Overview
Suprapubic aspiration and catheterization is a procedure to obtain uncontaminated urine from the urinary bladder. [1] It is easy to perform in the emergency department and is associated with minimal complications. Huze and Beeson first published this practice in 1956 as an alternative to more traditional methods of obtaining urine for analysis and culture. [2] Their findings suggested that suprapubic catheterization and aspiration was superior to clean-catch or transurethral (via catheterization) collection of bladder urine for bacteriologic study.
The sensitivity of the aspirated urine for bacteriuria on urinalysis approaches 100% and is rarely associated with contamination. [3] In a study comparing contamination rates of various urine collection methods for children less than 24 months old, suprapubic catheterization had a contamination rate of 1% compared to 26% for clean-catch and 12% for catheterized specimens. [4] A study by Breinbjerg et al found that for the diagnosis of urinary tract infections in young children, urinary dipstick testing of a sample obtained by suprapubic aspiration had a sensitivity of 78.9% and a specificity of 82.2%, whereas testing of a sample obtained by the midstream clean-catch method had a sensitivity of 94.7% and a specificity of 14.4%. [5]
Relevant Anatomy
The adult bladder is located in the anterior pelvis and is enveloped by extraperitoneal fat and connective tissue. It is separated from the pubic symphysis by an anterior prevesical space known as the retropubic space (of Retzius). The dome of the bladder is covered by peritoneum, and the bladder neck is fixed to neighboring structures by reflections of the pelvic fascia and by the true ligaments of the pelvis. Conversely, the bladder of a child is an abdominal organ and contacts the lower two thirds of the abdominal wall between the symphysis pubis and the umbilicus. The bladder rapidly descends during the first few years of life and then slowly descends until approximately the 9th year of life when it approaches the adult position.
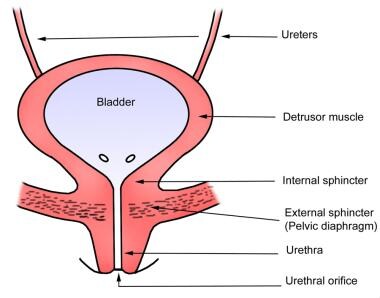
The body of the bladder receives support from the external urethral sphincter muscle and the perineal membrane inferiorly and the obturator internus muscles laterally (see the image below).
For more information about the relevant anatomy, see Bladder Anatomy. See also Female Urinary Organ Anatomy and Male Urinary Organ Anatomy.
Indications
Indications for suprapubic aspiration include the following:
-
Urinary retention (eg, prostate hyperplasia or cancer, gynecologic malignancy, spinal cord injury) [6]
-
Chronic infection of the urethra or periurethral glands
Contraindications
Contraindications to suprapubic aspiration are as follows:
-
Empty or unidentifiable bladder (eg, child’s last urination within 1 hr, nonpalpable bladder in adults)
-
Known bladder tumor
-
Lower abdominal wounds or scarring
-
Overlying cellulitis
Anesthesia
Local anesthesia, in the form of a skin wheal, is placed using lidocaine at the insertion site to reduce discomfort.
The insertion site can be identified beforehand with bedside ultrasonography, if available (see Technique for more details).
For more information, see Local Anesthetics Agents, Infiltrative Administration.
Equipment
Equipment for the procedure includes the following:
-
Sterile gloves
-
Sterile drapes
-
Povidone-iodine (Betadine) skin preparation with sterile gauze
-
Local anesthetic (1% or 2% lidocaine) with syringe and needle
-
Sterile syringe, 10 or 20 mL
-
Needle, 22 gauge (ga), 1.5 in, for pediatric patients
-
Spinal needle, 20 ga, for adult patients
-
Foley catheter tray (catheter size must be at least 1F smaller than the introducer sheath size)
-
Cystostomy kit (eg, Peel-Away Sheath or Rutner cystostomy kit)
-
Sterile urine specimen container
-
Sterile dressing
Positioning
The patient should be supine with the abdomen and pubic areas exposed.
Consider placing the patient in slight Trendelenburg position.
Parents of small children may help hold and calm the child. Otherwise, at least one assistant is needed to immobilize the pediatric patient in a frog-legged position. [12]
Technique
Steps in the procedure are as follows:
-
Localization of the bladder is critical for the procedure. Bedside ultrasonography is remarkably helpful, especially in patients who are obese or contracted. Ultrasonography should be used, if available, even if the bladder is readily palpable. [13]
-
If ultrasonography is unavailable and the bladder is not palpable, the authors advise delaying the procedure.
