Practice Essentials
Temporal bone trauma usually is the sequela of blunt head injury. Damage to the temporal bone typically requires the application of great force and may cause fracture, hemorrhage, nerve trauma, vascular damage, or disruption of the middle or inner ear structures. Associated intracranial injuries, such as extra-axial hemorrhage, shear (or diffuse axonal) injury, and brain contusion, are common. [1] Temporal bone fractures classically are described with reference to the long axis of the petrous bone, being classified as either longitudinal (parallel to the axis) or transverse (perpendicular to the axis). Many temporal bone fractures, however, are oblique. The 3 types of fractures (longitudinal, transverse, mixed) are demonstrated in the images below. A newer fracture classification system is based on involvement of the otic capsule, which identifies fractures as otis capsule sparing (OCS) and otis capsule violating (OCV). [2, 3, 4, 5]
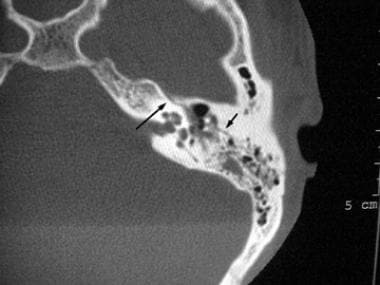
 Axial noncontrast CT scan with bone windows demonstrates a complex fracture with a transverse component (arrow) and an oblique component (arrowhead).
Axial noncontrast CT scan with bone windows demonstrates a complex fracture with a transverse component (arrow) and an oblique component (arrowhead).
Potential complications of temporal bone fracture include infection (meningitis), hearing loss, facial (and other cranial) nerve injury, cerebrospinal fluid (CSF) leak/otorrhea, and perilymphatic fistula. [6] Early identification of temporal bone trauma is essential to managing the injury and avoiding complications.
Historically, temporal bone fractures were diagnosed clinically, with imaging playing a minor role in initial evaluation. However, with the advent of computed tomography (CT) scanning, which offered high-contrast images with spatial resolution, detailed scans of fractures and their complications could be produced.
Imaging modalities
Patient evaluation should begin with a CT scan of the temporal bone. The imaging modality of choice for accurate detection of fracture lines is multidetector CT (MDCT) with multiplanar reconstruction at a section thickness of 1 mm or less. In addition, most patients should undergo a CT head scan for possible associated intracranial injuries. [7, 8, 9, 10, 11] Although CT scanning may be appropriate for assessing complications, magnetic resonance imaging (MRI) is useful for identifying vestibular hemorrhage, determining the extent of brainstem injury, and demonstrating nerve compression. [12, 13]
It is difficult to visualize fracture lines on MRI because of low signal intensity. However, fluid is well demonstrated and contrasts with air and bone. Subtle hemorrhage may be more conspicuous on fluid-attenuated inversion recovery (FLAIR) than on T1-weighted images. [5]
A study by Dempewolf et al noted that in patients with blunt temporal bone trauma, judicious use of a combination of helical CT–scan and physical exam findings during workup can be useful when no maxillofacial CT scans are indicated. Even so, the authors found that only in a relatively small number of patients did temporal bone CT scanning lead to changes in acute patient management; in these cases, the change involved additional workup of a possible vascular injury. [14]
A retrospective study by Szczupak et al indicated that in lower-risk patients, trauma pan-scan CT may be adequate to detect whether temporal bone fractures involve critical structures, without the additional use of a dedicated temporal bone CT scan. [15]
During radiologic examination, select, if possible, scan angles that avoid exposure of the patients' orbits to radiation.
Temporal bone CT scans require additional imaging time and patient cooperation, neither of which may be obtainable in the immediate posttraumatic period. CT scans cannot distinguish between CSF and hemorrhage in the middle ear.
MRI may demonstrate fluid (high signal on T2-weighted images) in the middle ear and mastoid air cells. T1-weighted images may reveal a bright signal in the labyrinth or middle ear, consistent with hemorrhage. However, with regard to depicting temporal bone fractures, MRI has poor sensitivity and specificity.
Plain film radiographs of the skull may show opacified mastoid air cells, intracranial air, or, rarely, a lucency (fracture line). Generally, diagnosis of temporal bone fracture by plain film radiographs is difficult and requires confirmation by CT scanning. The false-negative rate for plain film radiographs is high.
Nuclear medicine studies are not a factor in the diagnosis of acute trauma. However, nuclear cisternography may be used as an adjunct to CT scanning in the diagnosis of a persistent, trauma-related CSF leak. In this setting, nuclear cisternography is a sensitive means of confirming the CSF leak but is not accurate in depicting the location.
Longitudinal fractures
Longitudinal fractures typically result from trauma to the temporal or parietal region and commonly involve fractures of the temporal squamosa or parietal bone. The line of force runs roughly from lateral to medial. A fracture line may extend through the facial nerve canal, thereby damaging the facial nerve, designated as cranial nerve (CN) VII. Associated injury, such as transection or intraneural hemorrhage, may cause facial nerve paralysis, as can damage from displaced bone fragments. The fracture may also disrupt the ossicular chain, resulting in conductive hearing loss.
