Practice Essentials
Thoracic aortic aneurysm (TAA) represents aneurysmal dilatation of the ascending thoracic aorta, the aortic arch, or the descending thoracic aorta, or a combination of these locations. The most common location for TAA is the ascending aorta, followed by the descending aorta. Thoracic aortic aneurysms are less common than aneurysms of the abdominal aorta. Aortic aneurysm is defined as a localized or diffuse dilatation of more than 50% normal diameter of the aorta. TAA is diagnosed when there is at least 50% enlargement of the aortic lumen, or alternatively when the aortic diameter is more than two standard deviations above the mean for the patient’s sex and age. [1] It is the most common disease of the thoracic aorta requiring surgical treatment. Better imaging technology has led to the earlier recognition of acute aortic dissection, allowing the identification of more patients with complex conditions who are candidates for surgery. [2]
In patients with aortic aneurysm, aortic dissection is the most feared catastrophic event. Rupture of a thoracic aortic aneurysm is more frequent than abdominal aortic rupture. Thus, high clinical suspicion is required, and time is of the essence. Imaging techniques, including MRI, TEE, or CT scanning, should be quickly utilized.
Preferred examination
Although aortic dissection may be suspected on the basis of history and physical examination findings, diagnostic imaging is necessary to establish the diagnosis. A clear and efficient imaging strategy is required. The clinical team involved in the diagnosis and treatment of patients with aortic dissection should prospectively agree on a strategy. In developing an approach, consideration should be given to the technology available at the institution and the ease of performing each test, especially after hours.
Transesophageal echocardiography (TEE), CT scanning, and MRI have been reported to be highly sensitive for the diagnosis of aortic dissection. However, the specificity of CT scanning and MRI is significantly better than that of TEE. [3]
Many thoracic aneurysms are readily visible on chest radiographs. Characteristic findings are widening of the mediastinal silhouette, enlargement of the aortic knob, or displacement of the trachea from the midline. [4] Lateral films demonstrate loss of the retrosternal air space, but the aneurysms may be completely obscured by the heart, and the chest radiograph may therefore appear normal. Aortic calcification may outline the borders of the aneurysm in the anterior, posterior, and lateral views in both the chest and abdomen.
The preferred examinations for diagnosis are aortic angiography, CT, CT angiography, MRI, MR angiography, and echocardiography. Aortography was the criterion standard against which other modalities were measured, but with the advent of TEE and CT scanning, this modality is now rarely used; however, aortography is still the preferred modality for the preoperative evaluation of thoracic aortic aneurysms and for precise definition of the anatomy of the aneurysm and great vessels. [5, 6, 7]
CT scanning is a reliable modality for diagnosing aortic dissection; this modality is the diagnostic method of choice in most institutions. CT with contrast has become the most widely used diagnostic tool. Contrast CT scans rapidly and precisely evaluate the thoracic and abdominal aorta to determine the location and extent of the aneurysm and the relation of the aneurysm to major branch vessels and surrounding structures. They can help to accurately determine the size of the aneurysm and assess dissection, mural thrombus, intramural hematoma, free rupture, and contained rupture with hematoma. CT scans usually show dilation of the aorta, an intimal flap, and both the false and true lumina. Rapid scanning after an intravenous bolus injection of contrast material allows the detection of differential filling rates in the true and false lumina. [7]
The diagnosis of aortic dissection by standard transthoracic echocardiography is based on detecting intimal flaps in the aorta. Transthoracic echocardiography (TTE) is restricted in patients with abnormal chest wall configuration, narrow intercostal spaces, and obesity, and these limitations are usually overcome by TEE. A major advantage of multidetector CT over TEE is the ability to look beyond the aorta for alternative diagnoses such as pulmonary embolism. [8]
Because of the proximity of the esophagus to the aorta, higher transducer frequencies with TEE may be used to better delineate the aorta. TEE is highly sensitive but less specific, and it is excellent at detecting pericardial effusion and aortic regurgitation. TEE may be quickly performed at the patient's bedside with the patient under sedation; it does not expose the patient to radiation, nor is the injection of contrast material necessary. However, it may be difficult to evaluate the ascending aorta and the proximal arch with TEE.
TTE is not accurate for diagnosing thoracic aneurysms, and it is particularly limited in its ability to examine the descending thoracic aorta. It may help detect aortic insufficiency and aneurysms of the sinus of Valsalva. TEE is a far more accurate method for assessing the thoracic aorta and has become widely used for detection of aortic dissection. There has been less experience with TEE, however, in the evaluation of nondissecting thoracic aneurysms. TEE images show the aortic valve, ascending aorta, and descending thoracic aorta, but they are limited in the area of the distal ascending aorta, transverse aortic arch, and upper abdominal aorta.
