrosis, hemorrhage, or cyst formation. [43]
In rare cases, calcification can be seen in the lymph nodes on pretreatment scans.
A discrete or infiltrating thymic mass can be seen.
Associated findings that can be detected on CT scans include mediastinal displacement, compression, and invasion of the vascular structures, pericardium, heart, pleura, lungs, and chest wall. [26]
CT scanning is used during surveillance to detect local and distant recurrences of the disease. Recurrent lymphoma has an appearance similar to that of primary Hodgkin lymphoma; however, pulmonary parenchymal involvement is much more common in recurrent Hodgkin lymphoma. Parenchymal involvement may present as a pulmonary nodule or a mass, lobar or segmental consolidation with air bronchogram, and a reticular pattern with peribronchovascular and interlobular septal thickening. [44]
Recurrence within the radiation field usually presents as an alteration in the contour of the radiation fibrosis, with increase in size, convex borders, obliteration of the air bronchograms with homogeneous opacity, and filling of the bronchi. [45]
Posttreatment radiation fibrosis usually develops 6-12 months after completion of radiation. The features include a well-demarcated area of volume loss, linear scarring or consolidation, parenchymal distortion and traction bronchiectasis, ipsilateral mediastinal shift, and adjacent pleural thickening. [45, 46]
Bleomycin-induced lung toxicity can present as diffuse alveolar damage, nonspecific interstitial pneumonitis, and bronchiolitis obliterans organizing pneumonia. Cyclophosphamide can cause pulmonary hemorrhage and diffuse alveolar damage. Nonspecific interstitial pneumonitis may present as ground-glass opacities combined with reticular opacities in peripheral subpleural distribution.
Bronchiolitis obliterans organizing pneumonia usually presents as bilateral, asymmetric ground-glass opacities or air-space consolidations in the peripheral or peribronchial distribution. [47, 48]
Patients who have been treated for Hodgkin lymphoma have an increased risk of lung cancer and mesothelioma, and CT is the primary imaging modality for both of these.
Degree of confidence
CT scans can help in the differentiation of the various causes of mediastinal or hilar enlargement seen on chest radiographs in most patients; however, CT is limited in detecting chest wall invasion (in which case, MRI is the modality of choice). CT is limited in the use of size criteria for lymph node involvement, because nodes that are larger than those defined by the criteria can be reactive without tumor involvement. Also, lymph nodes smaller than those defined by the size criteria can harbor Hodgkin disease. Residual masses can persist during and after treatment without any viable tumor being present. [38, 12]
CT scans cannot help differentiate between fibrosis and viable tumor. MRI, gallium scanning, or PET scanning can be used to identify residual tumor and predict the patient’s response to therapy. [49, 50, 51, 52, 53]
Magnetic Resonance Imaging
MRI is not the primary modality for evaluating Hodgkin disease, but its use is important in the pediatric population to avoid radiation exposure. Multiplanar capability, high tissue contrast, flow sensitivity, and the use of gadolinium-based contrast agents all make MRI an ideal tool for problem solving. Its soft-tissue contrast and multiplanar capability also make it useful for assessing chest wall invasion, pericardial involvement, pleural involvement, and brachial plexus involvement. [4]
In thoracic lymphomas, MRI is used to image suggestive spinal cord compression, involvement of the spinal cord and the meninges, involvement of the musculoskeletal system in the chest, cardiac involvement, and involvement of the brachial plexus.
MRI is also helpful in posttreatment evaluation to differentiate between fibrosis and tumor. [15]
On MRI, lymph node involvement is defined by size criteria similar to those of CT.
MRI is helpful for planning radiation therapy fields because of its multiplanar capabilities. [49]
On T1-weighted images, tumor involvement can be seen as relatively homogeneous masses with low signal intensity (similar to that of muscle).
On T2-weighted images, high signal intensity equal to or slightly greater than that of fat can result from tumor edema, inflammation, immature fibrosis, or granulomatous tissue. Follow-up T2-weighted images can show signal intensity increased from the baseline. This finding is correlated with disease recurrence.