Transverse fractures
Transverse fractures typically result from trauma to the occiput or cranial-cervical junction, with the line of force running roughly anterior to posterior. A fracture passing through the vestibulocochlear apparatus can cause sensorineural hearing loss and equilibrium disorders. Transverse fractures also commonly injure CN VII, because their path often takes them close to the nerve's labyrinthine segment.
Mixed fractures
Oblique (or mixed) fracture patterns, which extend both longitudinally and transversely, are common, and some case series report that these occur more often than do isolated transverse or longitudinal fractures.
Other classifications
Temporal bone fractures can also be grouped according to whether or not they involve the petrous portion of the temporal bone. For instance, some fractures pass through the tympanic (middle ear), squamous, or mastoid portion of the temporal bone, missing the petrous region. Additionally, temporal bone fractures can be categorized according to whether or not they involve the otic capsule. [16, 2, 3, 4, 5]
Computed Tomography
Patient evaluation should begin with a CT scan of the temporal bone. The imaging modality of choice for accurate detection of fracture lines is multidetector CT (MDCT) with multiplanar reconstruction at a section thickness of 1 mm or less. In addition, most patients should undergo a CT head scan for possible associated intracranial injuries. [7, 8, 9, 10, 11] Although CT scanning may be appropriate for assessing complications, magnetic resonance imaging (MRI) is useful for identifying vestibular hemorrhage, determining the extent of brainstem injury, and demonstrating nerve compression. [12, 13]
A thin-section (1-mm) CT scan can demonstrate a lucency through the temporal bone. Involvement of the middle ear, petrous bone, otic capsule, and facial nerve canal are the primary determinants of prognosis. [12, 13]
A longitudinal fracture (shown in the image below) roughly parallels the petrous bone long axis. Involvement of the middle ear, carotid canal, bony labyrinth, and external auditory canal should be noted.
A transverse fracture (seen below) is perpendicular to the petrous bone long axis. Involvement of the inner ear structures and facial nerve course should be noted.
An oblique fracture (shown below) has transverse and longitudinal elements.
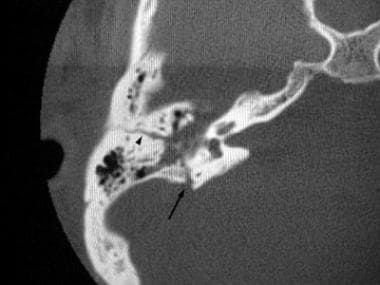 Axial noncontrast CT scan with bone windows demonstrates a complex fracture with a transverse component (arrow) and an oblique component (arrowhead).
Axial noncontrast CT scan with bone windows demonstrates a complex fracture with a transverse component (arrow) and an oblique component (arrowhead).
A study by Ulano et al indicated that in trauma cases in which a temporal bone fracture is not visible on CT scanning, the presence of air around the temporal bone and a finding of mastoid air cell or middle ear cavity opacity should raise suspicions for the presence of fracture. The investigators also found a positive association between complex fracture and pneumocephalus. [17]
There may be false-positive results when normal sutures are misdiagnosed as fracture lines. False negatives may occur with subtle fractures or when suboptimal technique is utilized (as when the study is performed using section thickness >1.25 mm collimation or without employing a bone algorithm).
Angiography
Angiography typically is not a factor in the diagnosis or management of temporal bone fracture; however, when the fracture involves the internal carotid artery canal, damage to the carotid artery may occur. Angiography may reveal a filling defect in the lumen, resulting from intimal flap dissection (linear defect) or thrombosis (irregular or round defect). Alternatively, pseudoaneurysm may be present.
In a retrospective study of the use of angiography for evaluation of temporal bone fractures, Ahmed et al found that mortality was significantly higher in patients with an abnormal CT and no angiogram than it was in patients with an abnormal CT and an abnormal angiogram. The authors concluded that current guidelines for angiography may need to be expanded to include all patients who have CT evidence of neurocranial injury, so as to detect vascular injuries that need aggressive management and thus to lower overall mortality. [18]
-
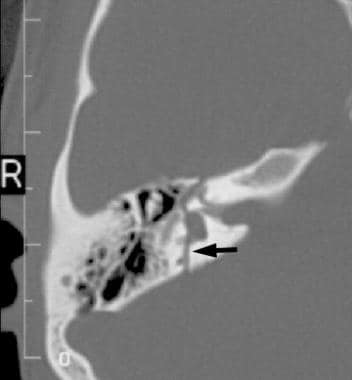
Axial noncontrast CT scan with bone windows reveals a longitudinal temporal bone fracture (arrows).
-
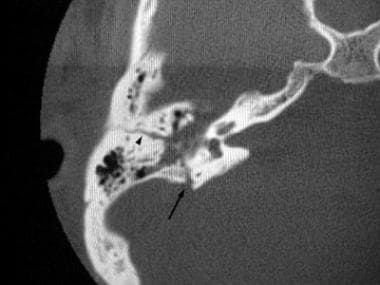
Axial noncontrast CT scan with bone windows reveals a transverse temporal bone fracture (arrow).
-
Axial noncontrast CT scan with bone windows demonstrates a complex fracture with a transverse component (arrow) and an oblique component (arrowhead).