MRI is useful in defining thoracic aortic anatomy and detecting aneurysms. This modality is particularly useful for patients with preexisting aortic disease. MRI is an appealing option in the detection of aortic dissection. Sensitivity and specificity are excellent, but it is time consuming and cumbersome to perform. MRA may prove especially useful in defining the anatomy of aortic branch vessels. [5, 6, 9, 10]
Infrarenal abdominal aortic aneurysms may be visualized by means of ultrasonography, but these images do not help define the extent of thoracoabdominal aortic aneurysms.
The American College of Radiology in their Appropriateness Criteria recommend CTA or MRA for diagnosis of suspected thoracic aortic aneurysm. It is noted that MRA can provide high-resolution images of the surrounding thoracic structures and can help evaluate aortic and periaortic inflammation or infection. CTA has a high sensitivity for thrombus and dissection, and the delayed phase can help diagnose aortic wall thickening and enhancement in the presence of infectious or inflammatory aortitis. [1]
Acute myocardial infarction and pneumothorax are included in the differential diagnosis. Other conditions to be considered are acute coronary syndrome, pulmonary embolism, acute pericarditis, pericardial effusion or tamponade, new aortic regurgitation, penetrating aortic ulcer, aortic intramural hemorrhage, esophageal rupture, and musculoskeletal and/or spinal conditions.
(See the 2 images below showing thoracic aortic aneurysm.)
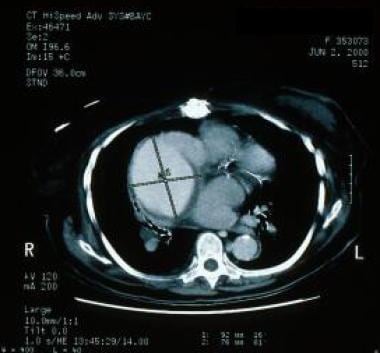
 Computed tomography scan depicting a descending thoracic aortic aneurysm with mural thrombus at the level of the left atrium.
Computed tomography scan depicting a descending thoracic aortic aneurysm with mural thrombus at the level of the left atrium.
Anatomy
Thoracic aneurysms are classified in accordance with the portion of aorta involved: the ascending thoracic aorta, the arch, or the descending thoracic aorta. This anatomic distinction is important because the etiology, natural history, and treatment of thoracic aneurysms vary for each of these segments.
The DeBakey and Stanford classifications are the 2 most widely used methods of describing the types of aortic dissection. In the DeBakey classification, there are 3 types of dissection: types I, II, and III; dissections are classified on the basis of the origin and extent of the dissecting process. In the Stanford system, type A signifies involvement of the ascending aorta, with or without involvement of the arch or the descending aorta (regardless of the site of the primary intimal tear). Type B represents all others, or dissections that do not involve the ascending aorta. [11]
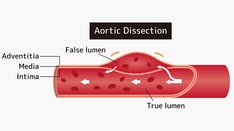
The aortic layers, beginning at the innermost wall, are the intima, the media, and the adventitia. In aortic dissection, a tear in the intima allows blood to escape from the true lumen of the aorta. The inner layer of the media is rapidly dissected from the outer layer, and blood causes the aorta to rapidly expand above normal size. A false channel forms in the outer half of the aortic media, whose walls are exceedingly thin and are highly susceptible to rupture. Size is an important predictor of the risk of aneurysm rupture. [12] Chronic dissections are generally diagnosed 2 weeks after the initial tear and may expand in the weakened aortic wall to develop an aneurysm.
Radiography
Many thoracic aneurysms are readily visible on chest radiographs. Characteristic findings are (1) widening of the mediastinal silhouette, (2) enlargement of the aortic knob, or (3) displacement of the trachea from the midline (see the first image below). [4] Lateral films demonstrate loss of the retrosternal air space, but the aneurysms may be completely obscured by the heart, and the chest radiograph may therefore appear normal. Aortic calcification may outline the borders of the aneurysm in the anterior, posterior, and lateral views in both the chest and abdomen.
Chest radiographs display abnormalities in 80-90% of patients, but the abnormalities are nonspecific. For example, mediastinal widening occurs in more than 75% of cases and may occur in the ascending aorta, the aortic arch, or the descending portion of the thoracic aorta. This finding may be difficult to differentiate from the aortic tortuosity that is associated with long-standing hypertension.