-
If the bladder is distended, it appears on ultrasound as an anechoic (black) round or ovoid structure just below the abdominal musculature. General landmarks for this site include the midline lower abdomen, which is located approximately 2 cm (or 2 finger breadths) above the symphysis pubis. [14]
-
Sterilize the area with povidone-iodine (Betadine).
-
Palpate the symphysis pubis and inject local anesthetic 2 cm above the superior edge of the symphysis or at the sonogram-determined insertion site. See the image below.
-
Place a small skin wheal of lidocaine at the planned insertion site.
-
For aspiration, select a 22-ga needle for pediatric patients and a 20-ga needle for adults. Choose a needle of appropriate length (eg, shorter for children, longer for adults) and attach it to a 10- or 20-mL syringe.
-
Insert the needle while aspirating until urine appears within the syringe. The insertion approach is slightly different in children and adults. [12]
Pediatric: Insert the needle slightly cephalad, 10-20° off perpendicular, and advance. In a young child, the bladder is still an abdominal organ.
Adult: Insert the needle slightly caudad, 10-20° off perpendicular. In an adult, the bladder is a pelvic organ.
-
If the procedure is performed using ultrasonographic guidance, the bladder appears to tent as the needle pierces its anterior wall. [13] (Of note, the ultrasound transducer should be placed in a sterile probe cover that contains ultrasound gel to maintain a sterile field during the procedure.) See the images below.
-
If the insertion is unsuccessful, do not withdraw the needle fully. Instead, pull back until the needle tip rests in the subcutaneous tissue and then redirect 10° in either direction. Do not attempt more than 3 times. [14]
-
Once urine is obtained, remove the needle and apply gentle pressure at the insertion site with sterile gauze. Place a sterile dressing at the site of insertion.
-
Place the urine specimen in a sterile container approved for urinalysis and culture.
-
If a suprapubic catheter is to be left in place, follow the initial steps above, but use a cystostomy kit. Two common kits are the Cook® Peel-Away Sheath set and the Rutner Suprapubic Catheter set. [15]
-
Cystostomy using Peel-Away Sheath Technique
Once placement is confirmed (urine aspirated), remove the syringe and insert the guidewire from the cystostomy tray through the needle.
Remove the needle using the Seldinger technique and use a scalpel to make a small incision at the insertion site, adjacent to the guidewire.
Thread the peel-away sheath introducer over the guidewire into the bladder and remove the wire.
Insert the Foley catheter through the peel-away sheath introducer. Deploy the Foley catheter balloon with 10 mL of 0.9% saline.
Remove the peel-away sheath introducer from the Foley catheter and pull back on the catheter until resistance is met. Secure the catheter tubing to the abdominal wall with sterile dressing.
The Foley catheter should be attached to a urine meter drainage bag. [13]
-
Cystostomy with Rutner Suprapubic Catheter Technique
- Once placement is confirmed (urine aspirated), remove the syringe.
- Use an 11-blade to make a stab incision at the insertion site.
- Remove the protective sleeve from around the catheter and balloon and place the sharp obturator in the catheter locking it into place with a Luer-lock syringe.
- Advance the balloon catheter 10o caudad from the true vertical aiming toward the pubic symphysis, with one hand at skin level to guide the catheter and one hand on the back of the trocar to stabilize and apply firm steady pressure.
- Advance the catheter until urine is seen (if bladder pressure is low, this step may require aspiration before urine return is noted) and then advance no more than an additional 4-5cm to ensure that the balloon is completely in the bladder.
- Use 10cc sterile water to inflate the catheter balloon, attach the catheter to a drainage bag.
- Alternatively, the catheter may have a stent at the end. In this case advance the suprapubic tube as above into the bladder, apply tension to the accompanying string to engage the curl of the stent, and secure the string to the catheter to affix the stent in place.
-
Secure the indwelling catheter in place using a 2-0 or 3-0 Nylon suture with the suture being tied first with an air knot to the adjacent abdominal wall and then wrapped around the catheter to secure in place. Place dressing over the site.
Pearls
The needle insertion site is approximately 2 cm above the symphysis pubis.
From the true vertical, the needle should be angled 10 º cephalad in children and 10 º caudad in adults.
If available, use bedside ultrasonography to visualize the bladder and observe the needle puncture the bladder wall.
Use a cystostomy kit.
Complications
Complications are rare and include the following:
-
Peritoneal perforation with or without bowel perforation; [16] unlikely to cause significant ramifications unless a catheter is placed
-
Hematuria (usually transient and microscopic, gross hematuria is uncommon)
-
Inability to aspirate urine
-
Palpate the symphysis pubis.
-
Insert the needle while aspirating.
-
Urine appears within the syringe.
-
Gross anatomy of the bladder.