Low signal intensity on posttherapeutic T2-weighted images rules out the possibility of relapse in most patients. Increased signal intensity on T2-weighted images obtained within 6 months of therapy is nonspecific; however, after 6 months, this finding suggests recurrent disease. [53]
An enlarging or new mass may represent recurrent disease, a posttherapeutic thymic cyst, or thymic hyperplasia. [27]
Overall, the accuracy of MRI for predicting disease recurrence is similar to that of gallium scintigraphy. [51]
Dense fibrosis may demonstrate low signal intensity on T2-weighted images.
MRI has a role in identifying areas of bone marrow abnormality for targeting bone marrow biopsies; however, MRI is not a replacement for bone marrow biopsy in pathologic staging. [54]
Diffusion weighted imaging (DWI) depicts differences in the mobility of water in the tissues. This technique has emerged as a radiation-free alternative to PET-CT for staging of lymphoma and other malignancies. [55] Hypercellular tumors show comparatively restricted water diffusion to normal tissues, which is reflected as high signal intensity on DWI with low apparent diffusion coefficient (ADC). DWI has a sensitivity of up to 97% and can be used as an alternative to PET-CT for follow-up and assessment of treatment response. [56, 57] The higher the magnetic field strength in DWI, the higher the signal-to-noise ratio.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Degree of confidence
As with the criteria used in CT, a lymph node larger than 1.0 cm can be reactive without tumor involvement. Lymph nodes smaller than those that fall within the size criteria can also harbor disease. [37]
MRI is more sensitive for detecting bone marrow involvement associated with lymphoma. [54]
False-positive findings can result from residual lymph node masses that may not harbor any disease. To evaluate this possibility further, gallium scanning and PET scanning can help.
Radiation-induced inflammatory changes can result in increased signal intensity on T2-weighted images. These changes can mimic active disease.
Ultrasonography
Ultrasonography can help in performing mediastinal biopsies, but it is primarily used for the evaluation and biopsy of lesions involving the chest wall. Echocardiography is useful for the detection of clinically undetectable pericardial disease. [4, 17, 58, 59, 60]
Ultrasonography cannot help in differentiating the causes of pericardial effusion (eg, malignant, radiation-induced, drug-induced, or idiopathic effusion).
An echocardiogram can be used for determination of left ventricular ejection fraction before and after chemotherapy.
Nuclear Imaging
Gallium-67 citrate scintigraphy (gallium scanning)
Gallium-67 citrate scintigraphy (GS) has been shown to provide important diagnostic and prognostic information in patients with lymphoma. In Hodgkin disease, GS provides additional information in conjunction with CT for planning radiation therapy. GS is helpful for distinguishing residual disease from posttreatment fibrosis in bulky mediastinal Hodgkin disease. [51, 61, 62, 63]
Posttreatment 67Ga uptake is a poor prognostic factor in Hodgkin lymphoma and non–Hodgkin lymphoma, and it is an accurate predictor of the patient’s response to therapy and the overall outcome. In patients with aggressive lesions, advanced- stage tumors, or difficult-to-treat cases, sequential gallium scintigraphy can be performed before, during, or after therapy. These studies help in understanding the gallium avidity of the tumor, the response of tumor to therapy, and the timing of the therapeutic response. [51, 52, 61, 62, 63, 64]
Gallium uptake in tumor cells is mediated by transferrin receptors, and binding to cell-surface transferrin receptors allows this complex to be taken by actively growing tumor cells. Radiation therapy results in transient or permanent loss of 67Ga uptake, although recurrent Hodgkin disease is invariably associated with the return of increased uptake. [62, 63, 64, 65]
In Hodgkin disease, the sensitivity of GS is 85-97% and the specificity is 90-100%. Use of high-dose GS and single-photon emission CT (SPECT) techniques has increased the sensitivity of GS, especially for evaluating the mediastinum and abdomen. [64, 66]