The calcium sign is a rare radiographic finding in aortic dissection (AD). Generally, intimal calcification is seen along the outer border of the aorta. With dissection of the aortic media, the calcium deposit becomes separated from the outermost portion of the aorta by more than 0.5 cm.
Other radiographic signs include a double-opacity appearance of the aorta, with the suggestion of true and false channels; a localized bulge along a normally smooth aortic contour; a disparity in the caliber between the descending and ascending aorta; obliteration of the aortic knob; and displacement of the trachea to the right by the dissection.
With a sensitivity of 64% and specificity of 86% for overt AD, chest radiographs are of limited use apart from the ability to establish or exclude alternative diagnoses. Most importantly, chest radiograpy cannot be relied upon to definitively exclude acute aortic disease. Up to 20% of patients with AD will have a normal or near normal radiographs. [8]
Computed Tomography
On CT scans, thoracic aortic aneurysms are characterized by an increase in aortic diameter and outward displacement of calcium of the aortic wall (see the images below). CT scanning is an effective method for defining the maximum diameter of the aneurysm and monitoring the diameter over time. A diameter exceeding 4 cm is considered aneurysmal. A diameter exceeding 6 cm is usually an indication for surgery of thoracic aortic aneurysm. [7]
 Computed tomography scan depicting a descending thoracic aortic aneurysm with mural thrombus at the level of the left atrium.
Computed tomography scan depicting a descending thoracic aortic aneurysm with mural thrombus at the level of the left atrium.
 Computed tomography scan from a patient whose ascending aortogram showed an ascending aortic aneurysm.
Computed tomography scan from a patient whose ascending aortogram showed an ascending aortic aneurysm.
Established linear methods for measuring aortic size include reviewing cross-sectional dimensions in the axial plane and double oblique plane. A small study comparing the 2 methods found that at all locations the double oblique plane yielded smaller differences with planimetry than the axial plane and differed with the axial plane in proportion to aortic geometric obliquity. [13]
On MDCT, a thoracic aortic aneurysm is unstable if it shows rapid enlargement and/or the following signs of impending rupture [8] :
-
Size increases, especially with a rapid enlargement rate (>10 mm year−1)
-
Focal discontinuity of the intimal wall calcification (missing calcium sign), especially if the patient lumen tapers toward the focal discontinuity (tangential calcium sign)
-
Eccentric shape of the aortic lumen
-
Hyperattenuating crescent rim sign or “crescent sign” seen on unenhanced MDCT as a localized, usually curvilinear, zone with higher attenuation in the thrombus, caused by fresh blood that first insinuates itself into the mural thrombus and later penetrates the aortic wall
-
Thrombus fissuration (ie, penetration of bleeding through longitudinal, transverse, or oblique fissures, which directly communicates with the lumen and represents fissures or dissections between layers of the intraluminal low-attenuating thrombus with increasing wall tension)
-
Draped aorta sign (unidentifiable posterior aortic wall and the posterior aorta conforming to the contours of the neighboring vertebral body)
-
Periaortic stranding.
The detection of the findings above indicates the need for urgent treatment (early surgery or TEVAR). Patients with contained rupture should be managed with permissive hypotension to prevent a free rupture and maintain stability. [8]
Magnetic Resonance Imaging
MRI and CT scanning are the modalities most frequently used for diagnosing and monitoring thoracic aortic diseases. [5, 6] A number of reports attest to the effectiveness of MRI for the evaluation of both true and false aortic aneurysms. Velocity-encoded cine MRI provides a measurement of the differential flow velocity in the true and false channels. By using multiple images per cardiac cycle, a velocity-time curve may be generated to display the disparate flow pattern in the 2 channels.
Because MRI and MRA are noninvasive and provide images along both the short and long axes of the thoracic aorta, they are the preferred method for the follow-up of patients with thoracic aortic diseases. MRA in the sagittal plane is effective for depicting the origins of the arch branches and visceral arteries of the abdominal aorta and their relationship to the aneurysm.
MRI and MRA are used to monitor the maximum diameter and extent of the thoracic aortic aneurysm. A maximum diameter exceeding 6 cm indicates the need for surgical repair. Regular monitoring is important for patients with Marfan syndrome and other conditions associated with progressive aortic dilatation.
Velocity-encoded cine MRI may be used to quantify the volume of concomitant aortic regurgitation in patients with aortoannular abnormalities.
Gadolinium-containing contrast material administered by IV may be valuable in the full eveluation of aortic pathology. However, gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). For more information, see the eMedicine topic Nephrogenic Systemic Fibrosis. The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness. For more information, see the FDA Public Health Advisory or Medscape.
Ultrasonography
Transesophageal echocardiography (TEE) provides an assessment of cardiac structure and function and is highly sensitive in the diagnosis of aortic pathologies. [14, 15, 16, 17] The accuracy of TEE in imaging intimal membranes for signs of aortic dissection has been reported to be 90%.
TEE is reliable for surveys of the following:
-
Aortic valve disease
-
Aortic dilatation
-
Ascending aortic aneurysm
-
Aortic dissection
-
Thrombi
-
Atherosclerotic disease
-
Mitral valve disease
Intraoperatively, TEE may be used to monitor cardiac function; detect atherosclerosis in the thoracic aorta; establish the competency of the aortic valve before surgery; and lower the incidence of stroke, by enabling surgeons to better navigate the placement of clamps and to avoid loosening any atherosclerotic plaques, which could otherwise cause brain embolism.
TEE poorly depicts aneurysms below the diaphragm and in the transverse aortic arch. In addition, this modality requires a skilled cardiologist to interpret the study data, because a high rate of false-positive results has been observed with those who are unfamiliar with the diagnostic limitations of TEE.
Angiography
The findings of aortic dissection seen at angiography include the following: (1) filling of a false channel with or without an intervening intimal flap, (2) distortion of the true lumen by either a patent or a thrombosed false lumen, (3) thickening of the aortic wall by more than 0.5 cm from a thrombosed false lumen, and (4) displaced intimal calcification.
Aortography is accurate for determining the site of the intimal tear and the extent of the dissection (see the first image below). Aortic regurgitation is also easily demonstrated with aortography; this modality demonstrates the extent and location of dissection into aortic side branches.
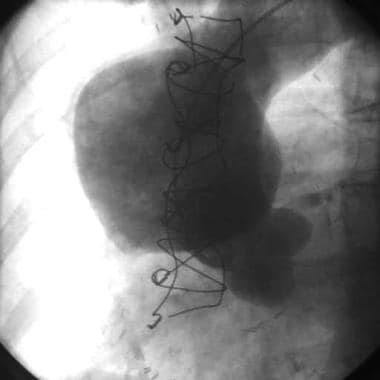 Ascending aortogram showing ascending aortic aneurysm. The patient also underwent computed tomography scanning.
Ascending aortogram showing ascending aortic aneurysm. The patient also underwent computed tomography scanning.
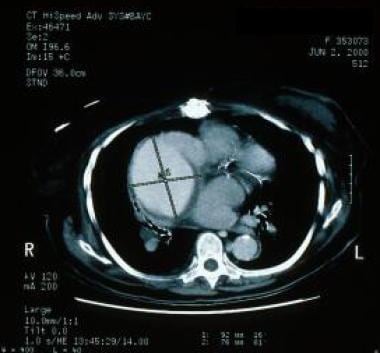 Computed tomography scan from a patient whose ascending aortogram showed an ascending aortic aneurysm.
Computed tomography scan from a patient whose ascending aortogram showed an ascending aortic aneurysm.
Generally, patients electively undergo aortography. It is used in the assessment of operative risks and in deciding on possible modifications of operative technique. The aortogram depicts aortic root dilatation and clearly defines the geography of the aorta and the condition of the smaller vessels. Absolute indications for aortography include renovascular hypertension, intermittent claudication, atherosclerotic occlusive abdominal aorta, and symptoms of carotid stenosis.
Cardiac catheterization may be required to evaluate any concomitant atherosclerotic occlusive disease of the coronary arteries, which may be corrected before or at the same time as the aortic aneurysm. [18]
Aortography is highly specific, but it is an invasive procedure and increases the risk of renal failure because of the use of radiopaque dyes.
-
Chest radiograph showing widening of the superior mediastinum.
-
Computed tomography scan depicting a descending thoracic aortic aneurysm with mural thrombus at the level of the left atrium.
-
Ascending aortogram showing ascending aortic aneurysm. The patient also underwent computed tomography scanning.
-
Computed tomography scan from a patient whose ascending aortogram showed an ascending aortic aneurysm.
-
Chest radiograph in a patient with a thoracic aortic aneurysm following aneurysm surgery.