FDG PET/CT evaluation
FDG PET/CT is crucial for initial staging and evaluation of treatment response in Hodgkin disease. PET/CT often leads to either upstaging or downstaging in approximately 15-40% of patients with Hodgkin lymphoma and, as a result, a change in management in 5-15% of patients. [67, 68, 11] A negative PET study reliably rules out Hodgkin relapse; however, the positive predictive value of PET is variable and thus cannot reliably diagnose a relapse. A biopsy is therefore necessary. [69, 70] FDG PET/CT is extremely useful in radiation treatment planning by helping better map the radiation fields without increasing radiation volumes. [71] FDG PET/CT has limitations, as FDG uptake can be seen in posttreatment inflammation, infection, brown fat, and normal physiologic metabolic activity, leading to false positive results. False negative results can be seen in low-grade histologic subtypes, as well as in minimal residual disease. [72, 73, 74]
Uptake of FDG is increased in malignant cells, as compared to normal tissues, because of a patient’s altered metabolism during malignancy (in which glycolysis becomes the major metabolic pathway). [20, 22, 23, 50, 52, 75, 76] Several studies have suggested that FDG scintigraphy is as good as CT for staging lymphomas. Moog et al showed that FDG PET is superior to CT in staging nodal lymphoma. [77, 78]
Bangerter et al found that for detecting hilar and mediastinal sites of disease before treatment, the sensitivity of FDG PET is 98% and the specificity is 90%, while the positive predictive value is 92% and the negative predictive value is 97%. [79]
FDG PET studies may cause upstaging of the disease because of bone marrow involvement. These studies can be used to guide targeted MRI scans and bone marrow biopsies. FDG PET can also help in characterizing residual masses after therapy, when morphologic imaging modalities are of limited value. PET can be used in the detection of relapse, and Bangerter et al found a sensitivity of 86% and a specificity of 96% for the detection of recurrent disease in mediastinal and hilar nodes in patients with lymphoma. [79]
A multigated acquisition (MUGA) scan can be used for exact determination of ejection fraction.
In patients treated for Hodgkin lymphoma, bone density loss and an increased risk for osteoporosis can be a concern; PET/CT can help identify risk by assessing bone mineral density. In one study, by Cohen et al, 160 Hounsfield units was used to define abnormal bone mineral density (BMD), and age, baseline BMD, and cumulative steroid dose were found to be associated with a decline in BMD and with increased risk for abnormal BMD after chemotherapy. [80]
Degree of confidence
For GS, a posttreatment FDG PET scan with negative findings has a negative predictive value of 100%, but positive scans have a positive predictive value of only 61%.
Gallium uptake is nonspecific, and uptake can be seen in various tumors, inflammation, and infection; however, in a known setting of Hodgkin disease, any abnormal uptake should be viewed as active disease, residual disease, or recurrence (see the image below).
In a study by Alkhawtani et al, lactate dehydrogenase levels and FDG PET/CT findings (ie, tumor size, necrosis, and FDG uptake) helped differentiate between mediastinal Hodgkin lymphoma and primary mediastinal B cell lymphoma. [81]
-
A positron emission tomography (PET) scan obtained with fluorodeoxyglucose (FDG) that shows increased FDG uptake in a mediastinal lymph node.
-
A schematic diagram showing the location of the mediastinal lymph nodes.
-
A CT scan showing bulk disease.
-
A CT scan showing lung parenchyma involvement with Hodgkin disease.
-
A posteroanterior (PA) chest radiograph demonstrating normal findings.
-
A lateral chest radiograph demonstrating normal findings.
-
PA chest radiograph showing a large anterior mediastinal mass in a 19 year female patient
-
Lateral chest radiograph showing a large anterior mediastinal (Hodgkin) mass in a 19 year female patient
-
Coronal view of CT scan with intravenous contrast of a 19 year female showing mediastinal Hodgkin disease. This is the same patient for which PA and lateral views are illustrated.